Abstract
Objective
This randomized, double blind, controlled study was designed to test whether the intraoperative use of intravenous lidocaine bolus followed by infusion would attenuate the tourniquet induced hypertension (TIH) in patients undergoing anterior cruciate ligament reconstruction (ACLR) under general anesthesia.
Methods
76 patients were randomly allocated into two equal groups. Lidocaine group (group L), in which patients received lidocaine 2% 1 mg/kg IV bolus after induction of anesthesia followed by lidocaine infusion (2 mg/kg/h) and placebo group (group P), in which patients received equal volumes of saline. Heart rate (HR), systolic blood pressure (SBP) and diastolic blood pressure (DBP) were recorded before induction of anesthesia, before tourniquet inflation (baseline value), every 15 min after tourniquet inflation, and after tourniquet deflation. The number of patients who developed TIH was recorded and total amount of propofol and fentanyl used intraoperative was recorded.
Results
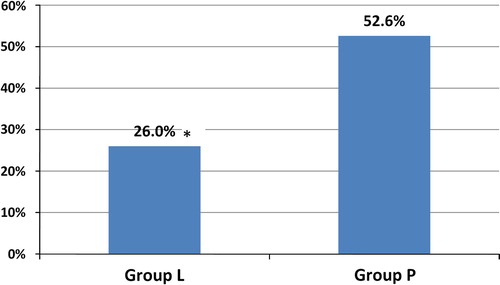
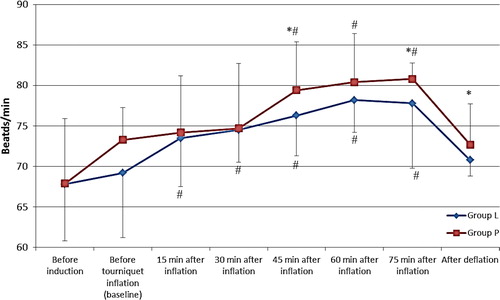
SBP, DBP and HR were significantly less after tourniquet inflation in group L compared to group P in most of the time periods after tourniquet inflation (p value < 0.05), the number of patients developed TIH was significantly less in group L compared to group P (26% in group L compared to 52.6% in group P) (p value 0.019), and the total amount of propofol and fentanyl used intraoperative was significantly less in group L compared to group P (p value 0.000).
Conclusion
Intraoperative use of lidocaine bolus (1 mg/kg), followed by infusion (2 mg/kg/h), started 10 min before tourniquet inflation attenuated the TIH in patients undergoing anterior cruciate ligament reconstruction under general anesthesia.
Introduction
Arterial tourniquet is used in limb surgeries to provide a bloodless field and improve the surgical conditions. However, tourniquet inflation is associated with some consequences that may be relatively benign in healthy individuals, but could be hazardous in patients with impaired cardiac conditions [Citation1]. Tourniquet inflation is associated with an increased sympathetic outflow, an increase in arterial blood pressure and severe pain [Citation2–Citation4].
The tourniquet induced hypertension (TIH) is usually delayed 30–60 min after tourniquet inflation [Citation5], and it is difficult to treat even with adequate analgesia and good level of anesthesia [Citation6,Citation7]. Although the proper mechanism of (TIH) is still unclear [Citation7], the autonomic nervous system is probably involved and plasma catecholamine levels are increased [Citation2]. Also, stimulation of N-methyl-D-Aspartate (NMDA) receptors by noxious stimuli from the extremities is another possible cause leading to TIH [Citation8,Citation9]. There are several studies done using different analgesics and NMDA receptor antagonists to find an effective drug to attenuate (TIH) [Citation6–Citation8,Citation5].
Intravenous lidocaine is known as having anti-inflammatory [Citation10,Citation11], analgesic [Citation10], anti-hyperalgesic [Citation12] properties and is used for attenuating stress response to laryngoscopy and intubation [Citation13]. To our knowledge, no previous studies tested the effect of intraoperative lidocaine infusion on TIH.
We designed this randomized, double blind, placebo controlled study to test whether the intraoperative use of intravenous lidocaine infusion would attenuate the TIH in patients undergoing anterior cruciate ligament reconstruction under general anesthesia as a primary outcome.
