Abstract
Background
Spine surgery needs a special consideration as regards minimizing the movement during intubation to avoid the hazards to spinal cord. The present study aims to highlight the preferable technique for cervical intubation. The Intubating Laryngeal Mask Airway (ILMA, Fastrach™ laryngeal mask company, Henle-on-Thomes, U.K.) is a supraglottic device specially designed to be an effective ventilator device and blind intubation guide in patient with normal and abnormal airways.
Methods
40 patients were involved and randomly assigned to two equal groups according to the used technique of endotracheal intubation: (Group 1): Intubating Laryngeal Mask technique and (Group 2): Direct laryngoscopy technique. Anesthesia was induced using a combination of 1 μg/kg fentanyl, 5 mg/kg thiopental sodium (sleeping dose) and atracurium 0.5 mg/kg (Intubating laryngeal Mask or the Macintosh blade) was used to secure the airway according to the patient group. Meanwhile a continuous videofluoroscopy was recorded. The radiographs were analyzed for movements in the cervical segments C1/2 and C2/3. A reference line was drawn following the dorsal alignment of C2. Another two lines, one connecting the anterior and posterior arch of C1, and one through the basal plate of C3, were drawn to transect the above mentioned reference line.
Results
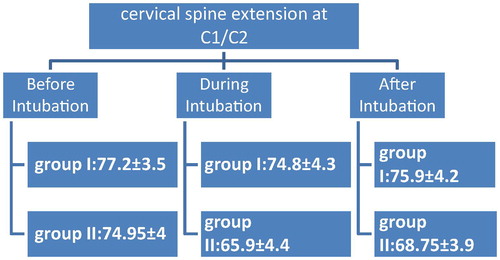
The mean cervical spine extension at C1/C2 was 77.2 ± 3.5 before intubation, 74.8 ± 4.3 during intubation, and 75.9 ± 4.2 after intubation for group 1, while it was 74.95 ± 4 before, 65.9 ± 4.4 during, and 68.75 ± 3.9 after intubation for group 2 there was statistically significant difference between LMA group (group 1) and direct laryngoscopy group (group 2) in the motion of cervical spine extension at C1/C2 during and after intubation where the p-value was <0.05.
Conclusion
The ILM (Fastrach) is a satisfactory alternative to the currently used methods of airway management in cervical spine injuries and reduces movement of the cervical spine.
Introduction
Management of difficult airway remains one of the most relevant and challenging tasks for anesthesia care providers, and claims involving airway management continuing to compromise an important aspect of the American Society of Anesthesiologist (ASA) closed claims project database which tracks all anesthesia-related insurance claims [Citation1]. The practice of airway management has become more advanced in recent years. This advancement is demonstrated by the introduction of many new airway devices, several of which have been included in the American Society of Anesthesiologist (ASA) Difficult Airway Algorithm [Citation2]. The Intubating Laryngeal Mask Airway (ILMA, Fastrach™ laryngeal mask company, Henle-on-Thomes, U.K.) is a supraglottic device specially designed to be an effective ventilator device and blind intubation guide in patient with normal and abnormal airways [Citation3]. Cervical spine surgery needs a special consideration as regards minimizing the movement during intubation to avoid the hazards to spinal cord. The degree of cervical spine extension makes a challenge for the anesthesiologist specially when there is cervical disc lesion or cervical spine fracture.
Aim of the study
The present study aims to compare different intubation methods as regards the cervical spine mobility to highlight the preferable technique for limitation in cervical mobility during intubation. The primary outcome was recording the change in angles C1/2 and C2/3 before, during and after intubation, the secondary outcome which was airway complications as blood streaked mucous after removal of the device, vital signs such as, heart rate and blood pressure, as well as oxygen saturation.
Subject and methods
This randomized controlled study was carried out in Kasr El Ainy Teaching Hospital. We used the simple randomization technique where sequence generation was created by a computerized random number generator (MS Excel model). Participants were intentionally allocated in equal numbers to each group in 1:1 ration. The allocation sequence was concealed from the investigator enrolling and assessing participants in sequentially numbered, opaque sealed envelopes.
