Abstract
Objectives
Evaluation of fluid responsiveness of septic shock patients admitted to surgical ICU and the predictability of non-invasive monitoring and estimated lactate/pyruvate (L/P) ratio for survival of these patients.
Patients and methods
The study included 58 septic shocked patients admitted and managed at surgical ICU. After non-invasive determination of baseline hemodynamic data and calculation of shock index (SI-0) and Pleth variability index (PVI-0), all patients received intravenous colloid infusion followed 15-min later by non-invasive re-evaluation for SI-15 and PVI-15. Blood samples were obtained for estimation of blood lactate and pyruvate levels at admission (BLL-0 and BPL-0) and 12-h after fluid resuscitation (BLL-12 and BPL-12) and L/P ratio was calculated. All patients were managed according to the Surviving Sepsis Campaign guidelines and followed up for ICU mortality rate (MR).
Results
ICU stay MR was 20.7%. Survival showed negative significant correlation with PVI, L/P ratio and BLL, while it showed positive significant correlation with BPL. Receiver Operating Characteristic (ROC) curve analysis defined baseline and persistently low PVI, high BLL and L/P ratio as significant sensitive predictors for MR, while elevated BPL-12 as significant specific predictor for survival. Regression analysis defined persistently elevated L/P ratio as the highly significant specific predictor, while persistently disturbed SI and PVI could predict mortality as screening tests. Odds ratio for mortality at BLL-0 of >2 mmol/L was 0.0321 (95% CI: 0.0037–0.2755), while it was 4.1111 (95% CI: 1.0702–15.792) at BLL-0 >4 mmol/L.
Conclusion
After fluid resuscitation and hemodynamic stability, persistently elevated BLL could predict mortality, while elevated BPL could predict survival of septic shock patients. Continuous non-invasive evaluation of fluid responsiveness judged by PVI and SI could provide sensitive screening for survival outcome of shocked patients. Wider scale comparative studies are mandatory for establishment of discriminative PVI and BLL cutoff points for prediction of survival of shocked patients.
1 Introduction
Shock is a life-threatening syndrome of acute circulatory failure. It can be caused by loss of intravascular volume, obstruction of flow through the vascular compartment, or a generalized state of vasodilation [Citation1]. Shock leads to decreased organ perfusion, with inadequate delivery of oxygenated blood to tissues and resultant end-organ dysfunction [Citation2].
Sepsis is a systemic response to infection, which may progress to severe sepsis and septic shock [Citation3]. Septic shock causes vascular dysregulation making tissue perfusion dependent on blood pressure. Furthermore, microvascular perfusion could be disrupted by circulating inflammatory mediators that directly damage the peripheral vascular bed [Citation4]. Microcirculatory dysfunction has been documented in the early phase of sepsis and its severity has been related to poor outcome [Citation5].
In critically ill septic patients, early hemodynamic resuscitation was effective to restore macro-hemodynamia and myocardial contractility. Fluid responsiveness is defined by a cardiac preload challenge by fluid infusion resulting in augmented stroke volume and cardiac output [Citation6]. Currently, both static and dynamic parameters are utilized for prediction of fluid responsiveness [Citation7].
Static parameters as central venous pressure and pulmonary artery occlusion pressure are much less reliable than dynamic parameters, which are based on respirophasic variation in stroke volume as pulse pressure variation and changes in aortic blood flow. However, most common dynamic parameters are invasive and expensive [Citation8]. Klijn et al. [Citation9] demonstrated that in critically ill septic patients, non-invasively assessed tissue perfusion and oxygenation is not inferior to invasive hemodynamic measurements in monitoring fluid responsiveness.
Mitochondrial function is thought to play a role in sepsis-induced multiple organ failure [Citation10]. In septic patients, inflammatory signaling leads to changes in the phosphorylation state of mitochondrial proteins resulting in a reduction of the mitochondrial membrane potential, and consequently a lack of energy, which can cause organ failure and death [Citation11]. Septic shock induced a severe hypotension in association with metabolic acidosis and significantly decreased rates of mitochondrial oxygen consumption, activity and content of cytochrome c oxidase [Citation12].
The blood lactate-to-pyruvate (L/P) molar ratio reflects the equilibrium between product and substrate of the reaction catalyzed by lactate dehydrogenase that favors lactate production and normally maintains a constant L/P ratio of about 10:1 [Citation13]. The L/P ratio is correlated with the cytoplasmic ratio between the reduced and oxidized forms of nicotinamide adenine dinucleotide (NADH:NAD+) and is used as a surrogate measure of the cytosolic oxido-reduction state. Impaired cellular respiration, as in hypoxia, causes reduced pyruvate oxidation, resulting in lactic acidosis and increased L/P ratio [Citation14]. Romijn et al. [Citation15] using isotopic tracer found pyruvate and lactate tracer-to-tracer ratios equilibrated almost completely within 3–4 min in whole blood, thus indicating a very rapid lactate clearance.
The current study aimed to evaluate fluid responsiveness of septic shock patients admitted to surgical ICU and the predictability of non-invasive monitoring and estimated lactate/pyruvate (L/P) ratio for survival of these patients.
