Abstract
Study objectives
This study was designed to evaluate how the anesthesiologists in Cairo University Hospitals are adherent in their practice to the latest ASA guidelines for management of difficult airway in order to stand on the current status and establish a basis for improvement.
Methods
This is a survey study included 190 anesthesiologists from the faculty members of Cairo university hospitals. All of them completed the study questionnaire.
Main results
A 77.9% of the responders admitted their use of the ASA Algorithm during their practice. For anticipated difficult airway, 74% would employ regional anesthesia as first choice while 52% and 54% would use Supraglottic airway devices and awake Fiberoptic respectively. For unanticipated failed intubation with adequate mask ventilation, 90% would use a supraglottic airway device as their first choice while 85% and 90% would wake up the patient, perform awake fiberoptic intubation and make an emergency invasive airway access respectively. For failed intubation with difficult/impossible mask ventilation, 87% would use a supraglottic airway device while 51% and 28% would perform needle cricothyroidotomy and percutaneous tracheostomy respectively. Awake fiberoptic intubation and intubation with direct laryngoscope using intravenous induction and succinylcholine were the most frequently used techniques in different clinical scenarios.
Conclusion
The practice of anesthesiologists in Cairo university hospitals is close to the recommendations of the ASA guidelines for management of difficult airway. There is increased skills in fiberoptic bronchoscopes and SGA with increased frequency of difficult airway managements training courses; however, they need to improve their skills in awake fiberoptic intubations technique and they need to be trained on invasive airway management access to close the discrepancy between their theoretical choices in different situations and their actual skills.
Introduction
In the anesthesia practice, failure to maintain a patent airway following the induction of general anesthesia is a major concern for anesthesiologists. For securing the airway, tracheal intubation using direct laryngoscopy remains the method of choice in most cases. However, direct laryngoscopic intubation is difficult in 1–4% and impossible in 0.05–0.35% of patients who have seemingly normal airway [Citation1]. The adverse respiratory outcomes related to difficult airway range from sore throat and various traumatic airway injuries up to brain damage and death [Citation2]. Death and brain damage in claims arising from difficult airway management associated with induction of anesthesia, but not other phases of anesthesia, decreased in 1993–1999 compared with 1985–1992 due to development of additional management strategies for prediction and management of difficult airways [Citation3].
The American Society of Anesthesiologists (ASA) has issued guidelines, “The ASA Algorithm on the Management of the Difficult Airway”, to facilitate the management of the difficult airway [Citation4] with frequents updates, the latest one was in 2013 [Citation5]. Furthermore, a large number of airway devices have been introduced into clinical practice, their role in managing different clinical situations has been studied in plenty of publications in anesthesia literature [Citation6,Citation7], and the airway management sessions and workshops become occupying a prominent position in all national and international anesthesia conferences [Citation8]. The expertise of anesthesiologists with the use of different airway devices and their orientation with recent guidelines of airway managements is another field of research in order to identify the current status to use it as a guide for improvement [Citation9,Citation10].
This is a survey study that was designed to evaluate how the anesthesiologists practicing in Cairo University Hospitals are managing difficult airway clinical situations and how their practice is adherent to the latest ASA guidelines for management of difficult airway in order to stand on the current status and establish a basis for improvement.
The primary outcome was to determine the airway management choices among Cairo University anesthesiologists in the three difficult airway situations presented in the ASA Algorithm for Management of the Difficult Airway. The secondary outcomes were to determine the familiarity and skills of anesthesiologists practicing in Cairo University Hospitals with the use of different airway devices and techniques and to observe how they will manage different difficult airway simulation scenarios.
Methodology
After approval of departmental ethical committee, this survey was applied on the anesthesiologists employed in the Anesthesia department of Cairo university hospitals. The Anesthesia faculty members and anesthesia residents completed their 1st year residency were included in this survey while faculty members who were not actually employed in clinical work at the time of survey either for vacation or for mandate outside Cairo university hospitals, anesthesia residents not completed 12 month practice of their residency and visitor anesthesia residents were excluded from the survey.