After the approval of the ethical committee, 40 patients were undergoing cervical spine surgeries, age from 18 to 65 years, weight 50–120 kg, height >150 cm; ASA class I or II; airway score <4 according to EL Ganzouri scoring system [Citation4]. Patients with BMI more than 30 kg/m2; Patients age above 65 years; airway score ⩾4 (EL Ganzouri scoring system [Citation4]); any chest or cardiac condition that interferes with safe general anesthesia (chest infection, COPD, Bronchial asthma); any anatomical abnormalities in the head and neck that interfere with intubation; or trauma patients were excluded from the study. The patients were randomly (by closed envelope technique) assigned to two equal groups of 20 patients each according to the used technique of endotracheal intubation; (Group 1): Intubating Laryngeal Mask technique and (Group 2): Direct laryngoscopy technique. History taking was done for all patients and they were assessed preoperatively by El Ganzouri scoring system which includes seven criteria. The study has an unique identification number in Pan African Clinical Trial Registry: PACTR201502000993337.
Anesthetic technique
| #x2022; | The standard monitors (pulse oximetry, 5-leads ECG, non-invasive blood pressure) and capnogram were attached to the patient. Check of the ILMA (intubating laryngeal mask airway): Check of both cuffs; the modified tube and the ILMA by inflation and deflation of them. Adequate lubrication of the tube and the ILMA, its outer surface and its inner surface (through frequent passage of the lubricated tube through the ILMA in–out), as well as complete deflation of the cuff of the ILMA. Check of the Macintosh blade: Check the availability of different sizes; blades 3 & 4, depending on the overall size of the patient trying to obtain the best possible view of the larynx normally expected for tracheal intubation. Check of the C-ARM Image: Check the electric source and screen. | ||||
| #x2022; | Before induction of general anesthesia, pre-oxygenation with 100% oxygen for 3 min is given via face mask, General anesthesia was induced using a combination of fentanyl 1 μg/kg, thiopental sodium 5 mg/kg and atracurium 0.5 mg/kg. The patient is mechanically ventilated using a face mask aided with an inhalation anesthetic (isoflurane 1% end tidal) until a full relaxation was established after about 3–5 min. | ||||
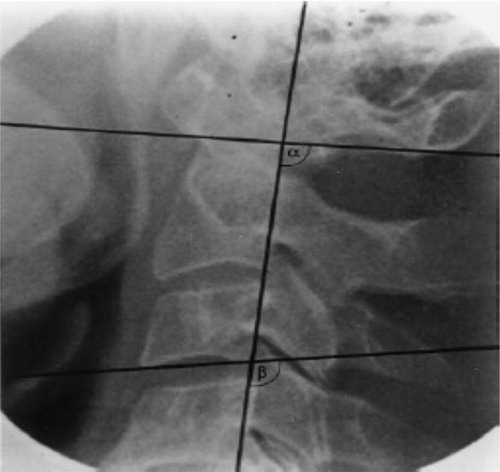
| #x2022; | One of the two devices (Intubating laryngeal Mask or the Macintosh blade) was used to secure the airway according to the patient group. Meanwhile a continuous videofluoroscopy was recorded. The radiographs were analyzed for movements in the cervical segments C1/2 and C2/3. A reference line was drawn following the dorsal alignment of C2. Another two lines, one connecting the anterior and posterior arch of C1, and one through the basal plate of C3, were drawn to transect the above mentioned reference line. | ||||
| #x2022; | Thus, two angles could be defined. The angle between the reference line and the line connecting the anterior and posterior arch of C1 was called a, and the angle between the reference line and the line through the basal plate of C3 was named b () [Citation5]. | ||||
| #x2022; | After intubation, endotracheal placement of the tube rechecked after re-inflated the tubal cuff by attaching the capnogram to the tube and checking ventilation. | ||||
Data management
Data were collected to compare between both groups : the primary outcome which was recording the change in angles C1/2 and C2/3 before, during and after intubation, and the secondary outcome which was airway complications as blood streaked mucous after removal of the device, vital signs such as, heart rate and blood pressure, as well as oxygen saturation.