Materials and methods
After obtaining ethical committee approval, written informed consents were taken from 76 patients, American Society of Anesthesiology (ASA) physical status I or II, their age range between 18 and 50 years, who were scheduled for anterior cruciate ligament reconstruction under general anesthesia with the use of pneumatic tourniquet.
The study was carried out at Saad Specialist Hospital, Alkhobar, Saudi Arabia, during the period from January 2014 to June 2015. Exclusion criteria included patients with sickle cell disease, peripheral vascular disease, hypertension, history of DVT, cardiac, liver or kidney diseases, allergy to amide local anesthetics and seizure disorder. Patients weighing more than 100 kg and patients in whom tourniquet time was less than 60 min were also excluded.
Patients were randomly allocated into two equal groups (37 patients each) by using the closed envelope technique. The study drugs were prepared by an anesthesia technician unaware of the study medications; as follows:
| #x2022; | Lidocaine group (group L): patients received lidocaine 2% 1 mg/kg IV bolus after induction of anesthesia followed by lidocaine infusion (2 mg/kg/h) diluted in 50 ml syringe with a maximum of 200 mg/h. The tourniquet was inflated 10 min after the start of lidocaine infusion. The lidocaine infusion stopped at the time of tourniquet deflation. | ||||
| #x2022; | Placebo group (group P): equal volumes of saline. | ||||
Anesthesiologists, surgeons and patients were all blinded to the treatment allocation. The lidocaine and placebo syringes were identical and labeled as test medication. Anesthesiologist who gave anesthesia was instructed not to use local anesthetics.
Depending on previous studies [Citation5,Citation7], the sample size was estimated to be 38 patients per group, to give a power of 80% at the level of 0.05 to detect 6.5% difference in the percentage increase of baseline arterial blood pressure after 60 min of tourniquet inflation.
All patients were pre-medicated with midazolam 0.03 mg/kg intravenously 5 min before induction of anesthesia. In the operating room intravenous infusion of Ringer’s lactate 10 ml/kg started and monitors were attached to the patient [ECG, pulse oximeter, non-invasive blood pressure, capnography, temperature probe and bispectral index (BIS)]. Anesthesia was induced using fentanyl 2 μg/kg IV, propofol 2 mg/kg IV and cisatracurium 0.15 mg/kg IV to facilitate tracheal intubation. Mechanical ventilation was adjusted to maintain end tidal CO2 between 35 and 40 mmHg. Anesthesia was maintained by using propofol infusion (5–10 mg/kg/h), starting with (10 mg/kg/h) and then adjusted to maintain the BIS between 40 and 60. Additional doses of fentanyl (50–100 μg) were given if there were signs of inadequate analgesia (BP and HR within 20% of pre-induction values). Cisatracurium boluses of 0.03 mg/kg were guided by peripheral nerve stimulator to maintain muscle relaxation.
If the BP or HR increased >30% of the baseline value before tourniquet inflation, labetalol boluses of 5 mg were given to control the hemodynamic changes.
The pneumatic tourniquet (20 cm width) was applied over cotton layer to the upper thigh (operation side), the limb was elevated 45 degrees for 5 min, exsanguination was done using crepe bandage and the tourniquet was inflated to 300 mmHg. The tourniquet was deflated at the end of the operation and all anesthetics were discontinued.
Patients were extubated after reversal of neuromuscular blockade using neostigmine 0.05 mg/kg and atropine 0.02 mg/kg IV and shifted to the post-anesthesia care unit (PACU). The following parameters were recorded by an anesthesiologist unaware of study drugs:
| . | Hemodynamic including HR, SBP and DBP (measured every 5 min) were recorded at the following time: before induction of anesthesia, before tourniquet inflation (baseline value), every 15 min after tourniquet inflation, and 15 min after tourniquet deflation. | ||||
| . | The number of patients who developed TIH which was defined by an increase in arterial blood pressure >30% of the baseline value (number of patients received labetalol). | ||||
| . | Total dose of fentanyl needed intraoperative. | ||||
| . | Total dose of propofol used intraoperatively. | ||||
| . | Tourniquet time. | ||||
| . | Duration of operation. | ||||
.1 The statistical analysis
Data were statistically described in terms of mean ± standard deviation (±SD), or frequencies (number of cases) and percentages when appropriate. Comparison of numerical variables between the study groups was done using Student’s t test for independent samples while comparing variables over time was done using repeated measure analysis of variance with paired t test as post hoc multiple pairwise comparisons. For comparing categorical data, Chi square (χ2) test was performed. Exact test was used instead when the expected frequency is less than 5. p values less than 0.05 were considered statistically significant. All statistical calculations were done using computer program SPSS (Statistical Package for the Social Science; SPSS Inc., Chicago, IL, USA) release 15 for Microsoft Windows (2006).
