Abstract
Background
Pediatric cardiac anesthesia involves anaesthetizing very small children with complex congenital heart disease. Sevoflurane provides the advantage of rapid induction of anesthesia with short recovery time. Ketofol is a neologism coined to refer to the combination of ketamine and propofol mixed together in one syringe. Ketamine and propofol have opposing influences on blood pressure, heart rate, and SVR.
Aim of the work
To compare the effectiveness and side effects of ketofol versus sevoflurane for maintenance of aesthesia in pediatric cardiac catheterization.
Methods
This double blinded randomized study was carried on 90 pediatric patients ASA II and III undergoing cardiac catheterization. Induction was accomplished with titration of 3–5% sevoflurane. Patients were randomly assigned to one of the two study groups. Group K received ketofol mixture (propofol, 4 mg/mL, and ketamine, 2 mg/mL) infusion rate propofol 25–50 mic/kg/min and ketamine 12.5–25 mic/kg/min for maintenance. Group S received sevoflurane 0.5–1 MAC. Changes in recovery time, hemodynamic variables and the incidence of adverse effects were measured.
Results
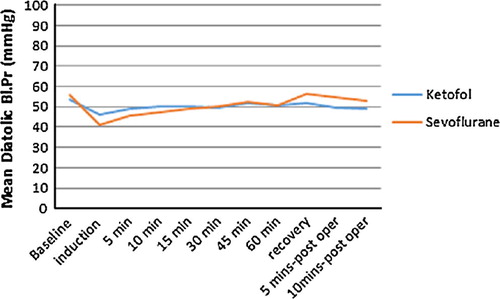
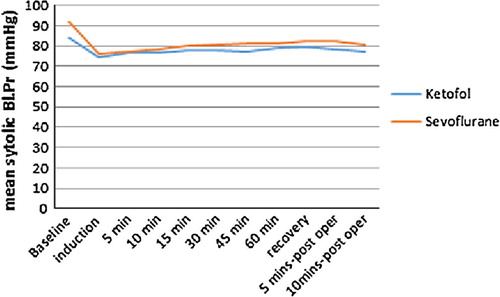
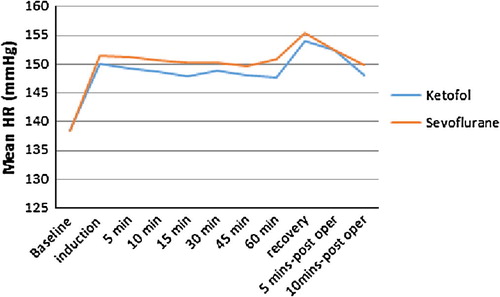
Diastolic blood pressure showed significant difference between the study groups at induction p (0.001), 5 min after induction p(0.04), on recovery 0.037, 5 min postoperatively p(0.016), and 10 min postoperatively. The need for vasopressor and MAP decrease >20% compared with baseline did not show significant difference p(0.832). Recovery time was shorter in group S p(.000). The incidence of nausea and vomiting was significantly more in group S p(.000). Emergence agitation was observed in group S in 12(26.6) patients. Watcha scale was significantly lower in group K at 10 min postoperatively p(.001).
Conclusions
Both propofol–ketamine and sevoflurane provided effective sedation and analgesia during pediatric cardiac catheterization. But propofol–ketamine combination was superior to sevoflurane because the incidence of agitation, nausea and vomiting in patients given sevoflurane was significantly higher than in ketofol group.
Introduction
Pediatric cardiac anesthesia involves anaesthetizing very small children with complex congenital heart disease. The unique nature of this patient population produces challenges for the anesthetist because of their altered physiology. The goals of anesthetic management during cardiac catheterization are adequate sedation, analgesia, and immobility. The agents used should have a minimal influence on cardiac function and respiratory drive [Citation1].
A wide variety of pharmacologic agents and techniques have been successfully used for these procedures. Sevoflurane provides the advantage of rapid induction of anesthesia with short recovery time [Citation2]. Ketofol is a neologism coined to refer to the combination of ketamine and propofol mixed together in one syringe. These two drugs are pharmacologically compatible [Citation3,Citation4], and this combination has been used widely for surgical anesthesia. Ketamine and propofol have opposing influences on blood pressure, heart rate, and systemic vascular resistance (SVR). In addition, ketamine supplementing a propofol infusion has been shown to preserve respiratory function and upper airway control in several studies. There has been a growing interest in this mixture for anesthesia in both children [Citation5–Citation10] and adults [Citation11–Citation13], subsequent to reports of earlier discharge and less vomiting and adverse events after procedural sedation and analgesia. Propofol total intravenous anesthesia (TIVA) is an effective and well-tolerated anesthetic technique that allows smooth induction and rapid recovery, making it ideal for procedural sedation of children [Citation14–Citation16]. However, approximately 3.7% of children experience emergence agitation (EA) after propofol TIVA [Citation17,Citation18]. This frequency is considerably lower than that reported with sevoflurane (23.1%) [Citation18].
