Abstract
Purpose
The purpose of this study was to evaluate the postoperative analgesia and morphine requirements of ultrasound guided rectus sheath catheters versus continuous wound catheters in midline open colorectal surgery patients.
Methods
Sixty patients of both sexes aged 40–65 years were randomized into 2 equal groups to receive postoperative analgesia through either a wound catheter continuous infusion (group I) or rectus sheath catheters (group II). The trial is registered in the Australian New Zealand Clinical Trials Registry: ACTRN12615000636550.
Results
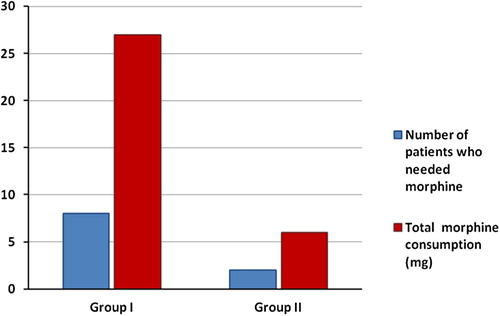
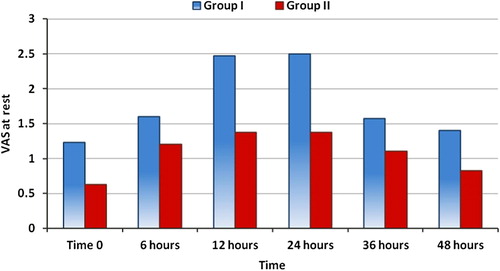
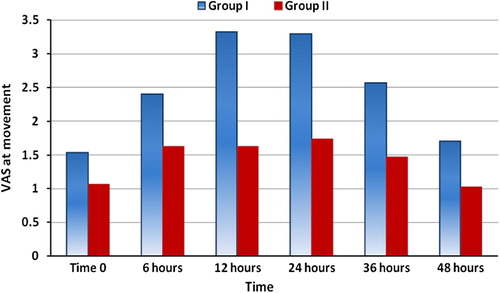
Heart rate and mean arterial blood pressure increased significantly in group I at 12 and 24 h as compared to time 0 and 48 h (P < 0.05). There was a significant increase in heart rate and mean arterial blood pressure in group I as compared to group II at all-time intervals (p < 0.05). There was a significant decrease in Visual analogue score at rest and with movement and in group II as compared to group I at all-time intervals (p < 0.05). Concerning the need for rescue analgesia, 8 patients (26%) in group I required rescue analgesia; 7 patients of them required only one dose and one patient required two doses. In group II two patients (6.6%) required rescue analgesia, and both required one dose. The total morphine consumption was lower and the patient satisfaction was better in group II compared with group I (p = 0.005). There were no serious complications in the two groups.
Conclusion
Ultrasound-guided rectus sheath catheters provided better postoperative analgesia compared with wound catheter continuous infusion for colorectal surgery without undesirable side effects.
Introduction
Extended midline abdominal incisions are associated with severe postoperative pain. Many multimodal analgesia techniques are used to provide effective analgesia for such incisions with the aim of limiting the perioperative use of morphine and its side effects [Citation1].
Wound infiltration (WI) with local anesthetic (LA) inhibits nociceptive impulse transmission from the site of injury thus modulating pain at the peripheral level. The main limitation for use of a single dose is short-term analgesic effect (usually 2–6 h) [Citation2]. Although there are multiple studies evaluating use of continuous wound catheters in different surgical procedures, there are conflicting reports of its efficacy [Citation3–Citation6].
Modified rectus sheath block was first described at the turn of the last century [Citation7], it was infrequently used till long acting local anesthetics agents, and small caliber infusion catheters and a small portable ultrasound machine are recently available [Citation8]. These developments have resulted in renewed interest in rectus sheath catheters for postoperative pain management after midline abdominal incisions [Citation7,Citation9,Citation10]. Ultrasound allows accurate visualization of the position of the needle tip, and placement of catheters to provide continuous postoperative analgesia [Citation10] and reduces the risk of puncture of the posterior rectus sheath, peritoneum and bowel [Citation9].
However, to the best of our knowledge, there is no clinical trial comparing the analgesic effect of both wound catheter continuous infusion and ultrasound guided rectus sheath catheters. So, the aim of the present study was to evaluate the postoperative analgesia and morphine requirements of ultrasound guided rectus sheath catheters versus continuous wound catheters in patients scheduled for open colorectal surgery through midline incision.
