Abstract
Background
Perioperative pain treatment in pediatrics is often insufficient. This study aimed to compare between two different analgesic procedures used for open cholecystectomy in pediatrics with left (LT) to right (RT) shunt.
Methods
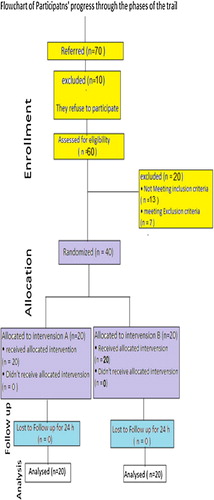
40 patients with age ranging from 2 to 5 years were submitted for elective open cholecystectomy procedures in congenital non-cyanotic heart diseases. After general anesthesia, they were randomized into two groups according to the type of analgesia given, 20 patients in each group. They were either epidural group (group A) or paravertebral group (group B). Hemodynamics including heart rate (HR), mean arterial blood pressure (MAP), and central venous pressure (CVP), were recorded. Pain score, arterial blood gases (ABG), first request for analgesic requirement, and total postoperative consumption of fentanyl (μg/kg) were detected.
Results
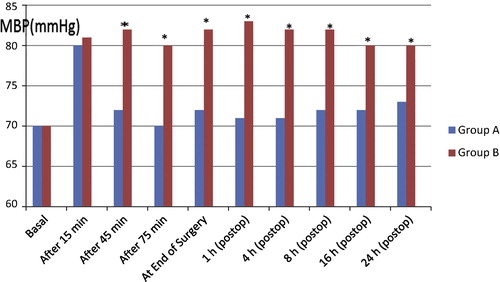
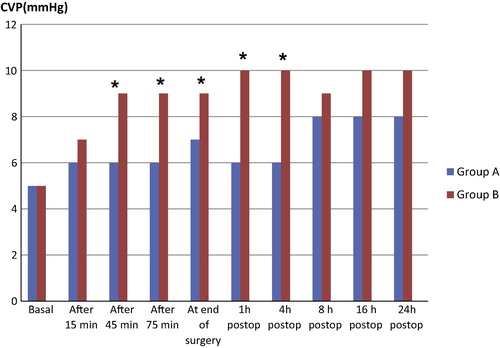
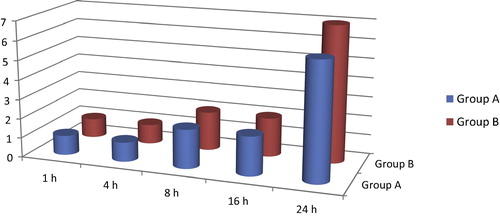
Children’s Hospital Eastern Ontario Pain Scale (CHEOPS) pain score, total fentanyl requirement and the time for first request of analgesic requirement were comparable in both groups. Hemodynamic parameters (HR–MAP–CVP) and the oxygenation parameters in the form of arterial oxygen tension (PaO2) and arterial oxygen saturation (SaO2) were significantly decreased in the epidural group than paravertebral group as P < 0.05.
Conclusion
Both blocks have the same analgesic efficacy but the paravertebral block is superior on epidural block in maintaining hemodynamic stability and improving the oxygenation in pediatrics with a cyanotic heart diseases.
Introduction
Pain following surgery is an universal phenomenon which up to now is often underestimated and undertreated especially in pediatrics. Any postoperative analgesic technique should meet three criteria, which are effectiveness, universal applicability and safety [Citation1].
A cyanotic heart disease, which is a group of congenital heart defects, occurs when shunting (flowing) of blood occurs from the left side of the heart to the right side of the heart due to a structural defect (hole) in the interventricular septum. Patients retain normal levels of ox-hemoglobin saturation in systemic circulation. They include ASD, VSD, PDA and atrioventricular septum defect [Citation2]. The key pathological change is due to the increased pulmonary vascular resistance (PVR) and pressure secondary to increased blood flow from the left to-right shunt. Increasing PVR and pulmonary arterial hypertension (PAH) will lead to reversed direction of blood flow through the cardiac defect (Eisenmenger Syndrome) and heart failure. Cardiac defects with left-to-right shunt generally require surgical or trans-catheter repair at an early age. The balance between pulmonary and systemic circulation will maintain the direction of shunt and any analgesic regimen or block technique will disturb systemic circulation; it will lead to the reversal of shunt [Citation3].