2 Patients and methods
The current prospective multi-center study was conducted at surgical ICU centers at Cairo University Hospitals, Naser Institute, Al-Marwa and Demascus private centers since January 2014 till June 2015. The study protocol was approved by the Local Ethical Committee of Cairo University Hospitals and written fully informed consents were signed by near patients’ relatives.
Patients inclusion relied on shock definition as hypoperfusion of tissues and/or organs manifested as systolic blood pressure (SBP) of ⩽90 mmHg, heart rate (HR) increased by ⩾10% from baseline, urine output (UOP) of <0.5 ml/kg/min for >2 h, presence of skin mottling; and/or blood lactate level of >2 mmol/L [Citation16]. Sepsis was diagnosed depending on the presence of at least two of the four systemic inflammatory response syndrome (SIRS) criteria and fulfilled the requirements for either severe sepsis or septic shock. SIRS criteria include body temperature <36 °C or >38 °C, heart rate (HR) > 90 beats/min, respiratory rate >20 breaths/min or, an arterial partial pressure of CO2 <32 mmHg and/or white blood cell count <4000 cells/mm3 or >12,000 cells/mm3, or the presence of greater than 10% immature neutrophil band forms. Requirements for severe sepsis patients included the following: (i) fulfilling at least 2 or more of SIRS criteria, (ii) an associated or suspected source of infection, and (iii) it has one or more of the following: evidence of end organ damage, serum lactate levels of ⩾4 mg/dL, and episode of hypotension (<90/60 mmHg), which responds to initial fluid resuscitation. Septic shock patients must have the diagnostic criteria for severe sepsis but blood pressure was persistently <90/60 mmHg and did not respond to adequate fluid resuscitation [Citation17].
Clinical evaluations entail collection of demographic data including age, gender, and body mass index data. Body injury severity was assessed using scoring on the anatomical abbreviated injury scale and the scores of the three most severely injured body regions were squared and added together to produce the injury severity scale (ISS) score ranking from 0 to 75 indicating unsurvivable injury [Citation18]. Acute physiology and chronic health evaluation II (APACHE II) [Citation19] and Glasgow Coma Scale (GCS) [Citation20] scores were also determined.
Patients were continuously non-invasively monitored for electrocardiogram, blood pressures (SBP, DBP and MAP), HR and temperature. Severity of hemodynamic compromise was evaluated using the shock index (SI) defined as systolic blood pressure divided by heart rate, with a normal range of 0.5–0.7 in healthy adults [Citation21].
A reusable Rad7 sensor was attached to the index or middle fingertip, and the sensor was covered with a black, opaque protector to reduce the interference by the surrounding lights, as recommended by the manufacturer. Then the sensor was connected to the Masimo Radical 7 device equipped with a software ver. 7.8.0.1 (Masimo Corp., Irvine, CA, USA). Rad7 device continuously non-invasively measures total hemoglobin (SpHb) and perfusion index (PI) which is the ratio of nonpulsatile to pulsatile blood flow through the peripheral capillary bed as it can influence SpHb measurement accuracy [Citation22]. Pleth variability index (PVI) is an automatic measure of the dynamic change in PI that occurs during the respiratory cycle. PVI = (PI maximum–PI minimum) divided by PI maximum; thus, PVI is a representative measure for PI change and helps to predict fluid responsiveness [Citation23].
Venous blood samples were obtained by venipuncture under complete aseptic conditions and without use of tourniquet. One sample was taken anaerobically in 3-ml heparinized syringes and analyzed on a bedside blood gas machine. Another blood samples were taken and divided into three parts:
| 1. | The first part was collected in sodium fluoride tubes for estimation of blood lactate level using Beckman Coulter analyzers by an end-point enzymatic reaction [Citation24]. | ||||
| 2. | One ml of blood was put in tube containing 2.5 ml of 6% perchloric acid prechilled prior to draw for measurement of blood pyruvate level manually by an end-point enzymatic assay with lactate dehydrogenase and oxidation of NADH to NAD+ with spectrophotometry [Citation25]. Then, lactate/pyruvate (L/P) ratio was calculated. | ||||
| 3. | The third part was put in EDTA tube (about 1.8 mg trik EDTA/1 ml blood) for at once hemoglobin estimation and complete blood count. | ||||
3 Management
For all patients after obtaining preliminary baseline measurements, intravenous volume expansion was conducted with rapid infusion, over 10 min, of 500 ml of available colloid solution and then all hemodynamic measurements were re-evaluated 5-minutes after the end of infusion, to determine the response for volume expansion [Citation26]; then, patients were managed according to the response.