Patients and methods
This randomized prospective clinical trial was carried out at the General Surgical department, Tanta University Hospital, from April 2014 to April 2015 on 60 patients of both sexes aged (40–65) years, and ASA physical status class I and II scheduled for elective open colorectal surgery via midline abdominal incision after obtaining an institutional board approval with approval code: 2474/03/14. A written informed consent was obtained from every patient and all the data in the study were confidential; every patient had a secret code and the results were used for scientific purpose only. The trial is registered in the Australian New Zealand Clinical Trials Registry: ACTRN12615000636550.
Patients were excluded from the study if they presented with coagulopathies, impaired platelet functions, cardiovascular instability, cerebral strokes, renal or liver disease. Patients with local infection at the block site or with history of allergy to local anesthetics were also excluded.
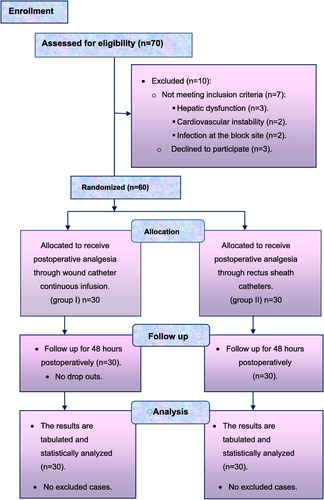
The sample size calculation was found to be N > 27 for each study group based on the following criteria: 95% confidence limit, 80% power of the study, ratio of cases to control is 1:1, expected outcome ranging between 70 and 95%. Preoperatively, 70 patients were assessed for eligibility: of them 10 were excluded; 3 patients refused to participate in the trial and 7 were not meeting the inclusion criteria (3 had hepatic dysfunction, 2 were suffering from cardiovascular instability and 2 had infection at the site of the block). So, 60 patients were randomized preoperatively using closed envelops and computer generated random numbers into 2 equal groups, each of 30 patients to receive postoperative analgesia through either a wound catheter continuous infusion or rectus sheath catheters. A blinded nurse, not participating in data collection read the patientיs number. The participants and people analyzing the data were also blinded. All the randomized patients completed the trial, .
For all patients clinical examination was performed, and routine laboratory investigations were assessed including the following: complete blood picture, fasting and postprandial blood glucose, prothrombin time and activity, liver and renal functions. Intra-operatively the patients were monitored continuously for oxygen saturation, end tidal CO2, heart rate (HR) and rhythm using electrocardiogram (ECG). Arterial blood pressure (systolic, diastolic and mean) was measured non-invasively every 5 min and a urinary catheter was inserted for collection of urine output.
.1 Anesthesia
After preoxygenation with 100% oxygen for 3–5 min, anesthesia was induced with I.V fentanyl (1 μg/kg) and propofol (2 mg/kg) followed by rocuronium (0.6 mg/kg), to facilitate endotracheal intubation. Patients’ lungs were ventilated to maintain end tidal CO2 at 35–40 mmHg. Anesthesia was maintained by isoflurane 1.5% with incremental doses of rocuronium (0.2 mg/kg) when needed (guided by train-of-four test; adequate surgical relaxation was achieved with 1 or 2 twitches present in train-of four-test that correlates with greater than 80% twitch depression) and intraoperative analgesia was provided by 0.5 μg/kg IV fentanyl every 30 min.
.2 Recovery
After the end of surgery and study procedures (according to the patients’ group) the isoflurane was discontinued and the muscle relaxant was reversed by neostigmine (0.05 mg/kg) with atropine (0.01 mg/kg) I.V and the patients were extubated when they were fully awake.
.3 Postoperative analgesia
Group I: wound catheter continuous infusion group (CWCs) “n = 30”: Two wound catheters were inserted before closure of the surgical wound.
Technique: The surgeon implanted two multi-holed catheters into the surgical wound. One catheter was placed in the subcutaneous layer of one side and the other was placed on the other side of the wound at the level of the sutures. A length of 6–10 cm of the catheters was embedded into the wound and secured to the skin. Then the catheters were connected to an infusion pump, preloaded with bupivacaine 0.25%. The loading dose was 10 mL of 0.25% bupivacaine infused through each catheter. Analgesia was maintained by infusing 0.25% bupivacaine at a rate of 4 mL/h through the two catheters (2 mL/h per catheter) for 48 h.
Group II: rectus sheath catheters group (RSCs) “n = 30”: rectus sheath catheters were inserted bilaterally by the aid of ultrasonography at the end of surgery.