.1 Data analysis
Data were statistically described in terms of mean ± standard deviation (±SD), median and range, or frequencies (number of cases) and percentages when appropriate. Comparison of numerical variables between the study groups was done using Student t test for independent samples. For comparing categorical data, Chi square (χ2) test was performed. Exact test was used instead when the expected frequency is less than 5. p values less than 0.05 was considered statistically significant. All statistical calculations were done using computer program SPSS (Statistical Package for the Social Science; SPSS Inc., Chicago, IL, USA) version 15 for Microsoft Windows.
.2 Sample size calculation
According to Sahin et al. [Citation12], the movement at the cervical spine was 10.2 ± 7.3°. Taking type I or α error of 5% and type II or β error of 20%, sample size calculation suggested a minimum of 16 subjects per group was required. To be on a safer side, 20 patients were included in each group. Thus, the total number needed was (n = 40) (see ).
able 1 El Ganzouri scoring system [Citation1].
Results
There was no statistical significant difference among groups as regards the demographic characteristics (p > 0.05) ().
able 2 The mean age, weight and height for the both groups.
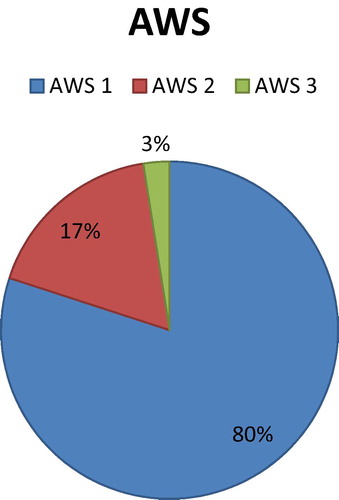
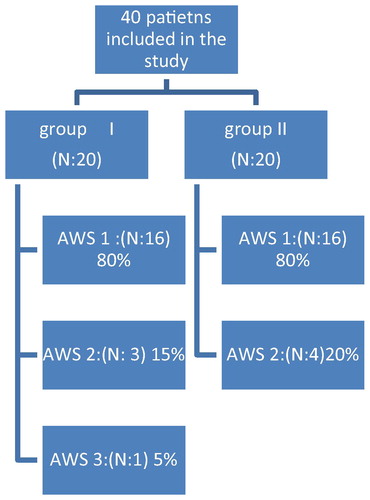
The Airway score (AWS) might range from 0 to 14 according to ALGanzori scoring system but in the current study only scores (0, 1, 2, 3) are included and scores ⩾4 are excluded, and in the current study 32 patients (80%) had AWS 1, 7 patients (17.5%) had AWS 2, 1 patient (2.5%) had AWS 3 and this was shown in . The distribution of AWS between the two groups was as follows: In group 1, 16 patients (80%) had AWS 1, 3 patients (15%) had AWS 2 and 1 patient (5%) had AWS 3 while in the group 2 16 patients (80%) had AWS 1, 4 patients (20%) had AWS 2 and no one had AWS 3. This is illustrated in and (see ).
able 3 The mean systolic BPs, mean diastolic BPs, mean heart rate (pre-insertion and post-insertion).
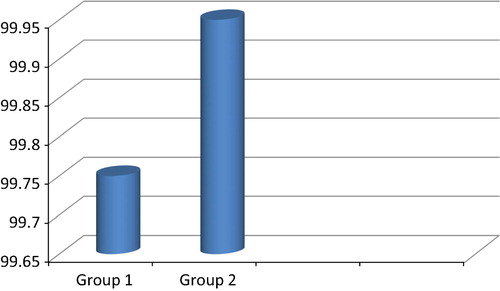
The airway score had no statistical significance among the two groups where the p-value was more than 0.05 (0.746). The mean systolic BPs (pre-insertion) were 121.5 ± 14.2, 119.5 ± 13.2 for group 1 and group 2 respectively with no statistical significant difference where the p-value was >0.05 (0.647). The mean systolic BPs (post-insertion) were 136 ± 11.9 and 137.5 ± 13.3 for group 1 and group 2 respectively and there was no statistical significant difference among the two groups p > 0.05 (0.709). The pre-insertion mean diastolic BPs were 75.5 ± 11.5 for group 1 and 74.5 ± 11 for group 2 while post-insertion mean diastolic BPs were 85 ± 7.6 for group 1 and 86 ± 6 for group 2. There was no statistical significant difference between pre-insertion and post-insertion values where the p > 0.05 (0.780 pre-insertion–0.647 post-insertion). The pre-insertion mean HRs were 73.9 ± 6.4 bpm and 73.7 ± 6.3 bpm for group 1 and group 2 respectively while the post-insertion mean HRs were 84.05 ± 8.4 bpm and 89.9 ± 6.5 bpm for group 1 and group 2 respectively and there was no statistical significant difference among groups (p > 0.05) (). The mean SPO2 were 99.75 ± 0.63 and 99.95 ± 0.22 for group 1 and group 2 respectively and there was no statistical significant difference among groups p > 0.05(0.194). This was illustrated in .