The site of surgery and type of surgery are important factors in determining the degree of pain. Operations involving skin incision without muscle cutting cause a type of pain described as soreness and dull ache, which is very sensitive to low concentration of analgesics, whereas pain following muscle cutting (as occurs in cholecystectomy surgery) is well localized, exaggerated by movement especially deep breathing and coughing and is less responsive to treatment with systemic opioids, so it requires paravertebral or epidural blocks to relieve the pain [Citation4].
Open cholecystectomy with subcostal incision is associated with severe postoperative pain and marked impairment of respiratory function.
Several studies have demonstrated benefits of regional anesthesia in pediatric patients undergoing surgery. Possible regional anesthetic technique for cholecystectomy includes Epidural block, Para-vertebral block, and caudal block [Citation5].
Epidural analgesia is an attractive choice for pediatric surgery. The epidural technique is most commonly used in children either single shot or continuous administration with the usage of many drugs as opioids, local anesthetics, ketamine or α2 agonist as clonidine or dexmedetomidine [Citation6].
Para-vertebral block has undergone a renaissance in last decade. Its use has grown to include breast surgery, renal surgery, cholecystectomy and thoracotomies [Citation7].
The touted benefits in these populations include prolonged and effective analgesia, reduced postoperative nausea and vomiting, with fewer postoperative respiratory complications, shortened recovery, and reduced the stress response to surgical procedures [Citation8].
Despite encouraging results in adult, Para-vertebral block has only recently been described in pediatric patients.
The aim of this study was to compare the analgesic, hemodynamic, and oxygenation parameters of single shot thoracic epidural and single shot thoracic paravertebral block after open cholecystectomy in pediatric patients with left to right shunt.
Patients and methods
This prospective randomized controlled study was conducted from January 2015 to June 2015 at Mansoura Children University Hospital on pediatric patients of ASA II and III who had to undergo elective open cholecystectomy. This study was carried out after approval of the Local Ethical Committee and a written informed consent was obtained from all the parents of patients. It was conducted on 40 patients with age group ranging from 2 to 5 years submitted for open cholecystectomy in non-cyanotic heart diseases. Patients with local sepsis, or with history of anaphylaxis to local anesthetics, coagulation disorders, neurological disorders, were excluded from the study.
In the preoperative visit, all patients included in the study were evaluated by clinical, biochemical and radiological investigations. Patients’ weight and vital signs were noted down. In the preoperative room all patients were premeditated with intramuscular 0.05-mg/kg midazolam and 0.02-mg/kg atropine sulphate 15 min before induction of general anesthesia. Electrocardiographic (ECG), peripheral oxygen saturation (SpO2) and noninvasive blood pressure (NIBP) were monitored. Anesthesia was induced by inhalation of sevoflurane at 8% MAC which decreased gradually down to 2% MAC carried by 100% oxygen, with loss of consciousness; a peripheral intravenous indwelling cannula 22G will be inserted, then the neuromuscular blockade was facilitated by cisatracurium 0.15 mg/kg to allow tracheal intubation with appropriate sized endotracheal tube. Anesthesia was maintained with air and O2 (60:40) and along with 2% sevoflurane to control the depth of anesthesia. This was associated with incremental doses of cisatracurium at 0.1 mg/kg to maintain muscle relaxation. Patients were mechanically ventilated and the end-tidal CO2 was monitored by capnograph. A radial artery catheter was inserted in the non-dominant hand under complete aseptic condition to monitor the arterial blood pressure and blood gases sampling during the entire procedure. A central venous catheter was inserted via the right internal jugular vein under complete aseptic condition for central venous pressure monitoring. A urinary catheter was placed to monitor urine output and nasopharyngeal temperatures were continuously monitored.