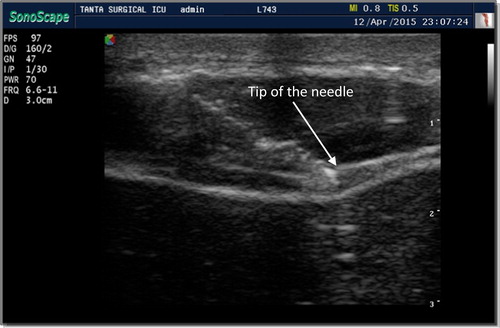
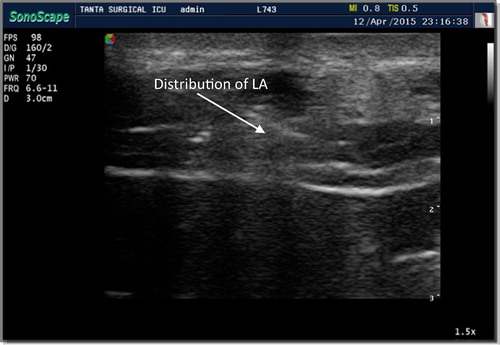
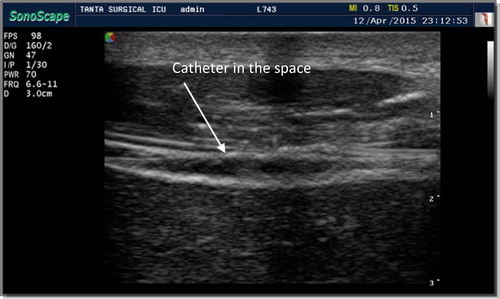
Technique: the skin of the upper abdomen was prepared with 2% betadine, and sheathed ultrasonography probe, broadband (5–12 MHz), linear array with an imaging depth of 4–6 cm, and 50 mm footprint was used. The rectus muscle was imaged in a longitudinal orientation above the level of the umbilicus. At first the probe identified the linea alba, and then moved laterally to demonstrate the main body of the rectus abdominis muscle and the posterior rectus sheath; then, 18G Tuohy needle was introduced few millimeters from the probe at an angle of approximately 45 degrees to the skin just below the costal margin using an in-plane technique. The ultrasound image allowed identification of the rectus muscle and two hyper echoic railway-like lines deep to it (posterior rectus sheath and fascia transversa-lis) . The needle tip was advanced under US guidance and when it reached the posterior sheath (tramlines) ,a bolus of normal saline was injected to achieve hydro-dissection between the rectus muscle and the underlying posterior rectus sheath and confirm the correct position. Then 20 mL bupivacaine 0.25% (loading dose) was injected down the Tuohy needle and this opened up the potential space between the rectus muscle and posterior rectus sheath, allowing the catheters to be inserted. The hydro-dissected space was easily visible on ultrasound confirming their correct positioning . The catheter was introduced through the needle into the space between rectus muscle and the posterior rectus sheath. Then 4–8 cm of the catheter was left in this space . To avoid interference with the surgical field, the rest of the catheter was tunneled laterally. The procedure was repeated on the opposite side. Analgesia was maintained by injecting 10 mL bupivacaine 0.25% in each catheter every 6 h in the first 24 h and then every 12 h in the second 24 h postoperatively.
.4 Evaluation
Primary outcomes: Severity of pain was assessed using Visual Analogue Pain Scale (VAS) score (0–10) at rest and with activity (movement in bed) at time 0 (fully awake), 6, 12, 24, 36 and 48 h postoperatively. If pain scores ⩾ 4 the patient received titrated morphine iv bolus dose (2 mg if the patient′s body weight is ⩽60 kg or 3 mg if the patient′s body weight is >60 kg), lockout interval, 5 min till VAS <3 was achieved and no upper limit to the number of doses. Morphine titration was stopped if the respiratory rate was <12 breaths/min, O2 saturation <95%, Ramsay sedation score >2 or there was serious side effect (hypotension, allergy, severe vomiting) [Citation11,Citation12]. Postoperative I.V morphine consumption was recorded and patient satisfaction was evaluated using a four-point verbal rating scale at 48 h (4 = extremely satisfied, 3 = satisfied, 2 = unsatisfied and 1 = extremely unsatisfied) [Citation13].