The aim of this study was to compare two anesthetic regimens: sevoflurane and ketofol as maintenance anesthesia in pediatric patients suffering from congenital heart disease. The primary outcome was to compare the hemodynamic effects of sevoflurane and ketofol as maintenance anesthesia. A significant change more than 20% compared with baseline values for mean arterial blood pressure was defined as clinically important. The secondary Outcome was to compare the side effects and the incidence of agitation on recovery between the two study groups.
Methods
The Alexandria university ethics committee approved the study, and written informed consent was obtained from patients’ parents. The study sample included 90 children aging 1 month to 4 years with American Society of Anesthesiologists grade II to III scheduled for elective cardiac catheterization between August 2015 and November 2015 in Alexandria University Hospital. This trial was registered in Pan African Clinical Trial Registry (PACTR) with identification number PACTR201605001606658. Patients suffering major endocrinal, respiratory, renal or hepatic disorders were excluded. Patients requiring mechanical ventilation, supplemental oxygen, or intravenous inotropic support were also excluded. The procedure was performed after a fasting period of 2 h for clear fluids, 4 h for breast milk and 6 h for light meals. Patients were monitored with electrocardiography, non-invasive blood pressure measurements, and pulse oximetry. Baseline blood pressure and heart rate were obtained before induction. Anesthetic cream was applied to all patients in the preanesthetic holding area 60 min before the procedure. On arrival to catheter room a catheter was placed in a peripheral vein, and lactated Ringer’s solution was infused at the maintenance rate. Blood pressure and heart rate were recorded at baseline and every 5 min during the procedure. Arterial blood gases were checked 5 min after insertion of a catheter in the femoral artery and followed as needed. Induction was accomplished with titration of 3–5% sevoflurane, and a peripheral line was inserted. Patients were randomly assigned using a table of random numbers and sealed envelope assignment to one of the two study groups, and group K anesthesia was induced with ketamine, 1–1.2 mg/kg, and propofol 1–1.2 mg/kg. Ketofol mixture was prepared in a ratio of 1:2 (50 mg ketamine diluted with glucose 5% to reach volume of 10 ml + 100 mg propofol 1%, total volume of 20 ml each ml contain 5 mg propofol +2.5 mg ketamine) infusion rate propofol 25–50 mic/kg/min and ketamine 12.5–25 mic/kg/min for maintenance, and 100% oxygen was given through a tightly fitted face mask. The infusion rate of the propofol and ketamine mixture was changed according to the required depth of anesthesia [Citation1]. Group S received sevoflurane 1–2% according to the required depth of anesthesia in 100% oxygen for maintenance through a tightly fitted face mask, once the procedure started. The patients’ groins were infiltrated with 1% lidocaine for femoral vascular access. The anesthetic drugs were discontinued when the groin bandage was applied. Parameters were recorded by anesthetist unaware of group assignment. Changes in mean arterial pressure (MAP) of more than 20% of awake (baseline) were noted. A vasopressor was given if a 30% decrease in the resting mean arterial blood pressure for 30 s was noted (1 μg/kg bolus of IV phenylephrine). A decrease in oxygen saturation of more than 5% from baseline was also noted. Awakening signs in the patients were monitored according to the modified Steward recovery scoring system [Citation19] by a blinded researcher who did not participate in the catheterization procedure in the operating room. The time to reach a modified Steward score of ⩾6 was recorded. Agitation was measured postoperatively at 10 min intervals by a blinded observer using Watcha scale graded as 0 score (Asleep), 1 score (Calm), 2 score (Crying, but can be consoled), 3 score (Crying, but cannot be consoled), and 4 score (Agitated and thrashing around) [Citation20]. The incidence of adverse effects including nausea, vomiting, apnea episodes (apnea was defined as a pause in breathing for more than 15 s or more than 10 s if associated with oxygen saturation less than 80%) and emergence agitation (Watcha scale 3–4) was noted.