The patients were randomized by computer randomization program into one of two groups each one included 20 patients [Citation4].
.1 Group A (Epidural group)
Patient was put in the lateral position; the desired insertion level was determined by ultrasound guidance using a 2–5 MHz curved array probe (Sonosite M-Turbo; Sonosite Inc., Bothell, Washington, USA). The T8–T9 intervertebral level was determined on the basis of the ‘counting-up’ method from the last rib. The probe was oriented in a sagittal direction and placed at the level of the 12th rib in a parasagittal plane 2 cm from the midline. The probe was moved in cephalad direction and the ribs were counted up until the eighth rib was reached. The probe was then directed medially to identify the dura matter at the T8–T9 intervertebral space, and a skin mark was placed to identify the correct level of the block. The block was performed under complete aseptic conditions and after sterilization of the back. The puncture was performed via paramedian approach, at the T8–T9 interspace in all patients, with a 22G needle (B. Braun Melsungen AG). The epidural space was identified by the loss of resistance technique. 0.5 ml/kg of 0.25% bupivacaine and 1 μg/kg fentanyl were injected in the epidural space after giving the test dose.
.2 Group B (Paravertebral group)
Starting with paravertebral space at the T1 level and proceeding caudally to T8 a touchy needle was inserted perpendicular to the skin in an in-plane approach relative to the ultrasound transducer toward the paravertebral space. The needle was advanced under direct vision in a cephalic orientation to puncture the superior costotransverse ligament at the desired level. We used the hydrolocation technique by injecting 0.5–1 ml saline to localize the needle tip and confirm proper placement in paravertebral space by observing anterior displacement of the parietal pleural upon injection. A volume 0.5 ml/kg of 0.25% bupivacaine and 1 μg/kg fentanyl was injected slowly after negative aspiration as a paravertebral block.
In both groups patients were turned supine and ventilation was managed as volume controlled ventilation with the following criteria (TV 8 ml/kg, RR 20 per min I:E ratio 1:2) until the end of surgery as the patients were allowed to take spontaneous respiratory attempts.
At the end of surgery they were reversed with 50 μg/kg neostigmine and 20 μg/kg of atropine and were extubated.
Procedure was considered failed if there was unsatisfactory post-operative analgesia with CHEOPS pain score greater than 4 at the first assessment. These patients were given intravenous narcotics in the form of fentanyl 1 μg/kg to relieve their pain.
Hemodynamics including HR, MAP, CVP, were recorded immediately after the induction of anesthesia, which is considered as basal value, at 15 min after induction of general anesthesia, then every 30 nim till the end of surgery and postoperatively at 1, 4, 8, 16, 24 h.
Pain score was assessed postoperatively at 1, 4, and 8.16, 24 h. For first request for analgesic requirement, total postoperative consumption of fentanyl was calculated.
Oxygenation parameters in the form of O2 tension, O2 saturation and carbon dioxide parameter in the form of CO2 tension were detected intraoperatively at 15 min after induction of general anesthesia then every 30 nim till the end of surgery and postoperatively at 1, 4, 8, 16, 24 h.
We assess the possibility of postoperative complications as nausea, vomiting, pruritus, urine retention and neurological defects.
Statistical method
The power of this clinical trial was retrospectively calculated using G power analysis program version 3 using post-hoc power analysis type II error protection of 0.05 and effect size conversion of 0.8, total sample size of 40 patients 20 patients in each group produced a power of 0.79.