All anesthesiologists employed in Cairo University Hospitals were identified officially through the Department of Anesthesia of Cairo University. After excluding members of the exclusion criteria, all legible anesthesiologists were categorized according to their ranks into 5 categories: residents, assistant lecturers, lecturers, assistant professors and professors. (190 anesthesiologists were randomly chosen from all legible participants according to the % of each rank in the total number. The included anesthesiologists were randomized to take numbers from 1 to 190.) The survey questionnaires were numbered from 1 to 190 to facilitate the follow-up and to avoid duplication. Survey questionnaire was mailed by the research candidate to the participating anesthesiologists, and those who did not respond within 2 weeks, were contacted through one of the research observers by telephone to resend the questionnaire either by mail or by hand. The completed questionnaires were collected by the research candidate without the identity of the participant.
The survey questionnaire is formed of questions that were answered either by yes or no, or by choosing from multiple choices with only single answer permitted except the question about age and number of years of practice. The survey questionnaire was composed of 4 sections. The first section was designed to assess the demographic characteristics of the responders including age, gender, category, length of practice, on-call duty, the use of the ASA algorism for difficult airway management and educational course participation in the last 2 years. The second section was designed to assess the familiarity and skills of the responders with different airway devices and techniques as special forms of laryngoscope as (Millar and McCoy), the Supraglottic airway devices as (Classic laryngeal mask airway (LMA), Intubating LMA and AirQ), Combitube, Intubation stylets as (Gum elastic bougie, Ventilating tube exchanger and Lightwand intubation), Local anesthesia of the upper airway, Blind nasal intubation, Fiberoptic intubation (under GA, awake oral fiberoptic intubation or awake nasal fiberoptic intubation), Video-assisted endotracheal intubation, and finally different emergency invasive airway access techniques as (Retrograde intubation, needle Cricothyroidotomy, Percutaneous dilatation tracheostomy, and Surgical tracheostomy). The third section was designed to rank the responders’ first three airway management choices in the three different difficult airway situations presented in the ASA Algorithm for the Management of the Difficult Airway: (1) anticipated difficult airway, (2) unanticipated difficult intubation with adequate mask ventilation, and (3) failed intubation with difficult/impossible mask ventilation. The fourth and last section in this questionnaire has presented five different clinical scenarios for difficult airway (Ludwig’s angina, fracture mandible with lock jaw, severe rheumatoid arthritis, sever post tonsillectomy bleeding, huge goiter with tracheal compression/deviation and caesarean section with anticipated difficult intubation and contraindication for regional anesthesia) and the participant was asked to choose their preferred management technique in each scenario from five available airway management techniques (intubation with direct laryngoscope using intravenous induction and muscle relaxant (succinylcholine), intubation after inhalational induction with spontaneous ventilation, awake blind nasal intubation, awake fiberoptic intubation, intubation with Supraglottic airway device or tracheostomy under local anesthesia).
.1 Statistical methods
The collected data were analyzed using IBM SPSS Statistics for Macintosh, version 22.0 (IBM Corp., Armonk, NY, USA). 169 participants were required to obtain 95% confidence interval. The number was increased to 190 for possible dropouts. Categorical data were compared using Chi-square test among responders according to their ranks, training in the last 2 years and number of years of practice, unless one of the observed or expected values was less than 5, then Fisher’s exact test was used. P value less than 0.05 was considered significant in all analyses.
Results
Over 9 months, 190 anesthesiologists from the faculty members of Cairo university hospitals completed questionnaire, and statistical analysis was done by dividing the responses according to their years of experience (less than 5 years, between 5 and 10 years and more than 10 years).
.1 Section 1
The total number of the responders completed the questionnaire was 190, including 117 (61.6%) males and 73 (38.4%) females with the mean age of 36.1 (8.4) years. The rest of Personal characteristics including training in the last 2 years, on-call duty and the use of the ASA guidelines for difficult airway are presented in . There is a statistically significant increase in male gender in all ranks. There is a significant difference among the ranks of the responders regarding training for airway management within the last 2 years and the on-call duty as the highest percentage was found in the group of residents and assistant lecturer. A 77.9% of the whole responders admitted their use of the ASA Algorithm for Management of the Difficult Airway during their practice and there was no statistically significant difference among the ranks.
able 1 Demographic data.