The extension of the cervical spine was calculated from the change in angles between the baseline and the radiograph recorded during and after intubation, and was reported as a mean with (±SD). The mean cervical spine extension at C1/C2 was 77.2 ± 3.5 before intubation, 74.8 ± 4.3 during intubation, and 75.9 ± 4.2 after intubation for group 1, while it was 74.95 ± 4 before intubation, 65.9 ± 4.4 during intubation, and 68.75 ± 3.9 after intubation for group 2; there was statistically significant difference between LMA group (group 1) and direct laryngoscopy group (group 2) in the motion of cervical spine extension at C1/C2 during and after intubation where the p-value was <0.05. This is shown in and .
able 4 Mean cervical spine extension at C1/C2 & C2/C3 before, during and after intubation in both groups.
The mean cervical spine extension at C2/C3 was 100 ± 3.3 before, 102.2 ± 3.6 during, 102.2 ± 3.6 after intubation for group 1, while it was 99.85 ± 3.6 before, 106.75 ± 4 during, 103.1 ± 4.8 after intubation for group 2 and that was statistically significant during intubation and this was shown in . The mean time for device insertion was 55.8 ± 7.5 s and 21.9 ± 4.7 s for group 1 and group 2 respectively and that was statistically insignificant in-between groups. This is shown in .
able 5 Mean time for device insertion.
During device and tube insertion, complications such as blood tinged mucous were recorded in 4 patients (10%) among the 2 groups, it is distributed as 3 patients in group 1(15%), and 1 patient in group 2 (5%) but there was no statistical significant difference among groups (p > 0.05). This is shown in .
able 6 Mucosal injury during device and tube insertion.
Discussion
This study was done on 40 patients that were randomly assigned to two equal groups of 20 patients each according to the used technique of endotracheal intubation as follows:
| #x2022; | (Group 1): Intubating Laryngeal Mask technique. | ||||
| #x2022; | (Group 2): Direct laryngoscopy technique. | ||||
All patients were assessed by Al Ganzouri scoring system. The patients were attached to monitors and after induction of the device inserted (ILMA, Macintosh blade) according to their group. Data collected about: (Time needed for device insertion, Change in angles C1/C2 and C2/C3 before, during and after intubation, Vital signs as oxygen saturation, heart rate and blood pressure). Post intubation the patients were assessed of the presence of bloody mucosa. The collected data revealed that, the mean times of device insertion were 55.8 ± 7.5 s and 21.9 ± 4.7 s for group 1 and group 2 respectively and that was statistically significant in-between groups.
The mean systolic BPs (post-insertion) were 136 ± 11.9 and 137.5 ± 13.3 for group 1 and group 2 respectively and there was no statistical significant difference among groups (p > 0.05). The mean HRs (post-insertion) were 84.05 ± 8.4 bpm and 89.9 ± 6.5 pbm for group 1 and group 2 respectively and that was statistically significant (p < 0.05) but of no clinical significance.
The mean cervical spine extension at C1/C2 was 77.2 ± 3.5 before, 74.8 ± 4.3 during, 75.9 ± 4.2 after intubation for group 1, while it was 74.95 ± 4 before, 65.9 ± 4.4 during, 68.75 ± 3.9 after intubation for group 2 and that was statistically significant during and after intubation.
The mean cervical spine extension at C2/C3 was 100 ± 3.3 before, 102.2 ± 3.6 during, 102.2 ± 3.6 after intubation for group 1, while it was 99.85 ± 3.6 before, 106.75 ± 4 during, 103.1 ± 4.8 after intubation for group 2 and that was statistically significant during intubation. During device and tube insertion, complications such as blood tinged mucous were recorded in 4 patients (10%) among the 2 groups, it is distributed as 3 patients (15%) and 1 patients (5%) in group 1 and group 2 respectively and there was no statistical significant difference among groups (p > 0.05).