Results
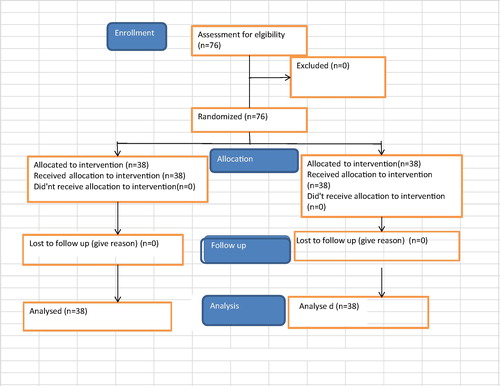
All patients completed the study ().
Patients in both groups were comparable as regards demographic data, tourniquet time and duration of operation (p value > 0.05), (). The total amount of fentanyl used in group L was significantly less than that in group P (p value 0.000), and the total amount of propofol used was also significantly less in group L than in group P (p value 0.000) (). The number of patients having TIH was significantly less in group L compared to group P (p value 0.019) (, ).
able 1 Demographic data, operation time, total amount of fentanyl and propofol and number of patients having TIH.
shows the changes in mean and SD in SBP between both groups during the study period, the mean SBP was significantly less after tourniquet inflation in the L group in comparison with P group at 30, 45, 60 and 75 min P value < 0.05, and also there was a significant difference in the values of SBP after tourniquet inflation in group P in most of the points and its baseline value, p value < 0.05.
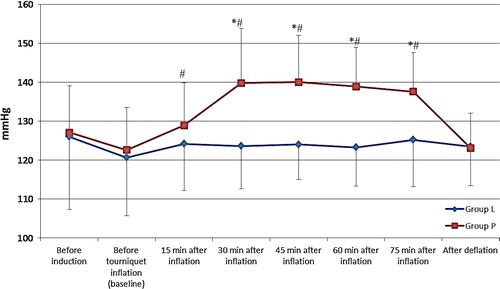
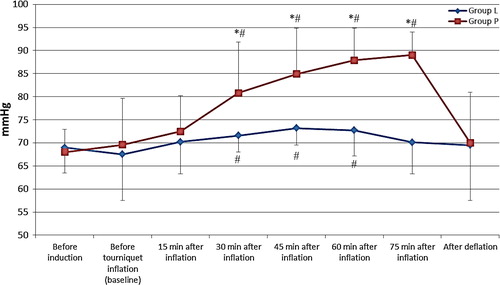
shows the mean DBP in both groups, DBP was significantly less after tourniquet inflation in group L in comparison with group P at 30, 45, 60 and 75 min, p value < 0.05, and there was a significant difference in the values of DBP in both groups and their baseline value in most of the time periods measured after tourniquet inflation.
shows the mean value and SD in heart rate in both groups during the study period, the HR was significantly higher in group P compared to group L at 45, 75 min after tourniquet inflation and also after deflation of tourniquet p value < 0.05, and both groups show significant difference after tourniquet inflation from their baseline value (p value < 0.05).
Discussion
Our study showed that the use of IV lidocaine bolus (1 mg/kg) followed by infusion (2 mg/kg/h), 10 min before tourniquet inflation and continued until tourniquet deflation resulted in attenuation of the increase in blood pressure and heart rate induced by pneumatic tourniquet inflation in patients undergoing anterior cruciate ligament reconstruction under general anesthesia. The incidence of TIH reduced from 52.6% in the placebo group to 26% in the lidocaine group.