Patients were managed according to the Surviving Sepsis Campaign guidelines [Citation27]. Briefly, fluid resuscitation was conducted using crystalloid given at a minimum rate of 30 ml/kg [Citation26] according to dynamic indices of preload as judged by PI and PVI. Norepinephrine (NE) was used as the first line vasopressor in a dose of 0.05–0.24 μg/kg/min in order to achieve a MAP of 65 mmHg or achieve increased SBP by ⩾20 mmHg [Citation28]. Positive inotropes using dobutamine infusion, starting with an initial dosage of 5 microg × kg × min, increased to a maximum of 10 μg/kg/min [Citation29] for patients with low cardiac index. Vasopressin (up to 0.03 U/min) can be added to norepinephrine with the intent of raising MAP to target or decreasing norepinephrine dosage [Citation26]. Hydrocortisone was started with a loading dose of 100 mg given within 30 min and followed by a continuous infusion of 0.18 mg/kg/h. When septic shock had been reversed, the dose of hydrocortisone was reduced to 0.08 mg/kg/h. This dose was kept constant for 6 days. As soon as the underlying infection had been treated successfully or sodium serum concentrations had increased to >155 mmol/L, the hydrocortisone infusion was tapered in steps of 24 mg/day [Citation30]. Renal replacement therapy was used only in patients exhibiting anuria or elevated potassium levels. The ambient temperature of the room was consistent at approximately 23–25 °C (climate controlled).
4 Statistical analysis
Considering sepsis, severe sepsis and septic shock is not so frequent surgical complication and to properly evaluate the predictors for survival as primary outcome, sample size was calculated using the standard nomogram proposed by Kraemer and Theimann [Citation31] and a sample size of 50 patients was determined to be sufficient to detect a difference at the 5% significance level and give the trial 80% power [Citation32]. Sample size and power were re-calculated and assured using Power and Sample Size Calculation Software program provided by Department of Biostatistics, Vanderbilt University.
Obtained data were presented as mean with standard deviation, median with IQR at 25% and 75% levels, numbers and percentages. Results were analyzed using Wilcoxon ranked test for unrelated data (Z-test) and Chi-square test (X2 test) for non-parametric analysis of numbers and ratios. Estimated parameters were evaluated as predictors from mortality using the receiver operating characteristic (ROC) curve analysis judged by the area under the curve (AUC) compared versus the null hypothesis that AUC = 0.05. Regression analysis (Stepwise method) was used for stratification of studied parameters as specific predictors. Statistical analysis was conducted using the SPSS (Version 15, 2006; SPSS Inc., Chicago, IL, USA) for Windows statistical package. P value <0.05 was considered statistically significant.
5 Results
The study included 58 septic shocked patients admitted to surgical ICU; demographic and preliminary clinical examination data are shown in . Throughout ICU stay 12 patients died, while 46 patients were discharged alive for a mortality rate of 20.7%.
Table 1 Patients’ data at admission (n = 58).
Mean SI estimated after trial fluid infusion (SI-15) was significantly (p < 0.05) lower compared to at admission SI (SI-0). Mean estimated SI-0 and SI-15 showed non-significant (p > 0.05) difference between survivors and non-survivors (). However, the frequency of survivors among those who had IS-0 in range of 0.5–0.7 was significantly higher after fluid resuscitation than those at admission frequency and in comparison with frequency among non-survivors after resuscitation. Mean PVI-15 was significantly (p < 0.05) higher compared to PVI-0 in both survivors and non-survivors. However, mean PVI-0 and PVI-15 estimates were significantly higher in survivors compared to non-survivors. Moreover, the percentage of change of PVI-15 versus PVI-0 was significantly (p < 0.05) higher in survivors compared to non-survivors (, ).
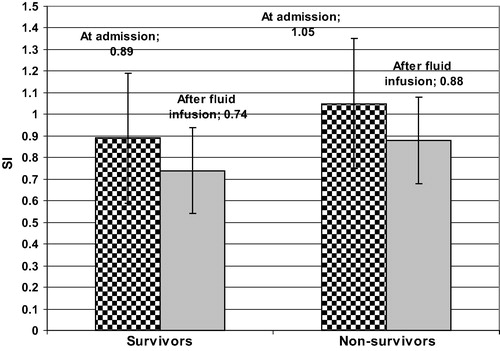
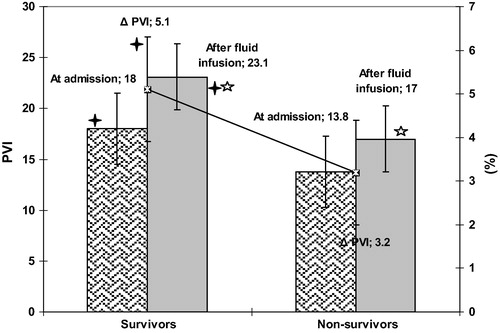
Table 2 SI and PVI data reported at ICU admission and after trial of fluid infusion of studied patients (n = 58) categorized according to survival.
After infusion trial for evaluation of fluid responsiveness as judged by SI and PVI, all patients received fluid therapy with median amount of 1700 cc received initially and 2500 cc 8 h thereafter. Empirical antibiotic therapy was started once patient was admitted and after obtaining samples: blood and fluid, or exudates if possible for culture and sensitivity test to define the appropriate antibiotic to be given. Forty-two patients (72.4%) received norepinephrine at time of admission and 27 (46.6%) patients required booster dose of norepinephrine 8-h thereafter. Thirteen patients (22.4%) received dobutamine at time of admission and 7 patients (12.1%) required a booster dose at 8-h thereafter. Steroid and vasopressin therapy was required for 32 (55.2%) and 14 patients (24.1%), respectively. Details of received therapeutic lines are shown in .