In the last years, a number of supraglottic airway devices have been introduced in the clinical practice of the airway management. These devices offer a simple and effective alternative to endotracheal intubation. They allow ventilation of the patient by delivering anesthetic gases/oxygen above the level of the vocal cords. The Intubating Laryngeal Mask is designed to allow intubation through it whether blindly or by the assessment of fiberoptic bronchoscopy [Citation6]. This study was done on 40 patients that were randomly classified into 2 groups, 20 each according to the inclusion and exclusion criteria (Group 1): Intubating Laryngeal Mask technique, (Group 2): Direct laryngoscopy technique.
Many studies had confirmed the value of the Fastrach LMA as a conduit for blind tracheal intubation but to our knowledge, there are few controlled studies that examine cervical spine movements during different tracheal intubating techniques. In this study the angle of cervical spine extension during intubation with the ILM (Fastrach) was significantly less when compared with intubation with direct laryngoscopy at C1/C2 and to some extent at C2/C3. In consistence with the current study, Watts et al. showed in their study that the extension of the occipito-atlantoaxial complex was reduced when using the Bullard laryngoscope and in-line stabilization compared with intubation via the Macintosh laryngoscope [Citation5] Hastings et al. compared cervical spine movement during laryngoscopy with the Bullard, Macintosh, and Miller laryngoscopes [Citation13]. As a result of different methods of measurement, these studies are not directly comparable. However, all of them showed that the greatest cervical spine excursion during intubation occurred at the level of C1/C2. In this study the demographic characteristics and the airway scores were not statistically significant among groups. This finding was consistent with many other studies done on the ILMA, as study done by Hwan et al. using The Intubating Laryngeal Mask Airway with and without Fiberoptic guidance [Citation7], the study done by Galgon et al. using the air-Q® intubating laryngeal airway [Citation10] vs. the LMA-ProSeal and a study done by Nakazawa et al. using the Intubating Laryngeal Mask Airway (LMA-Fastrach™) for blind endotracheal intubation in patients undergoing cervical spine operation [Citation6]. Another study done by Erlacher et al., using CobraPLUS and Cookgas air-Q versus Fastrach for blind endotracheal intubation showed similar findings [Citation8]. In this study, compared with the baseline, both groups showed an increase in systolic and diastolic blood pressure and heart rate at post insertion measurements. Although the increase in systolic and diastolic arterial pressure and heart rate during intubation was less in the ILM (Fastrach) group, it was not statistically Significant except for the HR was statistically significant in post insertion measurements but without clinical significance. Thereafter, no differences in hemodynamic parameters occurred between the groups. Oxygen saturation did not decrease below 98% during the intubation procedures in either group. The mean times of device insertion in our study were 55.8 ± 7.5 s and 21.9 ± 4.7 s for group 1 and group 2 respectively and that was statistically significant in-between groups. As a result of different definitions of the airway insertion time, the following studies are not directly comparable. However, Watts et al. [Citation5] compared the Bullard and Macintosh laryngoscopes with or without in-line stabilization for tracheal intubation of patients with a potential cervical spine injury. In the simulated emergency situation, they reported an intubation time of 25.6 (10.4) s using the Bullard laryngoscope without in-line stabilization vs. 40.3 (19.6) s with in-line stabilization and 20.3 (12.8) s for the Macintosh laryngoscope. Nolan and Wilson [Citation14] described intubation over a 15 Ch gum elastic bougie with manual in-line stabilization in a simulated emergency cervical spine injury situation and showed that all patients were intubated within 45 s (median 25 s) vs. 20 s in the visual technique group. Waltl et al. compared direct laryngoscopy vs. ILMA showed that the mean intubating time via the ILM (Fastrache) was 39 (7) s, ranging from 31 to 57 s, vs. 21 (5) s, ranging from 16 to 34 s via direct laryngoscopy [Citation9].