Although the mechanism of TIH is still not clear [Citation7], two mechanisms are thought to be involved; the first is activation of C fibers, causing stimulation of NMDA receptors in the dorsal horn of the spinal cord [Citation7], and the second is sympathetic activation [Citation2].
Tetzlaff et al., demonstrated that TIH coincides with the activation of the sympathetic nervous system, as shown by power spectral analysis of heart rate [Citation2]. This theory is supported by the finding that the onset of the TIH coincides with the onset of tourniquet pain as both usually occur 30–60 min after cuff inflation [Citation14]. Heropoulos et al., reported an increase in the plasma levels of catecholamines associated with TIH under general anesthesia [Citation15]. And, Zalunardo et al., showed that preoperative administration of clonidine suppressed the cardiovascular and hyperadrenergic response resulted from tourniquet inflation [Citation16].
The other hypothesis suggested that tourniquet pain is mediated by unmyelinated, slow-conducting C fibers – which are normally inhibited by fast pain impulses conducted by myelinated A-δ fibers – [Citation17,Citation18]. Mechanical compression caused by tourniquet inflation leads to loss of conduction in the large A-δ fibers, leaving still functioning C fibers uninhibited, that causes activation of NMDA receptors in the dorsal horn of the spinal cord [Citation7].
IV lidocaine injection blunts the sympathetic response in many studies by attenuating the increase in BP, HR and catecholamine release in response to intubation, extubation and surgical stimulation [Citation13,Citation19,Citation20].
The mechanism of analgesic effect of systemic lidocaine is still poorly understood and is unlikely to be explained only on the basis of lidocaine’s Na+ channel blocking effect [Citation21]. Some research has suggested that it could be partly associated with NMDA receptor antagonism by the glycinergic action of lidocaine itself or one of its metabolites [Citation11,Citation21]. Others suggested the inhibition of G-protein-coupled receptors and the inflammatory response possibly can contribute to the analgesia seen with lidocaine infusions [Citation22].
The observed attenuation of TIH by IV lidocaine injection in this study could be explained by the effect of lidocaine on sympathetic response and/or its systemic analgesic effect.
In our study, IV infusion of lidocaine resulted in less propofol and fentanyl consumption, which is consistent with previous studies that showed the sparing effect of systemic lidocaine on anesthetic and opioid requirements and referred this to anti-nociceptive effect of lidocaine [Citation20,Citation23].
The dose of bolus and the rate of infusion of lidocaine used in our study were based on previous studies that proved that this dose did not result in plasma concentration more than 4 mcg/ml, which is below the toxic levels [Citation19,Citation21].
We maintained an adequate level of anesthesia (BIS between 40 and 60) by using propofol infusion, fentanyl boluses to insure adequate analgesia and cisatracurium boluses for muscle relaxation to exclude their inadequacy as factors contributing to intraoperative hypertension and tachycardia.
Limitation in our study, we did not do dose response study to the effect of lidocaine on TIH. Further studies are needed to evaluate whether smaller doses of lidocaine bolus and infusion can achieve the same benefit or whether larger doses can reduce TIH to a greater extent.
Conclusion
Intraoperative use of lidocaine bolus (1 mg/kg), followed by infusion (2 mg/kg/h), started 10 min before tourniquet inflation attenuated the TIH in patients undergoing anterior cruciate ligament reconstruction under general anesthesia.