Statistical methods
A power analysis determined that 45 patients per group would be required to detect 20% reduction in mean arterial blood pressure with a power of 81% and a significance level of 0.05 using PASS 2000 program [Citation7]
Statistical analysis was done using IBM SPSS statistics program version 21 and Medcalc program. Quantitative data were described by mean and median as measures of central tendency and Standard deviation, Minimum and maximum as measures of dispersion, while categorical variables were summarized by frequency and percent. Chi-square test was used to study significant association between two categorical variables. Fisher exact and Monte–Carlo tests were used to detect a difference of more than 20% in quantitative parameters in the same group of patients. Independent sample t and Mann–Whitney U-tests were used to detect significant difference in the mean and median quantitative variables respectively between two groups of patients.
Repeated measures ANOVA test was done to detect statistical significant difference of mean quantitative variables along different time periods. We tested homogeneity of variance by Mauchly’s test of sphericity and Huynh–Feldt test was used instead of Conventional F test for significant results. Pairwise comparison was done using adjusted p value after Bonferroni correction.
All statistical tests were done at .05 significance level.
Results
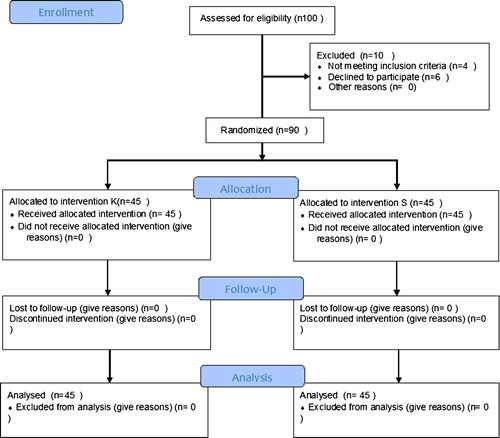
Hundred patients were approached in which 4 were excluded and 6 parents declined to participate in the current study. Ninety patients were recruited in this study, 45 in each group (). There was no statistical difference between the groups regarding weight, age and, medical illness and procedures (). Diastolic blood pressure was significantly lower in group S in comparison with group K after induction, on recovery and postoperatively. In group K there was significant decrease in diastolic blood pressure in comparison with baseline after induction. In Group S there was significant decrease in diastolic blood pressure in comparison with baseline after induction as shown in . Systolic blood pressure and heart rate did not show statistical difference between the study groups at all measured intervals. Systolic blood pressure in both groups showed significant decrease in comparison with base line (). Heart rate did not show statistical difference between the study groups at all measured intervals. Heart rate in both groups showed statistically significant increase in comparison with baseline (). Need for vasopressor and decrease in MAP more than 20% compared with baseline did not show significant difference p(0.832). Recovery time was statistically shorter in group S p(.000). The incidence of nausea and vomiting was significantly more in group S p(.000) (). Post-operative apnea occurred in 2 patients in group S p(0.532) in the first hour postoperatively. Emergence agitation was observed in sevoflurane group in 12 patients p(.000). Watcha scale was significantly lower in group K at 10 min postoperatively p(.001) ().
able 1 Demographic data and patients characteristics.
able 2 Post operative complications.
able 3 Watcha scale.
Discussion
This study included 90 children with American Society of Anesthesiologists grade II to III scheduled for elective cardiac catheterization. We compared two anesthetic regimens: sevoflurane and ketofol as maintenance anesthesia in pediatric patients suffering from congenital heart disease. The main finding of our study was that the incidence of agitation, nausea and vomiting in patients receiving sevoflurane was significantly higher than ketofol group and the change of more than 20% in MAP showed no significant difference between the study groups.
Watcha scale was significantly lower in group ketofol at 10 min postoperatively p(0.001). Incidences of emergency agitation were significantly higher in sevoflurane group p(0.000). Emergence agitation is associated with increased morbidity, hospital costs and delayed discharge. Compared to our results Chandler et al. examined the incidence of Emergence delirium in children following sevoflurane (SEVO) anesthesia and propofol-remifentanil total intravenous anesthesia (TIVA) on one hundred and twelve children. Incidence of ED was higher with SEVO (38.3% vs 14.9%, p = 0.018) [Citation21]. In this study the incidence of nausea and vomiting was significantly more in group S than in group K. A previous meta-analysis study by Joo et al. comparing the characteristics of sevoflurane and propofol for the induction of routine anesthesia concluded that propofol caused less frequent incidence of postoperative nausea and vomiting [Citation22].