Table 3 Therapeutic lines received by studied patients at time of catheter insertion and 8-h later.
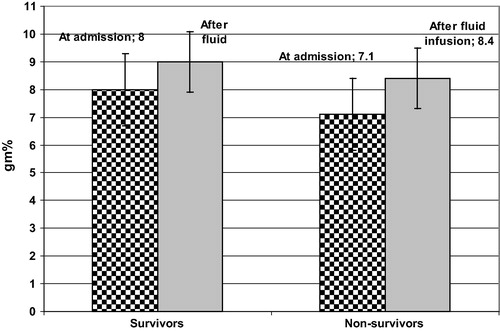
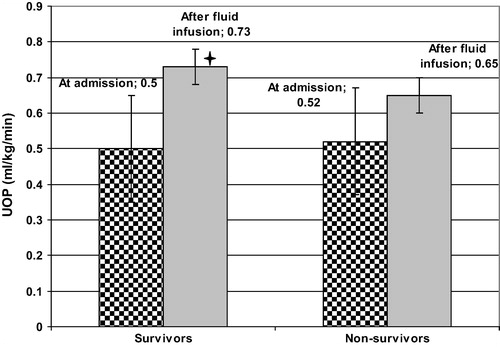
Median hemoglobin concentration was 7.8 g% at ICU admission, so all patients received fresh blood transfusion with median number of transfused units of two units. All patients showed increased post-transfusion hemoglobin concentration with significant (p < 0.05) difference versus at admission concentration, but with non-significant (p > 0.05) difference between survivors and non-survivors (). Mean UOP was significantly (p < 0.05) increased after fluid resuscitation compared to at admission UOP in both survivors and non-survivors. However, mean UOP after fluid resuscitation was significantly (p < 0.05) higher in survivors than in non-survivors ().
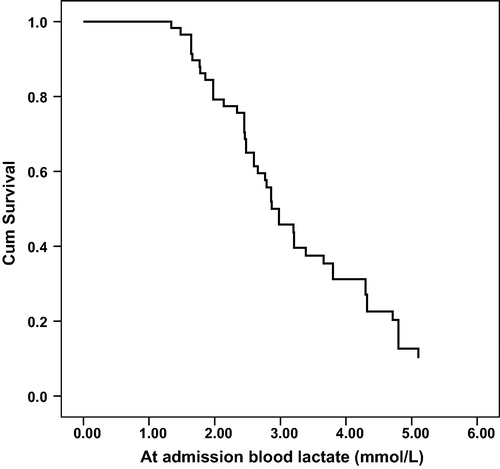
Blood lactate levels estimated at time of admission (BLL-0) were significantly (p < 0.05) higher in non-survivors compared to BLL-0 of survivors. On contrary, blood pyruvate levels (BPL-0) were non-significantly (p > 0.05) lower in non-survivors compared to survivors. Fluid resuscitation significantly (p < 0.05) reduced BLL estimated at 12-h after admission (BLL-12) in both survivors and non-survivors compared to at admission levels. However, BLL-12 was significantly (p < 0.05) lower, while BPL-12 was significantly (p < 0.05) higher in survivors compared to non-survivors. Estimated L/P ratio after fluid resuscitation (L/P-12) was significantly lower in both survivors and non-survivors compared to at admission ratios (L/P-0). Estimated L/P ratios were significantly (p < 0.05) higher in non-survivors compared to survivors (, ). Eleven non-survivors and 34 survivors (73.9%) had BLL-0 >2 mmol/L, with Odds ratio (OR) for survival of 0.0321 (95% CI: 0.0037–0.2755). On contrary, 6 non-survivors (50%) and only 9 survivors (19.6%) had BLL-0 >4 mmol/L, with OR of 4.1111 for mortality (95% CI: 1.0702–15.792) ().
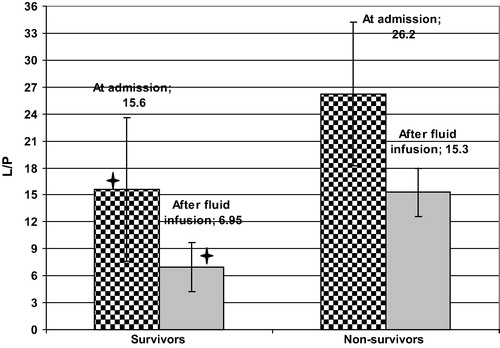
Table 4 Laboratory data reported at ICU admission and after fluid resuscitation of studied patients categorized according to survival.
Survival of shocked patients showed negative significant correlation with PVI-0, L/P-0 ratio and BLL-0 in decreasing order of significance, while it showed positive significant correlation with BPL-0. After fluid resuscitation, patients’ survival showed negative significant correlation with L/P-12 ratio, PVI-15, BLL-12 and SI-15 in decreasing order of significance, while it showed positive significant correlation with BPL-12 and UOP-12 in decreasing order of significance (). BLL-12 estimated 12-h after fluid resuscitation showed negative significant correlation with UOP-12 (r = −0.436, p = 0.001).