.2 Section 2
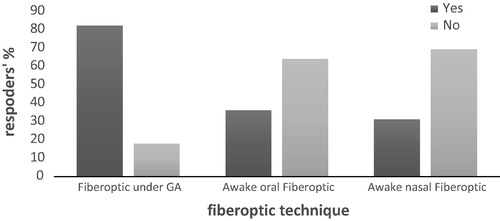
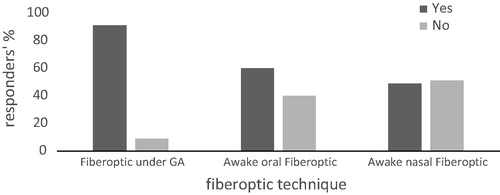
Skills with airway management devices and techniques are presented in . As noted in the survey questionnaire, being skilled with a specific airway device or technique means that the responder has employed the device or performed such technique successfully in his/her practice. A 100% of the responders were skilled with Macintosh laryngoscope and LMA. There is 96% of the responders were skilled with Miller laryngoscope while only 55% were skilled with McCoy laryngoscope with a statistically significant increase in this percentage toward the group with more than 10 years of experience. Responders who were skilled with fiberoptic intubation under general anesthesia were 82% while only 36% and 31% were skilled with awake oral and awake nasal fiberoptic intubation respectively. The statistically significant increase in these percentages was toward the group with more than 10 years of experience. Regarding the invasive airway techniques, only 12% were skilled with retrograde intubation and needle cricothyroidotomy and responders who were skilled with percutaneous and surgical tracheostomy were only 11% and 12% respectively.
able 2 Airway management devices and skills.
.3 Section 3
The choices for airway management in the three proposed difficult airway situations are presented in . For anticipated difficult airway, 74% would employ regional anesthesia if suitable and 52% would use a Supraglottic airway device while 54% would perform awake Fiberoptic intubation as their third and last choice. For unanticipated failed intubation with adequate mask ventilation, 90% would use a supraglottic airway device as their first choice and 85% would wake up the patient and perform awake fiberoptic intubation as their second choice while 94% would make an emergency invasive airway access as their third and last choice. For failed intubation with difficult/impossible mask ventilation, 87% would use a supraglottic airway device and 51% would perform needle cricothyroidotomy as their second choice while 28% would perform percutaneous tracheostomy as their third choice. In the three situations, there was no statistically significant difference between the choices among the three groups (1–5, 5–10, >10 years) experience (see and ).
able 3 Most common choices of difficult airway management.
.4 Section 4
For a case with fracture mandible with lock jaw, 59% would perform awake fiberoptic intubation while 20% and 14% would perform tracheostomy under local anesthesia and blind nasal intubation respectively. For a case with severe rheumatoid arthritis with sublaxation of the cervical spine, 72% would perform awake fiberoptic intubation. For a case with Severe post tonsillectomy bleeding, 86% would perform intubation with direct laryngoscope using intravenous induction and muscle relaxant (succinylcholine). For a case with huge goiter with tracheal compression/deviation, 53% would perform awake fiberoptic intubation while 36% would perform intubation after inhalational induction with spontaneous ventilation. For a case of caesarean section with anticipated difficult intubation and regional anesthesia is contraindicated, 48% would perform awake fiberoptic intubation while 33% would perform intubation with direct laryngoscope using intravenous induction and muscle relaxant (succinylcholine). From the above choices, awake fiberoptic intubation was the most frequent choice among three of such clinical situations, while intubation with direct laryngoscope using intravenous induction and muscle relaxant (succinylcholine) is an important alternative for difficult airway management situations.
Discussion
The main finding of this survey study is that 78% of the responders acknowledged their orientation and adherence to ASA guidelines in managing different difficult airway scenarios. The results revealed increased orientation and practicing with different airway devices and techniques specially fiberoptic intubation and supraglottic airway devices (SGA). On the other hand, very few percentage (10–12%) of the responders are skilled the invasive airway access as needle cricothyroidotomy, retrograde intubation, percutaneous and surgical tracheostomy. The fiberoptic intubation and intubation with direct laryngoscope using intravenous induction and succinylcholine muscle relaxant are found to be the most preferred techniques in managing several difficult airway situations.
The total number of responders revealed that females represent about 38.4% which is a higher percentage than that found in the United State (20%) [Citation10] and Israel (23%) [Citation11]. 67.4% of the responders have received airway educational courses over the last 2 years compared with 71% in United States [Citation10] and 43% in Israel [Citation11]. This may reflect the new policy of Cairo university hospitals to make airway managements training courses available all through the year, and make them mandatory for all new anesthesia residents.