In this study 2 patients suffered from postoperative apnea episodes in group S, while none of group K suffered from this complication. The difference in the incidence of postoperative apnea episodes did not reach statistical significance. A previous study by Davidson et al. compering awake regional anesthesia (RA) with sevoflurane general anesthesia in young infants on rates of apnea after anesthesia concluded that RA in infants reduces apnea in the early postoperative period [Citation23]. A previous study examining the effects of ketofol versus propofol on laryngeal mask insertion in children showed preserved hemodynamic stability (mean blood pressure, heart rate) in ketofol group, with less incidence of apnea compared to Propofol group [Citation24]. A previous study was conducted to compare side effects of intravenous ketofol on children, and patients received titrated injection of a solution containing combination of one part of Ketamine and two parts of Propofol (1:2) or one part of Ketamine and three parts of Propofol (1:3). Lower dose of Ketamine in these combinations has lower psycho mimetic side effects, and shorter recovery time. Both groups preserved hemodynamic stability and there was no respiratory depression [Citation25].
Before starting this research work, the authors performed a pilot study for determination of the optimal proportion and infusion rate of the propofol–ketamine mixture in children undergoing cardiac catheterization. A mixture proportion of 5 mg/mL and 2.5 mg/mL and initial infusion rate of 25–50 mic/kg/min and 12.5–25 mic/kg/min of propofol and ketamine, respectively, were found to provide safe and consistent sedation in this population.
In this study regardless of the significant difference between the study groups in diastolic blood pressure, the change of more than 20% in MAP showed no significant difference between the study groups. The hemodynamic effects of propofol and ketamine are opposed to each other, allowing the use of lower doses of each agent, reducing their hemodynamic effects. A previous study conducted by El Din et al. comparing the combination of ketamine–propofol versus ketamine fentanyl for anesthesia in children undergoing cardiac catheterization showed statistical significant decreases in mean arterial blood pressure (MAP) and systemic vascular resistance (SVR) in KP group [Citation26]. In agreement with our findings a previous study conducted by Kogan et al. on forty-five children aged 6 months to 16 years undergoing cardiac catheterization showed that continuous intravenous infusion of a mixture of propofol and ketamine with spontaneous ventilation provided hemodynamic stability [Citation1].
Akin et al. investigated the effects of propofol and propofol–ketamine on hemodynamics, sedation level, and recovery period in pediatric patients undergoing cardiac catheterization. Propofol combined with low-dose ketamine preserves mean arterial pressure better without affecting the recovery and thus is a good option in pediatric patients undergoing cardiac catheterization [Citation7]. A previous study conducted by Russell et al. on 182 pediatric patients for elective correction or palliation of congenital heart disease, compares sevoflurane and halothane maintenance. Patients receiving halothane experienced twice as many episodes of severe hypotension as those who received sevoflurane (p = 0.03). Sevoflurane produces fewer dysrhythmias than halothane [Citation27,Citation28].
The drawback of our study is that we did not correlate the incidence of emergence agitation with pain using a validated pain score.
Conclusions
Both propofol–ketamine and sevoflurane provided effective sedation and analgesia during pediatric cardiac catheterization. But propofol–ketamine combination was superior to sevoflurane because the incidence of agitation, nausea and vomiting in patients given sevoflurane was significantly higher than in ketofol group.
Conflicts of interest
None.
Contribution
Shahira EL Metainy participated in study design, conducted the study, collected the data, analyzed the data, and prepared the manuscript.
Rabab Saber participated in study design, conducted the study, collected the data, analyzed the data, and prepared the manuscript.
Attestation
Shahira El Metainy approved the final manuscript and attests to the integrity of the original data and the analysis reported in this manuscript.
Rabab Saber approved the final manuscript and attests to the integrity of the original data and the analysis reported in this manuscript.
IRB: ethics committee faculty of medicine alexandria university, IRBno; 00007555-FWA no;00015712, Website http://ohrp.cat.nih.gov/search/search. Email: http://mailto:[email protected].