Secondary outcomes: heart rate (HR) and mean arterial blood pressure (MAP) were measured at time 0, 6, 12, 24, 36 and 48 h postoperatively. Any undesirable postoperative side effects or complications were recorded.
The data were analyzed using SPSS (version 20); quantitative data were expressed as mean ± SD (age, weight, duration of anesthesia, HR and MAP) and analyzed using independent-t-test for comparison between the two groups. F Test was used for comparison within the same group and Tukey’s test is used as post hoc test. The nonparametric data (the VAS at rest, VAS at movement and patient satisfaction) that did not follow the normal distribution were analyzed with Mann–Whitney U test for comparison between the two groups and Kruskal Wallis H test for comparison within the same group, while the sex, number of patients who needed supplemental injection, and complications were expressed as (number %). P < 0.05 was considered statistically significant.
Results
The two groups were comparable for age, weight, sex, ASA, and duration of surgery (p > 0.05), . The heart rate and mean arterial pressure increased significantly in group I at 12 and 24 h as compared to time 0 (fully awake) and 48 h values (P < 0.05), while there was no significant change in heart rate and mean arterial blood pressure in group II at all-time intervals (P = 0.371). Comparison between groups revealed a significant increase in heart rate and mean arterial pressure in group I as compared to group II at all-time intervals: time 0 [(fully awake) p = 0.002 and 0.001 respectively], 6, 12, 24, 36 and 48 h (p = 0.001), and .
able 1 Demographic data and patient characteristics in two studied groups.
able 2 Heart rate in the studied groups.
able 3 Mean arterial blood pressure in the studied groups.
The VAS at rest showed a significant difference among its values within the two groups at all time intervals (P = 0.001). There was a statistically significant decrease in VAS at rest in group II as compared to group I at all-time intervals: time 0 (fully awake) p = 0.001, 6 h (p = 0.037), 12 h (p = 0.001), 24 h (p = 0.001), 36 h (p = 0.036) and 48 h (p = 0.001), . Also, comparison of the two groups showed a significant decrease in the values of VAS at movement in group II compared to group I at all-time intervals: time 0 (fully awake p = 0.012), 6, 12, 24, 36 and 48 h (p = 0.001) postoperatively, .
Concerning the need for rescue analgesia, 8 patients (26%) in group I required rescue analgesia, 7 patients of them required one dose and one patient required two doses. In group II, two patients (6.6%) required rescue analgesia, both required one dose, and the total morphine consumption increased significantly in group I compared to group II, .
The patient satisfaction was better in group II compared with group I (p = 0.005). Most of the patients in the two studied groups are extremely satisfied or satisfied (93.3% in group II and 76.7% in group I, respectively). No patient in group II was extremely unsatisfied, and only 10% of patients in group I were extremely unsatisfied. Moreover, 6.7% of patients in group II and 13.3% of patients in group I were unsatisfied, . There were no apparent local anesthetic, catheter-related complications or any undesirable side effects in the two studied groups.
able 4 Patient satisfaction in the two studied groups.
Discussion
The two studied groups were comparable regarding the patient characteristics and duration of surgery. Both techniques were effective in reducing the postoperative pain as indicated by the low VAS scores at rest and movement in bed and the need for rescue morphine analgesia in the first 48 h in both groups. The ultrasound guided rectus sheath catheters analgesia (RSCs) was better than continuous wound infusion as indicated by the better VAS at rest and movement in bed in group II compared to group I at all-time intervals. Also, the number of patients who needed rescue morphine analgesia and the total morphine consumption in group II was significantly lower [2 patients (6.6%)] compared to group I [8 patients (26%)].
A challenging issue for analgesia of large midline abdominal incisions, is the extensive origin of the nerves (T5–T12 and L1) that must be blocked [Citation14]. The anterior branches of the lower six thoracic and first lumber sensory nerves travel in the transversus abdominis plane (TAP) and enter into the rectus sheath medially, and they penetrate the rectus muscle anteriorly [Citation15], supplying motor fibers to rectus abdominis and sensory fibers to rectus abdominis and the skin overlying it in either side of the midline. Above the umbilicus, the rectus muscle and the nerves supplying it are contained both anteriorly and posteriorly within a distinct fascia, whereas below the umbilicus the posterior fascia becomes less distinct. This compartment is divided by the arcuate lines, creating a physical barrier to the spread of an injected solution, but posteriorly these are deficient and permit tunneling of a catheter into the rectus compartment. So, an injected solution can spread throughout the posterior aspect of the compartment [Citation16]. As a single bolus of local anesthetics has a maximum duration of 12 h [Citation7], it is necessary to insert a catheter into the space to allow either a continuous infusion or repeated boluses of local anesthetics postoperatively.