The statistical analysis of data was done by using excel program for figures and statistical Package for social Science (SPSS‘Inc‘Chicago‘IL‘USA) program version 16. To test the normality of data distribution Kolmogorov–Smirnov test was done and only significant data revealed to be nonparametric. Unpaired Student’s t-test was used for between-group comparisons of numerical variables ‘if its assumptions were fulfilled’ otherwise for non-parametric, ‘the Mann–whitney test was used. The statistical analysis and description of data were done in the form of mean (±SD) for quantitative data. Any difference or change showing probability (P) less than 0.05 was considered statistically significant at confidence interval 95% (see ).
able 1 Children’s Hospital Eastern Ontario Pain Scale (CHEOPS) [Citation9]. (Recommended for children 1–7 years old) – A score greater than 4 indicates pain.
Results
The patient’s demographics and duration of surgery had no significant changes in both groups ().
able 2 Patients’ demographics and duration of anesthesia.
This study demonstrated that there was statistical significant decrease in HR and MABP in epidural group compared with paravertebral group at 45 min after performing the block, 75 min until end of surgery intraoperatively and at 1 h, 4 h, 8 h, 16 h and 24 h postoperatively; additionally, CVP showed a significant decrease at 45 min after performing the block, 75 min until end of surgery intraoperatively and at 1 h and 4 h postoperatively ().
Regarding CHEOPS pain score, total fentanyl requirement was 4.66 ± 2.09 μg/kg/24 h in epidural (group A) comparing with 4.93 ± 2.37 μg/kg/24 h in paravertebral (group B) and the time for first analgesic requirement was 18.42 ± 2.04 h in group A compared with 17.30 ± 2.02 h in group B, P > 0.05. So, they were comparable in both groups ( and ).
able 3 The time for first analgesic requirement in hours and total fentanyl requirement μg/kg.
The oxygenation parameter in the form of PaO2 and SaO2 was significantly decreased in the epidural group (group A) than in the paravertebral group (group B) while PaCO2 significantly increased in epidural group than in paravertebral group at 45 min after induction then through the surgery and in 1 h, 4 h, 8 h, 16 h postoperatively ().
able 4 Oxygenation parameters and carbon dioxide parameters in two studied groups.
Only 2 cases (10%) in the epidural group developed pruritus and one case (5%) had nausea and vomiting.
Discussion
The results of this study demonstrated that thoracic paravertebral analgesia and epidural analgesia provide comparable pain relief after open cholecystectomy, but paravertebral analgesia has more hemodynamic stability and a better side effect profile.
Many years ago pain treatment in Infant and children was of doubtful quality and effectiveness. During the last decade pain treatment in them has been improved by knowledge derived from studies on pain and stress [Citation10]. Safe effective analgesia for pediatrics undergoing major surgery remains a challenge particularly in institution where resources are limited.
Open cholecystectomy frequently causes severe postoperative pain and significant morbidity. Atelectasis and emergency intensive care admission have all been found to be related to poor analgesia and consequent immobility. Postoperative pain is thought to be the single most important factor leading to ineffective ventilation and impaired secretion clearance after Cholecystectomy.
Effective postoperative analgesia is believed to reduce morbidity, quicken recovery, improve patient outcome and reduce hospital costs. Thoracic epidural analgesia is commonly used after cholecystectomy and upper abdominal surgery. However, there are risks associated with the technique such as dural puncture, neurological injury and paraplegia. Occasionally, the epidural technique fails as a result of difficult anatomy or poor technique and is contra-indicated in sepsis, coagulation disorders, pre-existing neurological diseases, and difficult thoracic vertebral anatomy [Citation11]. In these situations, PVB offers an attractive alternative that has few contraindications [Citation12].
This study showed a statistically significant decrease in the HR and MAP in epidural group than in the paravertebral group at all times intraoperative and postoperative periods, this is in agreement with Tarek Sarhan who had a study on 24 neonates, and they were randomly allocated into two groups after general anesthesia, Group I had a single shot unilateral thoracic paravertebral block with 1 ml/kg body weight of ropivacaine 0.375% and Group II had thoracic epidural block with 1 ml/kg body weight of 0.375% ropivacaine [Citation13].
Also these results are in accordance with those of Davis et al. during their systemic review and meta analysis comparative study of analgesic efficacy and side effects of paravertebral and epidural block for thoracotomy [Citation14].