Conflict of interest
The authors declare that there are no conflict of interests.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- P.C.A.KamR.KavanaughF.F.Y.YoongThe arterial tourniquet: pathophysiological consequences and anaesthetic implicationsAnaesthesia562001534545
- J.E.TetzlaffJ.O’HaraH.J.YoonA.SchubertTourniquet-induced hypertension correlates with autonomic nervous system changes detected by power spectral heart rate analysisJ Clin Anesth91997138142
- H.ValliP.H.RosenbergJ.KyttaM.NurminenArterial hypertension associated with the use of a tourniquet with either general or regional anesthesiaActa Anesthiol Scand311987279283
- P.C.KamR.KavanaughF.F.YoongThe arterial tourniquet; pathphysiological consequences and anesthetic implicationsAnesthesia562001534545
- S.YamashitaH.YamaguchiY.HisajimaK.IjimaK.SaitoA.ChibaPreoperative oral dextromethorphan attenuated tourniquet-induced arterial blood pressure and heart rate increases in knee cruciate ligament reconstruction patients under general anesthesiaAnesth Analg982004994998
- H.C.LaoP.S.TsaiJ.Y.SuT.G.KwokC.J.HuangDexmedetomidine attenuates tourniquet-induced hyperdynamic response in patients undergoing lower limb surgeries: a randomized controlled studyJ Surg Res1792013e99e106
- J.W.ParkY.H.JungC.W.BaekH.KangS.M.ChaEffects of low dose ketamine on tourniquet-induced haemodynamic responses during general anaesthesiaJ Int Med Res3552007600608
- T.SatsumaeH.YamaguchiM.SakaguchiT.YasunagaS.YamashitaS.YamamotoPreoperative small-dose ketamine prevented tourniquet-induced arterial pressure increase in orthopedic patients under general anesthesiaAnesth Analg92200112861289
- C.J.WoolfS.W.ThompsonThe induction and maintenance of central sensitization is dependent on N-methyl-D-aspartic acid receptor activation; implications for the treatment of post-injury pain hypersensitivity statesPain441991293299
- G.R.LaurettiMechanisms of analgesia of intravenous lidocaineRev Bras Anestesiol582008280286
- U.Muth-SelbachH.HermannsJ.U.StegmannK.KolloscheR.FreynhagenI.BauerP.LipfertAntinociceptive effects of systemic lidocaine: involvement of the spinal glycinergic systemEur J Pharmacol61320096873
- W.KoppertN.OstermeierR.SittlC.WeidnerM.SchmelzLow dose lidocaine reduces secondary hyperalgesia by a central mode of actionPain852000217224
- I.G.WilsonB.H.MeiklejohnG.SmithIntravenous lignocaine and sympathoadrenal responses to laryngoscopy and intubation. The effect of varying time of injectionAnaesthesia461991177180
- K.Urban MichealAnaesthesia for orthopaedic surgeryR.D.MillerMiller’s anesthesia2010Churcill Livingstone PublishersPhiladelphia2252
- M.HeropoulosH.SchierenJ.L.SeltzerR.R.BartkowskiM.TorjmanJ.LessinIntraoperative hemodynamic, renin, and catecholamine responses after prophylactic and intraoperative administration of intravenous enalaprilatAnesth Analg801995583590
- M.P.ZalunardoD.SerafinoP.SzelloeF.WeisserA.ZollingerB.SeifertPreoperative clonidine blunts hyperadrenergic and hyperdynamic responses to prolonged tourniquet pressure during general anesthesiaAnesth Analg942002615618
- M.J.GielenR.StienstraTourniquet hypertension and its prevention: a reviewReg Anesth161991191194
- A.J.HodgsonA proposed etiology for tourniquet-induced neuropathiesJ Biomech Engl1161994224227
- Mohamed R.El-TahanOsama M.WardaDouaa G.DiabEyad A.RamzyMohamed K.MatterA randomized study of the effects of perioperative i.v. lidocaine on hemodynamic and hormonal responses for cesarean sectionJ Anesth232009215221
- F.R.AltermattD.A.BugedoA.E.DelfinoS.SolariI.GuerraH.R.MuñozEvaluation of the effect of intravenous lidocaine on propofol requirements during total intravenous anaesthesia as measured by bispectral indexBr J Anaesth1082012979983
- M.SugimotoI.UchidaT.MashimoLocal anaesthetics have different mechanisms and sites of action at the recombinant N-methyl-D-aspartate (NMDA) receptorsBr J Pharmacol1382003876882
- J.CassutoR.SinclairM.BonderovicAnti-inflammatory properties of local anesthetics and their present and potential clinical implicationsActa Anaesthesiol Scand502006265282
- W.KoppertM.WeigandF.NeumannR.SittlJ.SchuettlerM.SchmelzPerioperative intravenous lidocaine has preventive effects on postoperative pain and morphine consumption after major abdominal surgeryAnesth Analg98200410501055