Despite the huge number of available and newly developed airway devices and techniques, the direct laryngoscopies, SGA devices and fiberoptic bronchoscopy are the most frequent available and used devices among anesthesiologists in Cairo university hospitals as seen in results of the second section. This study also revealed that 81.6% of the responders are skilled in fiberoptic intubation under general anesthesia, and only 35.8% and 31.1% of the responders are skilled in awake oral/nasal fiberoptic intubation respectively. It should be mentioned that the fiberoptic bronchoscopes have been introduced in all operating rooms of Cairo university hospital since 2005, and before this date, there were few known personnel who were skilled in fiberoptic intubation. Nowadays the availability of the device and the frequent airway management training courses led to a notable increase in the proportion of our faculty members who have become familiar and comfortable with these techniques. Two survey studies were conducted in the United States, one by Rosenblatt et al. [Citation12] in 1988 applied on random sample of active ASA members living in the USA, and the other one was by Ezri et al. [Citation10] in 2003 applied on homogeneous population of practicing American anesthesiologists who attended the 1999 ASA annual meeting. In agreement with our study, Rosenblatt et al. [Citation12] found that despite the availability of a large variety of airway devices, most anesthesiologists continue to perform direct laryngoscopy with paralysis or awake FOI for most difficult intubation scenarios; however, and after 4 years from Rosenblatt survey, Ezri et al. [Citation10] mentioned that direct laryngoscopy was no more a frequent management option for difficult airway in their population and there was an increase in number of anesthesiologists using fiberoptic intubation to be 59% compared with 41% in the study of Rosenblatt et al. [Citation12]. Another survey study conducted by Ezri et al. [Citation11] among anesthesiologists practicing in Israel revealed that classic LMA and fiberoptic intubation are the most frequent used techniques for difficult airway management in their population.
This study revealed the responders’ limited skills in invasive airway access as needle cricothyroidotomy and jet ventilation, retrograde intubation and percutaneous and surgical tracheostomy integrated in the ASA algorithm for difficult airway, which raises an issue of the importance of paying attention to such techniques in the future airway management training courses. Unlike our results, Rosenblatt et al. [Citation12] and Ezri et al. [Citation10] revealed the increased number of responders who are skilled in retrograde intubation especially among younger anesthesiologists and those who attended airway workshops.
In this study, 78% of the responders acknowledged their orientation and adherence to the ASA guidelines in managing difficult airway. The third section of this survey revealed that a higher percentage was adherent to ASA algorithm of difficult airway as 90% used SGA device for unanticipated difficult intubation with adequate mask ventilation while waking up patient and performing fiberoptic intubation was the second choice by 85%. In the situation of failed intubation with difficult/impossible mask ventilation (i.e. can’t intubate–can’t ventilate scenarios), the use of SGA devices was the first choice in 87% while the needle cricothyroidotomy was the second choice in 51%. However, such results revealed the increased choice of some skills as awake fiberoptic by 85%, needle cricothyroidotomy by 51% and percutaneous tracheostomy by 28% of responders which are percentages exceeding the actual skills of the responders appeared in the second section which were 35.8%, 12.1% and 10.5% respectively and this denotes the presence of a discrepancy between the responders actual skills and their preferred choice of difficult airway management techniques. Same discrepancy was found in Rosenblatt et al. [Citation12] and Ezri et al. [Citation11].
Another issue was revealed by the results of the third section, in a situation of anticipated difficult intubation, 74% of responders chose regional anesthesia if suitable as their first choice of management, and also regional anesthesia was the first choice in the survey study conducted by Ezri et al. [Citation10] in United States and the survey study conducted by Ezri et al. [Citation11]. This practice should be revised as it is not a solution for anticipated difficult airway situations, because it may convert an elective situation to an emergency one. The ASA guidelines were clear in this issue and they state that regional anesthesia is an acceptable choice in this situation, if the surgery can be discontinued at any point and awake intubation can be performed, if it is necessary.