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- A.KoganR.EfratJ.KatzPropofol–ketamine mixture for anesthesia in pediatric patients undergoing cardiac catheterizationJ Cardiothor Vasc Anesth1762003691693
- A.DönmezA.KizilkanH.BerksunOne center’s experience with Remifentanil Infusions for pediatric cardiac catheterizationJ Cardiothorac Vasc Anesth1562001736739
- L.A.TrisselD.L.GilbertJ.F.MartinezCompatibility of propofol injectable emulsion with selected drugs during simulated Y-site administrationAm J Health Syst Pharm54199712871292
- R.F.DonnellyG.AndolfattoStability of ketamine–propofol mixtures for procedural sedation and analgesia in the emergency departmentCan J Hosp Pharm612008426430
- Z.TosunA.AkinG.GulerDexmedetomidine–ketamine and propofol–ketamine combinations for anesthesia in spontaneously breathing pediatric patients undergoing cardiac catheterizationJ Cardiothorac Vasc Anesth202006515519
- Z.TosunR.AksuG.GulerPropofolketamine vs propofol–fentanyl for sedation during pediatric upper gastrointestinal endoscopyPediatr Anesth172007983988
- A.AkinA.EsmaogluG.GulerPropofol and propofol–ketamine in pediatric patients undergoing cardiac catheterizationPediatr Cardiol262005553557
- A.AkinA.EsmaogluZ.TosunComparison of propofol with propofol–ketamine combination in pediatric patients undergoing auditory brainstem response testingInt J Pediatr Otorhinolaryngol69200515411545
- A.KoganR.EfratJ.KatzPropofol–ketamine mixture for anesthesia in pediatric patients undergoing cardiac catheterizationJ Cardiothorac Vasc Anesth172003691693
- J.WuDeep sedation with intravenous infusion of combined propofol and ketamine during dressing changes and whirlpool bath in patients with severe epidermolysis bullosaPediatr Anesth172007592596
- J.B.GuitH.M.KoningM.L.CosterKetamine as analgesic for total intravenous anaesthesia with propofolAnaesthesia4619912427
- S.BadrinathM.N.AvramovM.ShadrickThe use of a ketamine–propofol combination during monitored anesthesia careAnesth Analg902000858862
- J.EscarmentE.CantaisP.Le DantecPropofol and ketamine for dressing in burnt patientsCah Anesthesiol4319953134
- S.GottschlingS.MeyerT.KrennPropofol versus midazolam/ketamine for procedural sedation in pediatric oncologyJ Pediatr Hematol Oncol2792005471476
- R.A.HasanJ.R.ShayevitzV.PatelDeep sedation with propofol for children undergoing ambulatory magnetic resonance imaging of the brain: experience from a pediatric intensive care unitPediatr Crit Care Med442003454458
- L.SymingtonS.ThakoreA review of the use of propofol for procedural sedation in the emergency departmentEmerg Med J23220068993
- S.UezonoT.GotoK.TeruiEmergence agitation after sevoflurane versus propofol in pediatric patientsAnesth Analg9132000563566
- I.T.CohenJ.C.FinkelR.S.HannallahK.A.HummerK.M.PatelRapid emergence does not explain agitation following sevoflurane anaesthesia in infants and children: a comparison with propofolPaediatr Anaesth13120036367
- D.J.StewardA simplified scoring system for the post-operative recovery roomCan Anaesth Soc J221975111113
- M.F.WatchaM.Ramirez-RuizP.F.WhiteM.B.JonesR.G.LagueruelaR.P.TerkondaPerioperative effects of oral ketorolac and acetaminophen in children undergoing bilateral myringotomyCan J Anaesth391992649654
- J.R.ChandlerD.MyersD.MehtaE.WhyteM.K.GrobermanC.J.MontgomeryJ.M.AnserminoEmergence delirium in children: a randomized trial to compare total intravenous anesthesia with propofol and remifentanil to inhalational sevoflurane anesthesiaPaediatr Anaesth2342013309315
- H.S.JooW.J.PerksSevoflurane versus propofol for anesthetic induction: a meta-analysisAnesth Analg9112000213219
- A.J.DavidsonN.S.MortonS.J.ArnupApnea after awake regional and general anesthesia in infants: the general anesthesia compared to spinal anesthesia study-comparing apnea and neurodevelopmental outcomes, a randomized controlled trialAnesthesiology12312015 Jul3854
- G.T.YousefK.M.ElsayedA clinical comparison of ketofol (ketamine and propofol admixture) versus propofol as an induction agent on quality of laryngeal mask airway insertion and hemodynamic stability in childrenAnesth Essays Res722013194199
- A.Ghadami YazdiV.AyatollahiA.HashemiSh.BehdadYazdi.E.GhadamiEffect of two different concentrations of propofol and ketamine combinations (ketofol) in pediatric patients under lumbar puncture or bone marrow aspirationIran J Ped Hematol Oncol312013187192
- H.El DinA.EldeebKetamine–propofol versus ketamine fentanyl for anesthesia in pediatric patients undergoing cardiac catheterization: a prospective randomized studyEgypt J Anaesth2812012 Jan4953
- I.A.RussellW.C.Miller HanceG.GregoryM.C.BaleaL.CassorlaA.DeSilvaR.F.HickeyL.M.ReynoldsK.Rouine-RappF.L.HanleyV.M.ReddyM.K.CahalanThe safety and efficacy of sevoflurane anesthesia in infants and children with congenital heart diseaseAnesth Analg925200111521158
- R.S.HolzmanM.E.van der VeldeS.J.KausS.C.BodyS.D.ColanL.J.SullivanS.G.SorianoSevoflurane depresses myocardial contractility less than halothane during induction of anesthesia in childrenAnesthesiology85199612601267