Abstract
Background
Anesthetic management, of patients with cardiomyopathy with reduced systolic function, is challenging and may be associated with high mortality. Continuous epidural anesthesia (CEA) is generally accepted as the routine method of regional anesthesia for vascular surgery of the lower limb.
Continuous spinal anesthesia (CSA) has been reported to be more rapid in action, with good sensory and motor block, fewer hemodynamic disturbance and side effects when compared to continuous epidural anesthesia (CEA), and single dose spinal anesthesia (SDSA).
Patients and methods
Forty adult patients with depressed systolic function (EF 45% or less) scheduled for lower abdominal surgeries were subjected to our study. Under full aseptic precautions subarachnoid space was accessed in the setting position by an epidural needle at L3–4 and 2 ml of hyperbaric bupivacaine (10 mg) was injected into subarachnoid space, then an epidural catheter was inserted in the subarachnoid space for 3 cm. Anesthesia was maintained by Top up doses of plain bupivacaine 0.5% 1.2 ml.
Result
There were no differences in demographic characteristics of patients, procedure’s duration, and ASA physical status classification. There were no significant changes in hemodynamics throughout the procedure. Hypotension occurred in 5% of patients, bradycardia occurred in 10% of patients and arrhythmia occurred in 2.5% of patients. There were no postoperative ECG changes and postoperative Troponin was negative. There was no postoperative Neurological deficit or Post dural puncture headache.
Conclusion
We can conclude that, CSA was effective and safe technique for patients with cardiomyopathy undergoing lower abdominal surgeries.
1 Introduction
Patients with cardiomyopathy are increasing nowadays as a result of advance in the facility of diagnosis and increase in the numbers of aging people. This type of patients may present for anesthesia and surgery so the anesthesiologist must understand the pathophysiology of this type of disease for better management and better patients outcome.
Dilated cardiomyopathy (DCM) is defined by the presence of (a) fractional myocardial shortening <25% and/or ejection fraction <45% and (b) left ventricular end diastolic diameter >117% excluding any known cause of myocardial disease. LV ejection fraction of ⩽35% is considered to be an optimal predictor of postoperative cardiac events [Citation1,Citation2].
Anesthetic management of patients with severe cardiomyopathies is associated with a high morbidity and mortality [Citation3] and therefore requires careful planning, preparation and monitoring [Citation4]. The preoperative preparation of these patients must be meticulous as they have minimal or no cardiac reserve. Any decrease in myocardial contractility, heart rate, or vasodilatation can cause profound hypotension. Preoperatively, patients tend to be dehydrated, as most of patients on diuretic therapy, a further cause for hypotension during anesthetic care. Preoperative hydration may not be desirable as it may lead to congestive heart failure. Fluid management is critical, and also the hypovolemic state is prudent. Therefore a vasopressor was used to overcome the vasodilating effect of the anesthesia [Citation1].
Arrhythmias occur when potassium or magnesium levels are decreased. These electrolytes should be measured preoperatively and corrected as necessary [Citation5].
Continuous epidural anesthesia (CEA) is generally accepted as the routine method of regional anesthesia for vascular surgery of the lower limb. However continuous spinal anesthesia (CSA) has been reported to be more rapid in action, good sensory and motor block, with fewer hemodynamic disturbance and side effects, when compared to Continuous epidural anesthesia (CEA), and single dose spinal anesthesia (SDSA) [Citation6,Citation7].
1.1 Aim of the study
The aim of the present study was to evaluate the safety of continuous spinal anesthesia (CSA) in patients with cardiomyopathy underwent lower abdominal surgeries as regard to changes in hemodynamic, the vasopressor use, surgeon and patients satisfaction.
The primary outcome is the hemodynamic changes while surgeon’s and patient’s satisfaction was the secondary outcome.
2 Patients and methods
This study was carried out on Forty adult patients with depressed systolic function (EF 45% or less) scheduled for lower abdominal surgeries in Tanta University Hospitals for 9 months after approval from the medical ethical committee (approval code: 30124/03/31) and written informed consent from the patients.
