Abstract
Background
Transversus abdominis plane (TAP) block provides sensory block from T6 to L1. It is one of the most widely used regional analgesic techniques and important component of multimodal approach for postoperative analgesia in multiple lower abdominal surgeries.
Objective
To compare between the analgesic potency of ropivacaine 0.2% and ropivacaine 0.5% when used in transversus abdominis plane (TAP) block for post operative analgesia after cesarean delivery.
Patients and methods
Fifty parturients with American society of Anesthesiologists Physical Status I or II aged between 25 and 35 years undergoing cesarean delivery with general anesthesia were included in this prospective, randomized, double blind study. They were randomly divided into 2 groups according to the concentration of ropivacaine used in TAP block. The 1st group received bilateral 20 ml of 0.2% ropivacaine while the 2nd received the same volume of 0.5% ropivacaine at the end of the surgery. Intensity of postoperative pain at rest and during movement, time to 1st analgesic request, total dose of tramadol used, time to 1st mobilization from bed, parturients satisfaction of pain management, and complications of TAP block were recorded.
Results
Visual Analogue Scale (VAS) at rest and during movement, time to 1st analgesic request, total dose of tramadol, time to 1st mobilization from bed, patients satisfaction of pain management were comparable between the two groups.
Conclusion
Ropivacaine 0.2% when used in TAP block provided postoperative analgesia similar to ropivacaine 0.5% in TAP block after cesarean delivery.
Introduction
Postoperative pain after cesarean delivery represents a major problem that facing both the obstetrician and the anesthesiologist; it is mainly related to the abdominal wall incision and dissection of the abdominal muscles [Citation1]. Inadequate postoperative analgesia after cesarean delivery delays ambulation with subsequent increased risk of thromboembolism, and harms mother–baby relationship [Citation2]. Goal standard for postoperative pain is opioids whether administered systemic or neuraxial but it is associated with many side effects such as nausea, vomiting, pruritus, constipation, and respiratory depression [Citation3]. Multimodal approach of postoperative analgesia which combines parenteral analgesics with regional analgesic techniques may enhance analgesia of each component and decrease its side effects [Citation4]. Transversus abdominis plane (TAP) block represents one of the most widely used regional analgesic techniques and important component of multimodal approach for postoperative analgesia [Citation5]. Transversus abdominis plane (TAP) is a neurovascular plane between the internal oblique muscle and the transversus abdominis muscle through which pass the nerves supplying the anterolateral abdominal wall [Citation6]. Application of the local anesthetics in this plane will produce myocutaneous sensory block between T6 and L1 (TAP) block which is suitable for pain relief in abdominal surgeries [Citation7]. TAP block was described for the 1st time by Rafi in 2001; he called the technique as refined abdominal field block. TAP block has been used successfully as an important element of multimodal postoperative analgesia for many abdominal procedures such as cholecystectomy, gynecological laparoscopy, appendectomy, nephrectomy, and cesarean delivery [Citation8].
able 4 Visual Analogue Scale (VAS) during rest.
Establishment of TAP block requires injection of large dose of LA in this relatively vascular plane which leads to potential neurotoxic plasma level of the LA [Citation9], especially during pregnancy which increases susceptibility of the pregnant women to local anesthetic toxicity [Citation10].
The aim of this study was to compare between ropivacine 0.2% and ropivacaine 0.5% as regards their analgesic potency and safety when they used in TAP block for postoperative analgesia after cesarean delivery performed under general anesthesia.
Patients and methods
This prospective, randomized, double blinded study was performed in El –Minia university hospital in the period from July 2014 to July 2015. After obtaining approval of the local ethics committee of the faculty of medicine and informed written consents from all the parturients, fifty parturients ASA I or II aged from 25 to 35 years scheduled for cesarean delivery under general anesthesia. Parturients with coagulopathy, infection in the site of the block, allergy to LA used, or sensitivity to prescribed analgesics, who are unable to understand visual analogue scale (VAS) were excluded.