The fourth section in this study also revealed that the awake fiberoptic and direct laryngoscopy are the most commonly used techniques in many different difficult airway scenarios. The choice of the awake fiberoptic intubation not only reflects the concordance with the ASA guidelines for difficult airway managements, but also reflects the uniform performance of this homogenous population who were chosen by 89% intubation with direct laryngoscopy using intravenous relaxant (succinylcholine) for post tonsillectomy bleeding. As in the third section, this section also emphasizes on the discrepancy between the technique of choice and the actual skill, only 35.6% and 31.1% of our responders reported skill with awake oral and awake nasal fiberoptic intubation respectively, 72% would perform awake fiberoptic intubation for a case with severe rheumatoid arthritis with sublaxation of the cervical spine, 59% would perform awake fiberoptic intubation for a case with fracture mandible with lock jaw, 53% would perform awake fiberoptic intubation for a case with huge goiter with tracheal compression/deviation, 48% would perform awake fiberoptic intubation (and it was the first choice) for a case of caesarean section with anticipated difficult intubation and regional anesthesia is contraindicated.
The ASA guidelines for difficult airway management emphasized that they are just recommendations that assist the anesthesiologists in making decisions, they are not absolute requirements, and they do not guarantee any specific outcome and not intended to replace any local institutional policies. In this study, the ASA guidelines for difficult airway management were used as a guide to measure the performance of our institution especially with absence of local institutional or national guidelines. The results of this study revealed that our practice is so close to the recommendations of the ASA guidelines of difficult airway management, a finding that can be explained by the academic nature of our hospitals in which all residents are mandatory exposed to difficult airway training courses while more senior staff are involved in teaching and research processes that necessitate the orientation with any recent update regarding this field.
Some limitations may be considered in this study. First; to our knowledge, and after searching in different literature, no previous studies assessed the pattern of difficult airway managements among Egyptian anesthesiologists, so no previous data available to be compared to enable us to stand on the extent of change in the pattern of practice of the Egyptian anesthesiologists. Second; the population of this study were limited to Cairo university hospital anesthesiologists that represent a homogenous population which means that the results may not reflect the pattern of practice of all Egyptian anesthesiologists, so further larger nationwide studies will be needed to stand on the current pattern of difficult airway management among Egyptian anesthesiologists and to clarify the aspects need to be improved. Third; this study provides very limited difficult airway scenarios while real clinical practice entails dynamic situations that can rapidly deteriorate, changing management choices accordingly. Forth; we did not assess the recommendations of the responders to improve the difficult airway management practice among Cairo university hospital anesthesiologists which may be used as a guide for future planning.
Conclusion
The results of our study revealed that the practice of anesthesiologists in Cairo university hospitals is close to the recommendations of the ASA guidelines for management of difficult airway. There was an obvious improvement in the skill patterns of Cairo university anesthesiologists due to the availability of fiberoptic bronchoscopes and SGA with increased frequency of difficult airway managements training courses; however, they need to improve their skills in awake fiberoptic intubations technique and they need to be trained on invasive airway management access to close the discrepancy between their theoretical choices in different situations and their actual skills.
Conflict of interest
No conflict of interest in this study.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- J.L.BenumofManagement of difficult adult airway with special emphasis on awake tracheal intubationAnesthesiology75199110871110
- T.CookS.ScottR.MihalLitigation related to airway and respiratory complications of anaesthesia: an analysis of claims against the NHS in England 1995–2007Anaesthesia652010556563
- G.N.PetersonK.B.DominoR.A.CaplanManagement of the difficult airway. A closed claims analysisAnaesthesiology10320053339
- The American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Practice guidelines for management of the difficult airway: a report, vol. 78. Anesthesiology; 1993. p. 597–602.
- Practice Guidelines for Management of the Difficult Airway An Updated Report by the American Society of Anesthesiologists Anesthesiology, vol. 118; 2013; p. 251–70.