Table 5 Correlation between survival (n = 46) and evaluated parameters.
Among studied parameters evaluated at time of ICU admission, Receiver Operating characteristic (ROC) curve analysis defined low PVI-0, but high BLL-0 and L/P-0 ratio as sensitive significant predictors for mortality during ICU stay. After fluid resuscitation, ROC curve analysis defined persistently elevated BLL-12 and L/P-12 ratio, while low PVI-15 as sensitive significant predictors for mortality. On contrary, elevated BPL-12 after fluid resuscitation was defined as significant specific predictor for survival during ICU stay ().
Table 6 Receiver operating characteristic curve analysis of evaluated parameters as predictors for survival (n = 46).
Among studied parameters Regression analysis defined persistently elevated L/P ratio after fluid resuscitation and establishment of stable hemodynamic variables as the highly significant specific predictor for ICU mortality of septic shocked patients. Persistently disturbed PVI indicating unfavorable fluid responsiveness could predict mortality as screening test that was positive in two analysis models. Also, persistently high SI despite fluid resuscitation was significant screening test for mortality during ICU stay ().
Table 7 Regression analysis of SI, PVI and L/P as predictors for survival (n = 46).
6 Discussion
Fluid resuscitation significantly improved shock index (SI) and the frequency of survivors with SI in range of 0.5–0.7 after fluid resuscitation was significantly higher compared to non-survivors and persistently elevated SI predicts mortality with AUC of 0.670. In line with these findings, Berger et al. [Citation33] reported that SI ⩾ 0.7 could predict the presence of severe sepsis and was the most sensitive screening test, while SI ⩾ 1.0 was the most specific predictor for 28-day mortality. Wira et al. [Citation34] found that 47.5% of patients with severe sepsis had sustained SI elevation after fluid resuscitation and 38.6% of these patients required vasopressors within 72 h versus 11.6% of patients without sustained SI elevation and the mean number of organ failures was 4 and 3.2 in patients with and without sustained SI elevation, respectively. McCall et al. [Citation35] reported that SI at extremely high and low values could predict stroke mortality and very early (3-day) mortality.
All patients showed significantly improved PVI after fluid therapy compared to PVI-0 with significant difference in favor of survivors. PVI measurements showed positive significant correlation with survival and were defined as significant predictors for survival on ROC curve analysis. These findings indicate the applicability of PVI as sensitive parameter for non-invasive continuous monitoring of fluid responsiveness, despite being less specific and go in hand with Loupec et al. [Citation23] who found PVI changes significantly correlated with the percentage change in cardiac output after fluid challenge and PVI at 17% can discriminate responders from non-responders with 95% sensitivity and 91% specificity rates.
Feissel et al. [Citation36] reported that in septic patients PVI values were significantly higher in responders to hydroxylethyl starch infusion vs. non-responders with significant correlation with the percent changes induced by intervention in aortic velocity-time integral measured using transthoracic echocardiography and PVI at 19% discriminates responders from non-responders with sensitivity, specificity and AUC of 94%, 87% and 0.97, respectively. Siswojo et al. [Citation37] reported that pulse oximeter derived from baseline PVI and stroke volume index derived from esophageal Doppler were significantly different between responders and non-responders to fluid intervention and baseline PVI at 10.5% could predict fluid responsiveness with sensitivity and specificity of 88% and 67%, respectively and AUC of 0.84.
Recently, Yu et al. [Citation38] found PVI-based goal-directed fluid management can reduce the intraoperative fluid amount especially the crystalloid and blood lactate levels in patients under general-epidural anesthesia. Chu et al. [Citation39] through systemic literature review reported sensitivity and specificity rates of 73% and 82%, respectively for PVI to predict fluid responsiveness in mechanically ventilated patients with no heterogeneity within nor between studies and concluded that PVI has reasonable ability to predict fluid responsiveness.
On contrary, Bahlmann et al. [Citation40] found pulse oximetric PVI- and esophageal Doppler-based stroke volume optimizations agreed poorly and did not affect the amount of fluid administered, and none of both algorithms showed a good ability to predict fluid responsiveness and concluded that these results do not support the fluid responsiveness concept.
These discrepancies concerning predictability of PVI to fluid responsiveness could be attributed to the fact that the concept is still recently involved in researches and not examined in wider scale comparative studies and to the variability of choice of the comparative cutoff point for PVI [Citation23,Citation36,Citation37,Citation40] and the choice of counter comparative method [Citation36,Citation37,Citation40].