Parturients included in the study were randomly allocated into two equal groups according to the concentration of the ropivacaine used in TAP block by random allocation software (windows software, version 1.0, May 2004). The allocation ratio was 1:1 and the group identification cards were put in sealed and opaque envelops to hide allocation. The local anesthetic solution was made by the pharmacist in a glass bottle labeled as A or B. Parturients were injected with 20 ml of this solution in each side in the TAP. At the end of the study these labels were known from the pharmacist that A was ropivacine 0.2% while B was ropivacaine 0.5%. Anesthesiologist, parturients, and nursing staff who follow up the parturients were blinded with the concentration of ropivacaine used. Parturients were instructed to use Visual Analogue Scale (VAS) 0/10 to assess the post operative pain, where 0 represents no pain while 10 represents the worst possible pain. Parturients were cannulated when they entered the operation room and they preoxygenated for 3 min through face mask. Standard monitoring (pulse oximetry, electrocardiogram, capnography, and non invasive blood pressure measurement) was applied to the parturients. Induction of anesthesia was done by thiopental 5 mg/kg and succinylcholine 1 mg/kg followed by tracheal intubation with suitable size of endotracheal tube with cricoid pressure. Maintenance of anesthesia was done by isoflurane 1% and atracurium 0.25 mg/kg to maintain train–of- four (TOF) at 1 throughout the surgery using peripheral nerve stimulator and mechanical ventilation was adjusted to keep end-tidal PaCo2 at 35–45 mmHg. After delivery of the baby, the parturients received 5 international units (I.U) bolus dose of oxytocin and 40 I.U as continuous infusion. 1 μg/kg fentanyl was administered to the parturients after delivery. At the end of the surgery and after wound closure TAP block was performed by the guidance of ultrasound device CHISON Ultrasound Diagnostic System model ECO 3 Chison Medical Imaging Co., Ltd. No 8, XIANG NAN ROAD, SHUO FANG, NEW District, WUXI, China, 214142 with broadband linear array probe 6–11 MHz.
.1 Technique of TAP block
After complete disinfection and sterilization of the entry site which located in the midaxillary line midway between the costal margin and the iliac crest, 150 mm Stimuplex needle (B-Braun Medical, Bethlehem, PA, USA) was advanced in the neurofascial plane between the internal oblique muscle and transversus abdominis muscle using plane technique. Once the needle was introduced in the correct place 20 ml of the LA solution was injected. Visualization of hypoechoic layer between the two muscles on injection of the local anesthetic solution was considered as the end point of success of the block [Citation11]. This procedure was repeated on the other side.
After the end of the TAP block anesthesia was terminated and neuromuscular block was antagonized by 2.5 mg neostigmine plus 1 mg atropine, then extubation was done when airway reflexes returned. Parturients considered awake when they could open their eyes on command.
Parturients were transferred to the post anesthesia care unit (PACU) where they were observed by nursing staff blinded with the concentration of LA used. Parturients received analgesic regimen of 1 gm of intravenous paracetamol/24 h, and diclofenac 75 mg I.V infusion/8 h starting from the time of admission to PACU to overcome the visceral component of postoperative pain. Parturients were advised that they could ask for a rescue analgesic dose if the VAS was >4 at any time. The rescue analgesic dose was bolus dose of 0.5 mg/kg of tramadol hydrochloride though intravenous route.
Parameters assessed
| . | Intensity of pain using visual analogue scale (VAS) where 0-no pain or 10 = maximum sever pain during rest and during movement (passive flexion of hip and knee) at 30 min, 1, 2, 4, 8, 12, 24 h after admission to the PACU. | ||||
| . | Time to 1st analgesic request (time from TAP block), number of analgesic doses in the 1st 24 h, and total dose of tramadol hydrochloride in the 1st 24 h. | ||||
| . | Time to 1st mobilization from bed after surgery. | ||||
| . | Parturients satisfaction of pain management according to patient satisfaction scale where 0 = very unsatisfied and 10 = highly satisfied at the time of discharge. | ||||
| . | Symptoms of LA toxicity e.g. numbness, tingling, or arrhythmia. | ||||
| . | Complication of TAP block technique such as hematoma, infection, pain at site of entry, and visceral injury. | ||||
Sample size calculation
Using Power Analysis and Sample Size System (PASS) software (NCSS, East Kaysville, Utah, USA), it was found that the least number of parturients required in each group to detect three scores difference in VAS with 95% power and 0.05% significance level was 22 parturients with 10% dropout ratio, and the number increased to 25 parturients in each group.
.1 Statistical analysis
Data were expressed as mean ± SD, or number and percentage. Data were analyzed with SPSS version 21 (SPSS Inc., Chicago, IL, USA).
Data were tested for normal distribution by Kolmogorov-Smirnov test. One-way analysis of variance (ANOVA) was used to analyze normally distributed continuous data. None of normally distributed data were analyzed by chi-square or Fisher’s exact test. All tests are two-tailed. P value of <0.05 was considered significant.
Results
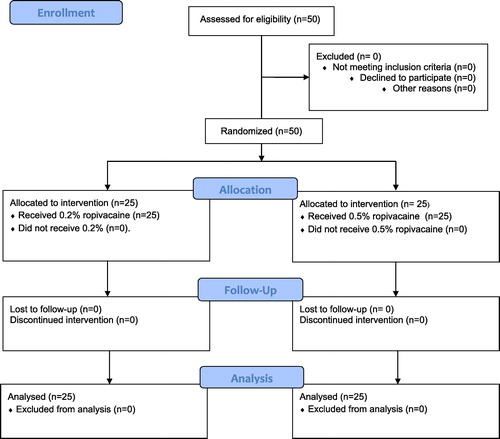
A total number of 50 parturients were randomized for the study in the period from January 2014 to July 2015. None of the parturients were excluded from the study nor lost follow up nor lost analysis .