This can be explained by the fact that epidural analgesia induces bilateral somatic and sympathetic nerve block, whereas thoracic paravertebral block is the technique of injecting local anesthetic adjacent to the thoracic vertebrae close to where the spinal nerves emerge from the intervertebral foramina. This results in ipsilateral somatic and sympathetic nerve blockade in multiple contagious thoracic dermatomes above and below the site of injection [Citation6].
On the other hand, the significant decrease in the HR and MAP in epidural group leads to a significant decrease in systemic vascular resistance with subsequent reversal of shunt from left to right to become right to left with shunting of venous blood to arterial side. This explains the statistically significant decrease of PaO2 and SaO2 with increasing the degree of cyanosis in epidural group than in PVB group [Citation15]. These findings are in parallel with Kaya and his associates who reported that the neuraxial block in the form of spinal or epidural block in these patients leads to a decrease in systemic vascular resistance (SVR). Thus, in patients with intracardiac shunting, this decrease in SVR results in an increase in right-to-left shunting and a decrease in the ratio of pulmonary to systemic blood flow, which may lead to arterial desaturation, where a patient may develop a reversed direction of shunting (Eisenmenger Syndrome) from left-to-right shun t resulted in decreased left-to-right flow and increased right-to-left flow; the pulmonary to systemic flow ratio significantly decreased [Citation2].
This research proved that CHEOPS score and total fentanyl requirement were comparable in both groups which reflect the equianalgesic efficacy of both blocks for analgesia of cholecystectomy, and these findings are consistent with Cucu and his colleagues who made a study on fifty patients who were randomized to be given either epidural (Group I) or paravertebral (Group II) blocks. All patients received a bolus dose of % 0.25 bupivacaine 10 ml before wound closure and an infusion of %0.25 bupivacaine 0.1 ml/hr was started immediately upon arrival to surgical intensive care unit. All subjects were allowed to take supplementary doses of morphine. Patients were asked to assess the pain at rest, using visual analog scale (VAS) starting from 1 h after arrival in the ICU and every 2 h for the first 24 h. They found that there were no significant differences between the groups with respect to VAS score and morphine consumption [Citation16]. Additionally these results are in agreement with the results of the study done by Matthews and Govenden and Richardson and co-workers [Citation17,Citation18].
On the other hand Bigler and his colleagues compared epidural morphine and bupivacaine combination with paravertebral bupivacaine in patients undergoing cholecystectomy. They found better pain scores in epidural group due to additional use of morphine but no difference in pulmonary function [Citation19].
Tarek Sarhan, Adrian, Karmakar and their associates proved that neonatal infant pain score (NIPS) less than 4 points up to 150 min postoperatively in the epidural group and up to 210 min in the paravertebral group. This means that longer duration of analgesia in the thoracic paravertebral block than thoracic epidural group. The explanation of longer duration of thoracic paravertebral block than thoracic epidural block may be more vascularity in the epidural space than the paravertebral space which may lead to more absorption of local analgesic drug from the epidural space than the paravertebral space leading to shorter duration in epidural group and longer one in PVB group [Citation13,Citation20,Citation21].
Finally, this research showed some complications that related to the epidural block technique, which is in contrast to Cucu et al. who assumed that neither technique demonstrated pain-related complications. This discrepancy was due to the nature of the drug used where they used bupivacaine 0.25% alone while we used bupivacaine 0.25% and opioids in the form of fentanyl 1 μgl kg [Citation16].
Conclusion
It has been shown from the study that both thoracic epidural block and thoracic paravertebral block provide effective postoperative analgesia following open cholecystectomy. However in paravertebral block complications are much less compared to thoracic epidural block and it is associated with more hemodynamic stability and decreased the incidence of reversal of shunt. Therefore it is a safe and effective technique especially in pediatric patients with Lt to Rt shunt and deserves to be used more widely for postcholecystectomy pain relief.