Fluid resuscitation significantly reduced blood lactate level (BLL) and calculated L/P ratio with still significantly higher L/P ratio in non-survivors compared to survivors. Persistently elevated BLL and high L/P ratios were found to be the most significant predictors for mortality. The reported decreased BLL may be attributed to increased lactate clearance as evidenced by significantly higher UOP after fluid resuscitation compared to at admission UOP. Also, UOP showed negative significant correlation with BLL. Both decreased BLL and increased UOP supported the findings concerning PVI and indicated improved tissue perfusion, thus supporting the concept of fluid responsiveness. In line with this attribution, Burša and Pleva [Citation41] suggested that in traumatic hemorrhagic shock patients, L/P ratio is useful to identify tissue ischemia and can estimate the effectiveness of fluid resuscitation and an increase in L/P ratio is an early warning sign of inadequate tissue oxygenation and should lead to more detailed hemodynamic and laboratory monitoring. Burša et al. [Citation42] also suggested that L/P ratio could be a useful transfusion trigger. Dezman et al. [Citation43] found that among patients with elevated BLL that did not decline to <2 mmol/L in response to resuscitative efforts, the mortality rate was nearly seven times higher than that among those with an elevated BLL that normalized and logistic regression analysis showed that failure to clear lactate was associated with death more than any other feature.
Improved mitochondrial function as evidenced by the increased blood pyruvate after fluid resuscitation compared to at admission levels, may explain the reported decreased BLL and L/P ratio especially in survivors and was found to be significant specific predictor for survival. In support of this assumption, Nuzzo et al. [Citation44] found pyruvate dehydrogenase (PDH) activity and quantity in septic patients were significantly lower than in healthy controls and in non-survivor compared to survivors and concluded that PDH activity and quantity are low in sepsis, and this may cause cells to shift to anaerobic metabolism, resulting in increased lactate and decreased pyruvate production.
Interestingly, 11 of non-survivors (91.7%) and 34 of survivors (73.9%) had at admission BLL >2 mmol/L, while 6 of non-survivors (50%) and only 9 of survivors (19.6%) had BLL >4 mmol/L; a finding indicating that for differentiation between survivors and non-survivors, a cutoff point of 2 mmol/L is non-sense while 4 mmol/L had higher predictivity. In support of such finding Datta et al. [Citation45] found that the odds ratios for 30-day death, compared to lactate ⩾4, were 0.125 for lactate <2 and 0.273 for lactate 2–<4. Casserly et al. [Citation46] documented BLL >4 mmol/L is significantly associated with in-hospital mortality than BLL of 2–3 and 3–4 mmol/L, thus supporting the use of the cutoff of >4 mmol/L as a qualifier for future trials in severe sepsis or septic shock.
In support of the rational suggestion to rely on multiple parameters for early prediction of outcome of shocked ICU patients, Cevik et al. [Citation47] found that in patients who had elevated BLL and SI, the use of mechanical ventilation and vasoactive drug was significantly higher with higher hospitalization rate and in-hospital mortality (54.1%) than in patients who had elevation of either parameter alone and concluded that combination of both parameters is effective in predicting these outcome measures with higher sensitivities and NPV. Shackelford et al. [Citation48] reported that automated analysis of triage vital signs, 15 min of pulse oximetry signals, and laboratory values including BLL predicted use of blood transfusion during trauma resuscitation more accurately than triage vital signs or pulse oximetry analysis alone.
It could be concluded that after fluid resuscitation and hemodynamic stability, persistently elevated BLL could predict mortality, while elevating BPL could positively predict survival of septic shock patients admitted to ICU. Continuous non-invasive evaluation of fluid responsiveness judged by PVI and SI could provide sensitive screening for survival outcome of shocked patients. Wider scale comparative studies are mandatory for establishment of discriminative PVI and BLL cutoff points for prediction of survival of shocked patients.
Conflict of interest
The authors declared that there is no conflict of interest.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- H.VadakelD.RizzoloShock: early recognition and resuscitation are keyJAAPA26620132124