There was no significant difference between the two groups as regards characteristics of the parturients or number of the cesarean. The average time of the surgery was 55 ± 11 min in group 0.2% ropivacaine and was 57 ± 8 min in 0.5% ropivacaine with no significant difference . There was no significant difference between the two groups as regards the time of the 1st request of analgesic dose where it was 4.2 ± 0.3 h in group 0.2% ropivacaine and 4.3 ± 0.4 in group 0.5% ropivacaine . Time to 1st mobilization from bed was 2.3 ± 0.6 h in group 0.2% ropivacaine while it was 2.1 ± 0.5 h in group ropivacaine 0.5% with no significant difference between the two groups. There was no significant difference between the two groups as regards the total dose of tramadol hydrochloride as it was 160 ± 10 mg in 0.2% ropivacaine group and 150 ± 9 mg in 0.5% ropivacaine group. As regards the patient satisfaction score there was no significant difference between the two groups as it was 7.8 ± 1.2 in 0.2% ropivacaine group while it was 8 ± 1.4 in 0.5% ropivacaine group. There was no significant difference between the two groups as regards VAS whether at rest or during movement (see –).
able 1 Parturients characteristics.
able 2 Time to 1st analgesic request, and 1st mobilization.
able 3 Total dose of tramadol hydrochloride, number of analgesic doses, and patients satisfaction of pain management score.
able 5 Visual Analogue Scale (VAS) during movement.
Discussion
This study compared two ropivacaine concentrations 0.2% and 0.5% as regards their postoperative analgesic potency when used for TAP block after cesarean delivery performed under general anesthesia and it was found that the two concentrations provided nearby postoperative analgesia after cesarean delivery as shown by VAS and patients satisfaction. The volume of the local anesthetic LA which injected in TAP was selected to be 20 ml in each side which coincides with Moeschler et al. [Citation12] in their study on cadavers, in which they injected different volumes of contrast in TAP and they concluded that the increased volume of the injected contrast would increase the cranio-caudal spread and would reach iliohypogastric nerve, and intercostals nerve which increase the incidence of success rate of the TAP block and they suggested that 15 ml of LA may be the optimal volume of LA to provide adequate TAP block. In this study the volume was increased to 20 ml in each side to compensate for the possible intramuscular spread of the LA.
Chen and Phui [Citation13] found that injection of 20 ml of ropivacaine 0.375% for TAP block was effective as intraoperative and postoperative analgesic in 10 cases of laparoscopic cholecystectomy even after they were diverted to open cholecystectomy.
This coincides with Abdul Jalil et al. [Citation14] in their prospective, randomized, double blind study on 56 parturients scheduled for appendectomy under general anesthesia and they received TAP block with ropivacaine 0.2% in one group and ropivacaine 0.5% in the other group at the end of the surgery and they found that both concentrations provided comparable postoperative analgesia.
Also this coincided with Oliviera et al. [Citation15] in their prospective randomized, double blinded, placebo controlled study on 98 females scheduled for outpatient gynecological laparoscopy in which they compared between ropivacaine 0.25 and ropivacaine 0.5% in TAP block to provide postoperative analgesia and they found that there was no significant difference between the two concentrations in their analgesic potency and no significant difference in parturients satisfaction score between the two concentrations.
Sirvasta et al. [Citation16] in their randomized double blind study on 62 pregnant women scheduled for cesarean delivery to assess the role of TAP block as a component of multimodal postoperative analgesia and they found that the TAP block significantly decreased pain score at all study times during rest and movement and also decreased parturients consumption of tramadol through patient controlled analgesia.
McDonnell et al. [Citation17] in their study evaluated the effectiveness of TAP block with ropivacaine for postoperative analgesia in cesarean delivery performed under spinal anesthesia, and they found that TAP block significantly decreased the pain score and 48 h morphine consumption.
In this study there were no complications of the TAP block technique as hematoma, infection, visceral injury, and vascular injury, and this may be caused by ultrasound guidance of the procedure, but this does not mean the complete safety of the procedure as Farok and Carey [Citation18] reported hepatic trauma after TAP block and Scharine [Citation19] reported colon puncture or hematoma formation in the entry site.
This study had many limitations. The 1st limitation it was not possible to limit the intramuscular spread of LA solution by the pressure of injection and incomplete separation of the fascial plane which may affect the end result of the amount of LA involved in TAP block [Citation20].
The 2nd limitation was that the study could not eliminate the psychic factor of baby which strongly affects the mother in our locality and could encourage and motivate the mother to tolerate pain and move if male baby.