- J.B.PaoliniF.DonatiP.DroletReview article: video-laryngoscopy: another tool for difficult intubation or a new paradigm in airway management?Can J Anaesth6022013184191
- M.F.AzizD.DillmanR.FuComparative effectiveness of the C-MAC video laryngoscope versus direct laryngoscopy in the setting of the predicted difficult airwayAnesthesiology11632012629636
- Y.KaminohQuality assurance in airway management: education and training for difficult airway management (abstract)Masui55120063343
- M.S.KristensenJ.MollerAirway management behaviour, experience and knowledge among Danish anaesthesiologists – room for improvementActa Anaesthesiol Scand45200111811185
- T.EzriP.SzmukR.D.WartersDifficult airway management practice patterns among anesthesiologists practicing in the United States: have we made any progress?J Clin Anesth152003418422
- T.EzriS.KonichezkyD.GevaDifficult airway management patterns among attending anaesthetists practising in IsraelEur J Anaesthesiol202003619623
- W.RosenblattP.J.WagnerA.OvassapianPractice patterns in managing the difficult airway by anesthesiologists in the United StatesAnesth Analg871998153157
ppendix A
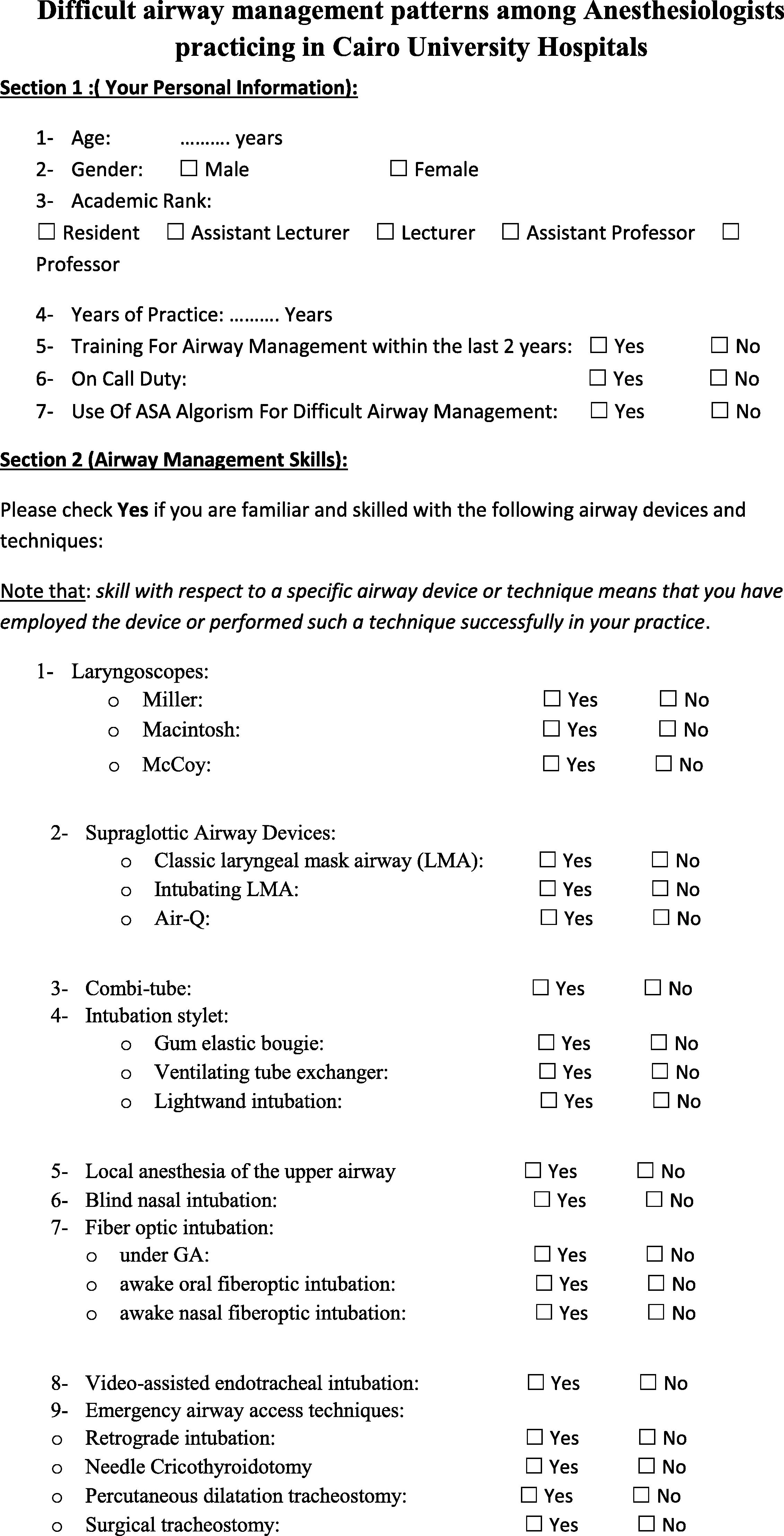
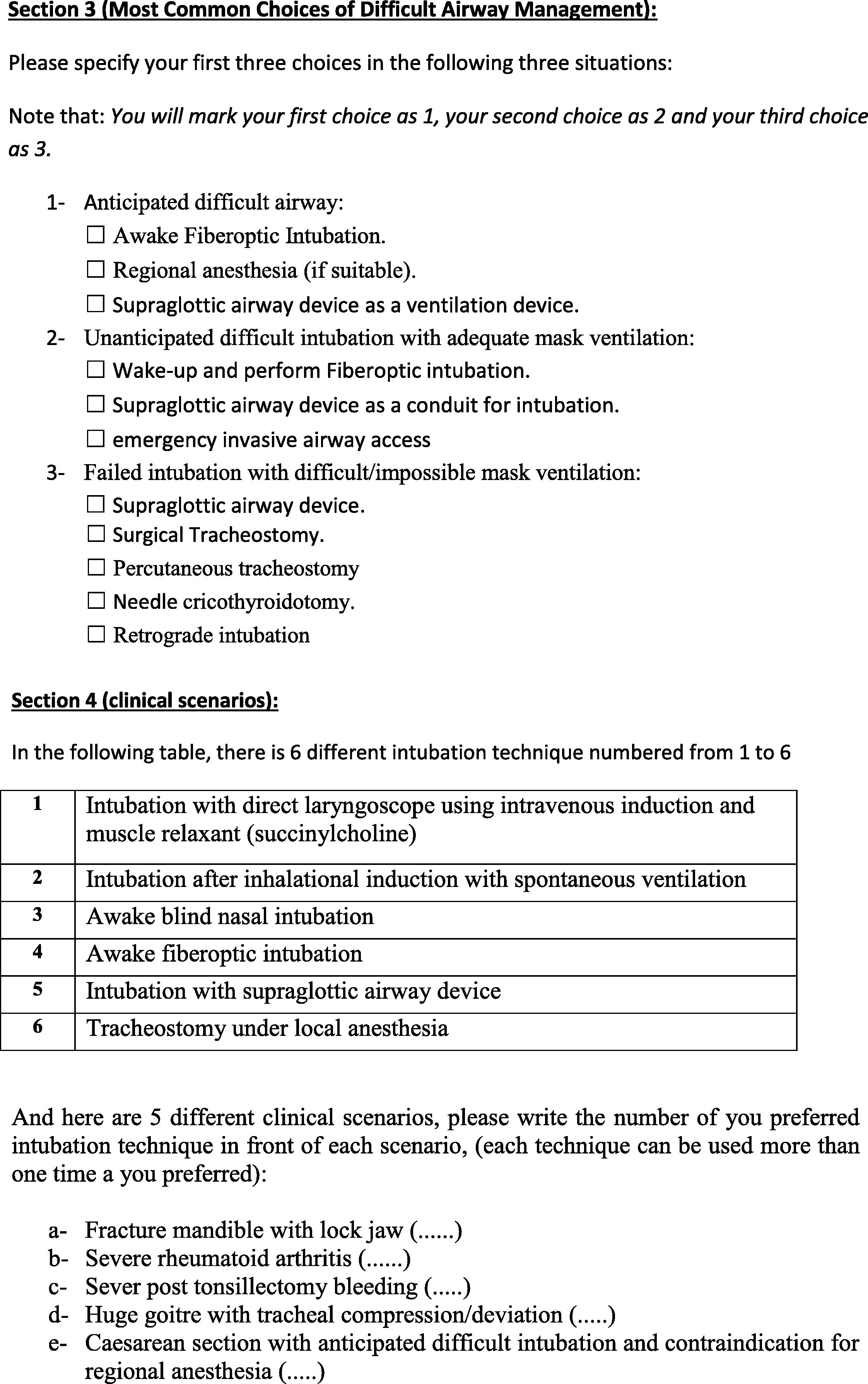
The survey questionnaire