All the above mentioned studies show that for the time being, in the absence of intubating difficulties, direct laryngoscopy is still the fastest method to secure the airway. In contrast, the Laryngeal Mask Airway and the ILM (Fastrache) are fairly fast, well established and widely used blind intubation techniques in the management of a difficult or failed intubation, particularly because they allow oxygenation of the patient throughout the intubation procedure. During device and tube insertion, complications such as blood tinged mucous were recorded in 4 patients (10%) among the 2 groups, it is distributed as 3 patients (15%), 1 patient (5%) in group 1 and group 2 respectively and there was no statistical significant difference. Our findings were matching with the study done by Galgon et al. [Citation10] as the bloody mucosa was seen in 19% of cases using Air Q and study done by Jagannathan et al. [Citation11] using tracheal tube as a stabilizing rod during removal of ILMA.
Conclusion
The ILM (Fastrach) was a satisfactory alternative to the currently used methods of airway management in cervical spine injuries. It is a technique in which it is easy to acquire expertise, it reduces movement of the cervical spine, intubation is achieved rapidly, there is hemodynamic stability, and oxygenation is possible throughout the intubating procedure.
Conflict of interest
No conflict of interest.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- CG: management of difficult intubation in closed malpractice claims. ASA Newsletter 2000;64(6):13–9.
- American Society of Anesthesiologist: task force on management of difficult airway. Practice guide lines for management of the difficult airway. An update report by the American Society of Anesthesiologist. Task force on management of the difficult airway. Anesthesiology 2003;98(5):1269–77.
- A.I.BrainC.VergheseE.V.AddyA.KapilaJ.BrimacombeThe intubating laryngeal mask. II: a preliminary clinical report of a new means of intubating the tracheaBr J Anesth791997704709
- A.R.El-GanzouriR.J.McCarthyK.J.TumanA.D.IvankovichFirst step to safe anesthesia: preoperative prediction of difficult intubationAnestheiology82199611971204
- A.D.WattsA.W.GelbD.B.BachD.M.PelzComparison of the Bullard and Macintosh laryngoscopes for endotracheal intubation of patients with a potential cervical spine injuryAnesthesiology87199713351342
- KoichiNakazawaNaofumiTanakaSeijiIshikawaSusumuOhmiMasatoUekiYutakaSaitohKoshiMakitaKeisukeAmahaUsing the intubating Laryngeal Mask Airway (LMA-Fastrach™) for blind endotracheal intubation in patients undergoing cervical spine operationAnesth Analg89519991319132110.1213/00000539-199911000-0004
- Hwan S.JooD. KeithRoseThe intubating laryngeal mask airway with and without fiberoptic guidanceAnesth Analg199988
- W.ErlacherH.TiefenbrunnerT.KästenbauerS.SchwarzR.D.FitzgeraldCobraPLUS and Cookgas air-Q versus Fastrach for blind endotracheal intubation: a randomized controlled trialEur J Anaesthesiol282011181186
- B.WaltlM.MelischekC.SchuschnigB.KabonW.ErlacherC.NaselM.FuchsS.KapralAnaesthesia562001221226
- R.E.GalgonK.M.SchroederS.HanA.AndreiA.M.JoffeThe air-Q® intubating laryngeal airway vs the LMA-ProSeal™Anaesthesia6612201110931100
- N.JagannathanR.J.KozlowskiL.E.SohnK.E.LangenA.G.RothI.I.MukherjiM.F.KhoS.SureshClinical evaluation of the intubating laryngeal airway as a conduit for tracheal intubation in childrenAnesth Analg11212011176182
- A.SahinM.A.SalmanI.A.ErdenU.AyparUpper cervical vertebrae movement during intubating laryngeal mask, fibreoptic and direct laryngoscopy: a video-fluoroscopic studyEur J Anaesthesiol212004819823
- Randolph H.HastingsA. ChristopherVigilRichardHannaBor-YauYangDavid J.SartorisCervical spine movement during laryngoscopy with the Bullard, MacIntosh, and Miller LaryngoscopesSurv Anesthesiol4041996251
- Nolan JP, Wilson ME. An evaluation of the gum elastic bougie Intubation times and incidence of sore throat. Article first published online: 22 Feb 2007. http://doi:10.1111/j.1365-2044.1992.tb03154.x.