Similar results were obtained by Shido et al. [Citation17], Parson et al. [Citation18], Malchow et al. [Citation19], Godden et al. [Citation20], Dutton et al. [Citation21] and Bakshi et al. [Citation22]. In contrary to our results, Pandmanbhan et al. [Citation23] found that intermittent infusion of bupivacaine after midline laparotomy into the rectus sheath-space does not reduce pain score postoperatively. This may be because they did not give their patients a loading dose of local anesthetics, and also they did not describe the technique of the block in details and if they used the blind technique or the ultrasound guidance.
As regards the patient satisfaction in the present study, there was a significant increase in the patient satisfaction in group II compared with group I. Also, most of the patients in the two studied groups were extremely satisfied or satisfied, while no patient in group II was extremely unsatisfied and only 10% of patients in group I were extremely unsatisfied. Moreover, 13.3% of patients in group I and 6.7% of patients in group II were unsatisfied. This may be due to the safety of both techniques and the low VAS at rest and at movement and the low number of patients who needed rescue analgesia in both groups. The less patient satisfaction in the CWCs group (group I) in our study can be explained by the possibility of limited patient mobility due to continuous infusion. Also, the VAS at movement in bed and the need for rescue analgesia are more in group I compared to group II. The patient satisfaction was infrequently reported in most of the clinical trials; however, Fredman et al. [Citation5] reported that the majority of their patients were satisfied.
As regards the changes in heart rate and mean arterial blood pressure, there was a significant increase in both HR and MAP in group I at 12 and 24 h compared to time 0 and 48 h and this was consistent with the time of increased pain intensity. Also, there was a significant increase in HR and MAP in group I compared to group II at all-time intervals. This can be explained on the basis of increased VAS scores in group I compared to group II.
Concerning the complications in the present study, no serious complications as hematoma in the rectus sheath, ileus, nausea, vomiting or local anesthetic toxicity were found in the two studied groups. The results of Bashandy and Elkholy [Citation14] and Malchow et al. [Citation19] on rectus sheath catheters are in agreement with our results. Also, our results are in line with those of Liu et al. [Citation3] and Polglase et al. [Citation6] who reported low incidence of catheter related complications in their continuous wound catheters patients. Potential adverse events of the ultrasound guided rectus sheath catheters include failed block, peritoneal injection of the local anesthetic, puncture of epigastric vessels, and wound infections [Citation10] but these are rare and have been described only after blind insertion using anatomic landmarks and tactile stimuli [Citation18]. A hematoma in the rectus sheath is of much less significance than that of the epidural space and so, the use of RSCs is allowed when epidural catheters are contraindicated owing to concomitant anticoagulation [Citation21]. Reduced need for morphine in the two studied groups of the present study has many advantages e.g. decreased incidence of postoperative nausea and vomiting (PONV) which was considered as a primary concern postoperatively as it may result in major patient discomfort, poor satisfaction, increased costs, and nursing care [Citation24].
However this study has some limitations: In ultrasound-guided rectus sheath catheters block group, the ultrasound is not always available, and also training the personnel is very important, while the high cost of the catheters and infusion sets and the limited patient movement in continuous local wound infiltration limit its routine use. Also, the study must be repeated on a larger number of patients before the findings of this trial to be generalized.
We concluded from the present study that ultrasound-guided rectus sheath catheters block provided better analgesia compared with continuous local wound infiltration in the management of postoperative pain in patients undergoing colorectal surgery without any undesirable side effects.
Conflict of interest
None.
Funding source
Self funded (the authors supported the study by themselves).
The contents have not been published elsewhere and the paper is not being submitted elsewhere.
Acknowledgments
Assistance: non declared. Financial support: non declared. Conflict of interest: non declared. Presentation: non declared.
Notes
IRB: The Research Ethics Committee of the Faculty of Medicine, Tanta, Egypt, approval code: 2474/03/14.