The 3rd was that the study could not stabilize the severity of surgical trauma or severity of uterine contractions which led to variability of pain severity. The study duration was limited to 24 h only because of the social pressure of the parturients and their relatives to return home as early as possible.
Conclusion
Bilateral 20 ml of ropivacaine 0.2% when used in TAP block provided postoperative analgesia similar to bilateral 20 ml of ropivacaine 0.5% in TAP block after cesarean delivery performed with general anesthesia.
Conflict of interest
The author declared that there was no conflict of interest.
The fund of the study was from the university research.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- T.C.KrivakK.K.ZornVenous thromboembolism in obstetrics and gynecologyObstet Gynecol10932007761777
- A.Y.LeungPostoperative pain management in obstetric anesthesia-new challenges and solutionsJ Clin Anesth1620045765
- T.T.TanW.H.TeohD.C.WooC.E.OcampoM.K.ShahA.T.SiaA randomized trial of the analgesic efficacy of ultrasound-guided transversus abdominis plane block after cesarean delivery under general anaesthesiaEur J Anaesthesiol2920128894
- D.BelvayP.J.CowlishawM.HowesF.PhillipsUltrasound guided transversus abdominis plane block for analgesia after cesarean deliveryBr J Anaesth1032009726730
- J.D.GriffithsF.A.BarronS.GrantA.R.BjorkstenP.HebbardC.F.RoysePlasma ropivacaine concentrations after ultrasound-guided transversus abdominis plane blockBr J Anaesth1052010853856
- M.J.YoungA.W.GorlinV.E.ModestS.A.QuraishiClinical implications of the transverses abdominis plane block in adultsAnesth Res Pract20122012731645
- J.D.GriffithsJ.V.MiddleF.A.BarronS.J.GrantP.A.PophamC.F.RoyseTransversus abdominis plane block does not provide additional benefit to multimodal analgesia in gynecological cancer surgeryAnesth Analg1112010797801
- J.RipollésS.M.MezquitaA.AbadJ.CalvoAnalgesic efficacy of the ultrasound-guided blockade of the transversus abdominis plane- a systematic reviewBraz J Anesthesiol6542015255280
- H.TorupA.U.MitchellT.BreindahlE.G.HansenJ.RosenbergA.M.MollerPotentially toxic concentrations in blood of total ropivacaine after bilateral transversus abdominis plane blocks; a pharmacokinetic studyEur J Anaesthesiol292012235238
- A.C.SantosH.PedersenT.W.HarmonDoes pregnancy alter the systemic toxicity of local anesthetics?Anesthesiology701989991995
- P.Y.HebbardY.FujiwaraY.ShibataC.RoyseUltrasound-guided transversus abdominis plane (TAP) blockAnaesth Intensive Care352007616617
- S.M.MoeschlerN.S.MurthyB.C.HoelzerUltrasound-guided transversus abdominis plane injection with computed tomography correlation: a cadaveric studyJ Pain Res62013493496
- C.K.ChenV.E.PhuiThe efficacy of ultrasound-guided oblique subcostal transversus abdominis plane block in patients undergoing open cholecystectomySouth Afr J Anaesth Analg172011308310
- R.M.Abdul JalilN.YahyaO.SulaimanW.R.Wan MatR.TeoA.IzahamR.A.RahmanComparing the effectiveness of ropivacaine 0.5% versus ropivacaine 0.2% for transabdominis plane block in providing postoperative analgesia after appendectomyActa Anaesthesiol Taiwan52220144953
- G.S.OliveiraP.C.FitzgeraldR.J.MarcusA dose–ranging study of the effects of transversus abdominis block on postoperative quality of recovery and analgesia after outpatient laparoscopyAnesth Analg113201112181225
- U.SrivastaS.VermaT.K.SinghA.GuptaA.SaxsenaK.D.JagarM.GuptaEfficacy of trans abdominis plane block for post cesarean delivery analgesia: a double- blind, drandomized trialSaudi J Anaesth92015298302
- J.G.McDonnellG.CurleyJ.CarneyA.BentonJ.CostelloC.H.MaharajThe analgesic efficacy of transverses abdominis plane block after cesarean delivery: A randomized controlled trialAnesth Analg10612008186191
- M.FarooqM.A.CareyA case of liver trauma with a blunt regional anesthesia needle while performing transversus abdominis plane blockReg Anesth Pain Med3332008274275
- J.D.ScharineBilateral transversus abdominis plane nerve blocks for analgesia following cesarean delivery: report of 2 casesAANA J772200998102
- L.EslamianZ.JaliliA.JamalV.MarsoosiA.MovafeghTransversus abdominis plane block reduces postoperative pain intensity and analgesic consumption in elective cesarean delivery under general anesthesiaJ Anesth1262012334338