- J.B.RichardsS.R.WilcoxDiagnosis and management of shock in the emergency departmentEmerg Med Pract1632014122
- R.P.DellingerM.M.LevyA.RhodesD.AnnaneH.GerlachS.M.OpalJ.E.SevranskyC.L.SprungI.S.DouglasR.JaeschkeT.M.OsbornM.E.NunnallyS.R.TownsendK.ReinhartR.M.KleinpellD.C.AngusC.S.DeutschmanF.R.MachadoG.D.RubenfeldS.A.WebbR.J.BealeJ.L.VincentR.MorenoSurviving Sepsis Campaign Guidelines Committee including the Pediatric Subgroup Surviving Sepsis Campaign. International guidelines for management of severe sepsis and septic shock: 2012Crit. Care Med.412013580637
- A.SpanosS.JhanjiA.Vivian-SmithT.HarrisR.M.PearseEarly microvascular changes in sepsis and severe sepsisShock3342010387391
- Y.SakrM.J.DuboisD.De BackerJ.CreteurJ.L.VincentPersistent microcirculatory alterations are associated with organ failure and death in patients with septic shockCrit. Care Med.32200418251831
- D.N.NaumannJ.DretzkeS.HutchingsM.J.MidwinterProtocol for a systematic review of the impact of resuscitation fluids on the microcirculation after haemorrhagic shock in animal modelsSyst Rev412015135
- V.A.DinhH.S.KoR.RaoR.C.BansalD.D.SmithT.E.KimH.B.NguyenMeasuring cardiac index with a focused cardiac ultrasound examination in the EDAm. J. Emerg. Med.30201218451851
- C.ChenM.H.KollefConservative fluid therapy in septic shock: an example of targeted therapeutic minimizationCrit. Care182014481
- E.KlijnM.H.van VelzenA.P.LimaJ.BakkerJ.van BommelA.B.GroeneveldTissue perfusion and oxygenation to monitor fluid responsiveness in critically ill, septic patients after initial resuscitation: a prospective observational studyJ. Clin. Monit. Comput.2962015707712
- M.KarlssonN.HaraS.MorataF.SjövallT.KilbaughM.J.HanssonH.UchinoE.ElmérDiverse and Tissue Specific Mitochondrial Respiratory Response in A Mouse Model of Sepsis-Induced Multiple Organ FailureShock2015 Epub ahead of print
- I.LeeM.HüttemannEnergy crisis: the role of oxidative phosphorylation in acute inflammation and sepsisBiochim. Biophys. Acta18429201415791586
- L.LorenteM.M.MartínE.López-GallardoR.IcetaJ.Solé-ViolánJ.BlanquerL.LabartaC.DíazA.JiménezN.LafuenteM.HernándezF.MéndezN.MedinaJ.M.Ferrer-AgüeroJ.FerreresM.C.LLimiñanaM.L.MoraS.LubilloM.Sánchez-PalaciosJ.MontoyaE.Ruiz-PesiniPlatelet cytochrome c oxidase activity and quantity in septic patientsCrit. Care Med.396201112891294
- B.H.RobinsonLactic acidemiaC.R.ScriverA.L.BeaudetW.S.SlyD.ValleThe Metabolic and Molecular Bases of Inherited Disease8th ed.2001McGraw-HillNew York22752295
- F.G.DebrayG.A.MitchellP.AllardB.H.RobinsonJ.A.HanleyM.LambertDiagnostic accuracy of blood lactate-to-pyruvate molar ratio in the differential diagnosis of congenital lactic acidosisClin. Chem.5352007916921
- J.A.RomijnD.L.ChinkesJ.M.SchwarzR.R.WolfeLactate-pyruvate interconversion in blood: implications for in vivo tracer studiesAm. J. Physiol.2663 Pt 11994E334E340
- G.S.HuangM.H.HuN.K.HungC.S.TsaiT.C.LiuW.J.LiawThe current situation and trends in the clinical treatment of shockHu Li Za Zhi.57120101116
- S.J.YussofM.I.ZakariaF.L.MohamedM.A.BujangS.LakshmananA.AsaariValue of Shock Index in Prognosticating The Short Term Outcome of Death for Patients Presenting With Severe Sepsis and Septic Shock in The Emergency DepartmentMed. J. Malaysia6742012406411
- W.S.CopesH.R.ChampionW.J.SaccoThe Injury Severity Score revisitedJ. Trauma28119956977
- W.A.KnausE.A.DraperD.P.WagnerJ.E.ZimmermanAPACHE II: a severity of disease classification systemCrit. Care Med.131985818829
- G.TeasdaleB.JennettAssessment and prognosis of coma after head injuryActa Neurochir.3419764555
- R.H.BirkhahnT.J.GaetaD.TerryJ.J.BoveJ.TloczkowskiShock index in diagnosing early acute hypovolemiaAm. J. Emerg. Med.2332005323326
- B.V.NguyenJ.L.VincentE.NowakM.CoatN.PaleironP.GounyM.Ould-AhmedM.GuillouetC.C.ArvieuxG.GueretThe accuracy of noninvasive hemoglobin measurement by multiwavelength pulse oximetry after cardiac surgeryAnesth. Analg.1135201110521057
- T.LoupecH.NanadoumgarD.FrascaF.PetitpasL.LaksiriD.BaudouinB.DebaeneC.Dahyot-FizelierO.MimozPleth variability index predicts fluid responsiveness in critically ill patientsCrit. Care Med.3922011294299
- K.WassermanW.L.BeaverJ.A.DaviesJ.Z.PuD.HeberB.J.WhippLactate, pyruvate and lactate-to-pyruvate ratio during exercise and recoveryJ. Appl. Physiol.5931985935940
- C.K.ChungT.J.WangC.Y.YeungW.S.HsiehD.S.LinS.C.HoS.P.LinInterference and blood sample preparation for pyruvate enzymatic assayClin. Biochem.3920067477
- R.P.DellingerM.M.LevyJ.M.CarletJ.BionM.M.ParkerR.JaeschkeK.ReinhartD.C.AngusC.Brun-BuissonR.BealeT.CalandraJ.DhainautH.GerlachM.HarveyJ.J.MariniJ.MarshallM.RanieriG.RamsayJ.SevranskyB.T.ThompsonS.TownsendJ.S.VenderJ.L.ZimmermanJ.VincentSurviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008Crit. Care Med.362008296327