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- M.K.BaigS.D.WexnerPostoperative ileus: a reviewDis Colon Rectum4742004516526
- M.K.BaigO.ZmoraJ.DerdemeziE.G.WeissJ.J.NoguerasS.D.WexnerUse of the ON-Q pain management system is associated with decreased postoperative analgesic requirement: double blind randomized placebo pilot studyJ Am Coll Surg20222006297305
- S.S.LiuJ.M.RichmanR.C.ThirlbyC.L.WuEfficacy of continuous wound catheters delivering local anesthetic for postoperative analgesia: a quantitative and qualitative systematic review of randomized controlled trialsJ Am Coll Surg20362006914932
- A.KarthikesalingamS.R.WalshS.R.MarkarU.SadatT.Y.TangC.M.MalataContinuous wound infusion of local anaesthetic agents following colorectal surgery: systematic review and meta-analysisWorld J Gastroenterol: WJG143420085301
- B.FredmanE.ZoharA.TarabykinA.ShapiroA.MayoE.KleinBupivacaine wound instillation via an electronic patient-controlled analgesia device and a double-catheter system does not decrease postoperative pain or opioid requirements after major abdominal surgeryAnaesth Analg9212001189193
- A.PolglaseP.McMurrickP.B.SimpsonR.WaleP.G.CarneW.JohnsonContinuous wound infusion of local anesthetic for the control of pain after elective abdominal colorectal surgeryDis Colon Rectum5012200721582167
- D.J.SandemanA.V.DilleyUltrasound-guided rectus sheath block and catheter placementANZ J Surg7872008621623
- P.MarhoferM.GreherS.KapralUltrasound guidance in regional anaesthesiaBr J Anaesth9412005717
- J.DolanP.LucieT.GearyM.SmithG.KennyThe rectus sheath block for laparoscopic surgery in adults: a comparison between the loss of resistance and ultrasound guided techniquesAnaesthesia6232007302
- S.FergusonV.ThomasI.LewisThe rectus sheath block in paediatric anaesthesia: new indications for an old technique?Paediat Anaesth661996463466
- F.AubrunJ.-X.MazoitB.RiouPostoperative intravenous morphine titrationBr J Anaesth10822012193201
- F.AubrunS.MonselO.LangeronP.CoriatB.RiouPostoperative titration of intravenous morphine in the elderly patientAnesthesiologists96120021723
- M.ShahS.S.KulkarniW.FunThe analgesic efficacy of ultrasound-guided modified rectus sheath block compared with wound infiltration in reduction of postoperative morphine consumption in women undergoing open hysterectomy or myomectomy: a randomized controlled trial 14/09/2012 trialJ Obst Anaesth Crit Care22201274
- G.M.N.BashandyA.H.H.ElkholyReducing postoperative opioid consumption by adding an ultrasound-guided rectus sheath block to multimodal analgesia for abdominal cancer surgery with midline incisionAnesthesiol Pain Med432014
- W.RozenT.TranM.AshtonM.BarringtonJ.IvanusicG.TaylorRefining the course of the thoracolumbar nerves: a new understanding of the innervation of the anterior abdominal wallClin Anat2142008325333
- P.CornishA.DeaconRectus sheath catheters for continuous analgesia after upper abdominal surgeryANZ J Surg771–2200784
- A.ShidoN.ImamachiK.DoiS.SakuraY.SaitoContinuous local anesthetic infusion through ultrasound-guided rectus sheath cathetersCan J Anesth5711201010461047
- B.ParsonsJ.AningM.DaughertyJ.McGrathThe use of rectus sheath catheters as an analgesic technique for patients undergoing radical cystectomyBr J Med Surg Urol4120112430
- R.MalchowL.JaegerH.LamRectus sheath catheters for continuous analgesia after laparotomy – without postoperative opioid usePain Med127201111241129
- A.GoddenM.MarshallA.GriceI.DanielsUltrasonography guided rectus sheath catheters versus epidural analgesia for open colorectal cancer surgery in a single centreAnn R Coll Surg Engl9582013591594
- T.J.DuttonJ.S.McGrathM.O.DaughertyUse of rectus sheath catheters for pain relief in patients undergoing major pelvic urological surgeryBJU Int11322014246253
- S.BakshiA.MapariR.PaliwalUltrasound-guided rectus sheath catheters: a feasible and effective, opioid-sparing, post-operative pain management technique: a case seriesIndian J Anaesth5922015118
- J.PadmanabhanA.RohatgiA.NiazE.ChojnowskaK.BaigW.WoodsDoes rectus sheath infusion of bupivacaine reduce postoperative opioid requirement?Ann R Coll Surg Engl8932007229
- T.J.GanT.MeyerC.C.ApfelF.ChungP.J.DavisS.EubanksConsensus guidelines for managing postoperative nausea and vomitingAnaesth Analg97120036271