The main limitations to this study are the small number of patients included as well as the short duration of the study. Further studies with larger sample sizes are required to detect any potential disadvantages or complications associated with these block techniques, especially in patients with concurrent diseases.
Financial support
The authors declare hereby that the study did not receive any form of financial support.
Conflict of interest
No conflict of interest emerged during the implementation of this work. The paper had not been presented at any congress before.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- H.KehletJ.DahlEpidural analgesia and postoperative outcomes–a need for a different approachActa Anaesthesiol Scand52200813111312
- A.D.KayeTyler B.StoutIra W.Pad nosLeft-to-right cardiac shunt: perioperative anesthetic considerationsMiddle East J Anesthesiol2162012793807
- P.A.DavlourosA.A.KaratzaI.XanthopoulouDiagnostic role of plasma BNP levels in neonates with signs of congenital heart diseaseInt J Cardiol147201142
- F.CarliH.KehletG.BaldiniEvidence basis for regional anesthesia in multidisciplinary fast-track surgical care pathwaysReg Anesth Pain Med3620116372
- V.M.BanzS.M.JacobD.InderbitzinImproving outcome after major surgery: pathophysiological considerationsAnesth Analg112201111471155
- S.C.KettnerH.WillschkeP.MarhoferDoes regional anesthesia really improve outcome?Br J Anaesth1072011i90i95
- A.VogtD.S.StiegerC.TheurillatSingle injection thoracic paravertebral block for postoperative pain treatment after thoracoscopic surgeryBr J Anaesth9562005816821
- A.CasatiP.AlessandriniM.NuzziA prospective, randomized, blinded comparison between continuous thoracic paravertebral and epidural infusion of 0.2% ropivacaine after lung resection surgeryEur J Anaesth2320069991004
- B.DalensRegional anaesthesia in childrenAnesth Analg681989654672
- P.MitchellUnderstanding a young child’s painLancet35419991708
- V.SvircevicD.van DijkA.P.NierichMeta-analysis of thoracic epidural anesthesia versus general anesthesia of cardiac surgeryAnesthesiology1142011271282
- M.N.HannaJ.D.MurphyK.KumarC.L.WuRegional techniques and outcome. What is the evidence?Curr Opin Anaesthesiol222009672677
- Tarek M.SarhanAnalgesia for tracheoesophageal fistula repair in neonates: a comparison of single shot thoracic paravertebral block and epidural block with ropivacaineAJAIC842005400402
- R.G.DavisP.S.MylesJ.M.GrahamA: comparison of the analgesic efficacy and side effects paravertebral vs epidural blockade for thoracotomy – a systemic review and meta analysis of randomized trialsBr J Anaesth962006418426
- P.S.RaoDiagnosis and management of acyanotic heart disease: Part II – Left-to-right shunt lesionsIndian J Pediatr7262005503512
- O.CucuP.KaracaY.EncG.CamurComparison of epidural anesthesia and paravertebral nerve block in patients undergoing thoracotomyInt J Anesthesiol1112005
- P.J.MatthewsV.GovendenComparison of continuous paravertebral and extradural infusions of bupivacaine for pain relief after thoracotomyBr J Anaesth621989204205
- J.RichardsonS.SabanathanJ.JonesA prospective randomised comparison of preoperative and continuous balanced epidural or paravertebral bupivacaine on post thoracotomy pain, pulmonary function and stress responsesBr J Anaesth831999387392
- D.BiglerW.DirkesJ.HansenEffects of thoracic paravertebral block with bupivacaine versus combined thoracic epidural block with bupivacaine and morphine on pain and pulmonary function after cholecystectomyActa Anaesthesiol Scadinavica331989561564
- T.AdrianEpidural analgesia for major neonatal surgeryPediatr Anaesth81998479
- M.K.KarmakarP.D.BookerR.FranksBilateral continuous paravertebral block used for postoperative analgesia in an infant having bilateral thoracotomyPaed Anaesth62003469471