- M.LeoneI.BoyadjievE.BoulosF.AntoniniP.VisintiniJ.AlbanèseC.MartinA reappraisal of isoproterenol in goal-directed therapy of septic shockShock262006353357
- T.FukuokaM.NishimuraH.ImanakaN.TaenakaI.YoshiyaJ.TakezawaEffects of norepinephrine on renal function in septic patients with normal and elevated serum lactate levelsCrit. Care Med.1711198911041107
- W.SchaffartzikC.SanftJ.H.SchaeferC.SpiesDifferent dosages of dobutamine in septic shock patients: determining oxygen consumption with a metabolic monitor integrated in a ventilatorIntensive Care Med.2612200017401746
- J.BriegelH.ForstM.HallerG.SchellingE.KilgerG.KupratB.HemmerT.HummelA.LenhartM.HeyduckC.StollK.PeterStress doses of hydrocortisone reverse hyperdynamic septic shock: a prospective, randomized, double-blind, single-center studyCrit. Care Med.2741999723732
- H.C.KraemerS.TheimannHow many subjects? Statistical power analysis in research1987SageNewbury Park, CA
- K.R.MurphyB.MyorsStatistical Power Analysis: A Simple and General Model for Traditional and Modern Hypothesis Tests2nd ed.2003Lawrence Erlbaum Associates, Inc
- T.BergerJ.GreenT.HoreczkoY.HagarN.GargA.SuarezE.PanacekN.ShapiroShock index and early recognition of sepsis in the emergency department: pilot studyWest J Emerg Med.1422013168174
- C.R.WiraM.W.FrancisS.BhatR.EhrmanD.ConnerM.SiegelThe shock index as a predictor of vasopressor use in emergency department patients with severe sepsisWest J Emerg Med.15120146066
- S.J.McCallS.D.MusgraveJ.F.PotterR.HaleA.B.ClarkM.A.MamasA.K.MetcalfD.J.DayE.A.WarburtonM.O.BachmannMyint PK; Anglia Stroke Clinical Network Evaluation Study (ASCNES) Group. The shock index predicts acute mortality outcomes in strokeInt. J. Cardiol.1822015523527
- M.FeisselR.KalakhyP.BanwarthJ.BadieA.PavonJ.P.FallerJ.P.QuenotPlethysmographic variation index predicts fluid responsiveness in ventilated patients in the early phase of septic shock in the emergency department: a pilot studyJ. Crit. Care2852013634639
- A.S.SiswojoD.M.WongT.D.PhanR.KlugerPleth variability index predicts fluid responsiveness in mechanically ventilated adults during general anesthesia for noncardiac surgeryJ. Cardiothorac. Vasc. Anesth.286201415051509
- Y.YuJ.DongZ.XuH.ShenJ.ZhengPleth variability index-directed fluid management in abdominal surgery under combined general and epidural anesthesiaJ. Clin. Monit. Comput.29120154752
- H.ChuY.WangY.SunG.WangAccuracy of pleth variability index to predict fluid responsiveness in mechanically ventilated patients: a systematic review and meta-analysisJ. Clin. Monit. Comput.2015 Epub ahead of print
- H.BahlmannR.G.HahnL.NilssonAgreement between Pleth Variability Index and oesophageal Doppler to predict fluid responsivenessActa Anaesthesiol. Scand.201510.1111/aas.12632
- F.BuršaL.PlevaAnaerobic metabolism associated with traumatic hemorrhagic shock monitored by microdialysis of muscle tissue is dependent on the levels of hemoglobin and central venous oxygen saturation: a prospective, observational studyScand J Trauma Resusc Emerg Med.22201411
- F.BuršaL.PlevaJ.MácaP.SklienkaP.ŠevčíkTissue ischemia microdialysis assessments following severe traumatic haemorrhagic shock: lactate/pyruvate ratio as a new resuscitation end point?BMC Anesthesiol.142014118
- Z.D.DezmanA.C.ComerG.S.SmithM.NarayanT.M.ScaleaJ.M.HirshonFailure to clear elevated lactate predicts 24-hour mortality in trauma patientsJ Trauma Acute Care Surg.7942015580585
- E.NuzzoK.M.BergL.W.AndersenJ.BalkemaS.MontissolM.N.CocchiX.LiuM.W.DonninoPyruvate Dehydrogenase Activity is Decreased in the Peripheral Blood Mononuclear Cells of Patients with Sepsis: A Prospective Observational TrialAnn Am Thorac Soc.2015 Sep 10. [Epub ahead of print]
- D.DattaC.WalkerA.J.GrayC.GrahamArterial lactate levels in an emergency department are associated with mortality: a prospective observational cohort studyEmerg Med J.3292015673677
- B.CasserlyG.S.PhillipsC.SchorrR.P.DellingerS.R.TownsendT.M.OsbornK.ReinhartN.SelvakumarM.M.LevyLactate measurements in sepsis-induced tissue hypoperfusion: results from the Surviving Sepsis Campaign databaseCrit. Care Med.4332015567573
- A.A.CevikH.DolgunS.OnerB.TokarN.AcarE.OzakinF.KayaElevated lactate level and shock index in nontraumatic hypotensive patients presenting to the emergency departmentEur J Emerg Med.22120152328
- S.ShackelfordS.YangP.HuC.MillerA.AnazodoS.GalvagnoY.WangL.HartskyR.FangC.MackenzieONPOINT Study Group. Predicting blood transfusion using automated analysis of pulse oximetry signals and laboratory valuesJ Trauma Acute Care Surg.794 Suppl 22015S175S180