All patients’ data were confidential with secret codes and were used for the current study only.
Any unexpected risk appears during the course of the study was cleared to the patients and the ethical committee on time and the proper measures were taken to minimize or overcome these risks.
2.1 Exclusion criteria
Patients refusal, morbid obese, tight mitral or aortic stenosis, patients on anticoagulant therapy, coagulopathy, history of allergy to drugs used, local infection in the puncture area, and severe deformity of the spinal column.
2.2 Preoperative preparation
All patients underwent preoperative assessment by history taking, physical examination and laboratory investigations which include complete blood count, liver function, renal function, random blood sugar, prothrombin time, INR, ECG, blood group, chest X-ray echocardiography, and serum electrolyte.
2.3 Premedication
All patients received 150 mg ranitidine and 10 mg of metoclopramide one hour before anesthesia. All cardiac medications were continued till time of surgery.
2.4 Intraoperative management
The procedure was explained to the patients during the preoperative visit. Patients were fasted for 8 h before the time of operation. On arrival to operating room an intravenous line was inserted and the patients were attached to monitor displaying the following: ECG, invasive blood pressure, noninvasive blood pressure, pulse oximetry, heart rate, O2 saturation and urinary catheter for urine output monitoring.
Central venous catheter was inserted through right internal jugular vein for fluid and drugs infusion and to measure the CVP. Arterial line was inserted for invasive blood pressure monitoring.
2.5 Anesthetic management
Under full aseptic precautions the skin was cleaned with an antiseptic solution, and the subcutaneous tissues and muscles are infiltrated with 3 ml of lidocaine 2%. Subarachnoid space was accessed in the setting position by an epidural needle at L3–L4 and 2 ml of hyperbaric bupivacaine (10 mg) was injected into subarachnoid space, then a epidural catheter was inserted in the subarachnoid space for 3 cm. After confirming a correct position of the catheter by seeing CSF leak, the catheter was connected to adopter and bacterial filter and was secured in position making sure that it is not kinked. Anesthesia was maintained by Top up doses of plain bupivacaine 0.5% 1.2 ml (as 0.2 ml would be retained in the catheter), given every hour to maintain the sensory at T10.
The level of the sensory blockade was tested using pinprick tests. If analgesia at level T12 was not achieved within 20 min, additional bupivacaine 1.2 ml was administered through the catheter.
Motor block was assessed with modified Bromage scale (0 = no block, 1 = inability to raise the extended leg, 2 = inability to flex the knee and 3 = inability to flex the knee and foot) and surgery was began when the modified Bromage score was 2 or 3.
2.6 Fluid therapy
All patients received a lactated ringer solution 5 ml/kg/h and blood loss was replaced by blood. The patients were given oxygen at the rate of two liters/minute through a nasal catheter.
Hypotension was defined as a decrease in mean arterial blood pressure by 20% or more from baseline or systolic blood pressure less than 90 mmHg after spinal block and was managed by 6 mg of ephedrine repeated twice if no response of noradrenaline was given in a dose 4–8 μg/min and the dose was adjusted to maintain the systolic blood pressure above 100 mmHg.
Bradycardia was defined as decrease in heart rate less than 60 beat/min and was managed by 0.5 mg of atropine. If Arrhythmias occurred it was treated by amiodarone infusion.
After completion of surgery we injected 1.2 ml of bupivacaine and 25 μg of fentanyl for postoperative analgesia, the catheter was removed and the patients were transferred to ICU.
2.7 Measurements
| – | HR. | ||||
| – | MABP. | ||||
| – | Total dose of bupivacaine. | ||||
| – | Duration of surgery. | ||||
| – | Surgeon’s satisfaction criteria which include, the surgical field bleeding, immobility of the patient, and degree of muscle relaxation. | ||||
| – | Patient’s satisfaction criteria included any pain or discomfort during surgery and in the post-operative period. | ||||
| – | Postoperative ECG every 12 h. | ||||
| – | Postoperative Troponin daily for 3 days. | ||||
2.8 Complication
Hypotension – Arrhythmia – Bradycardia – Nausea and vomiting – Neurological deficit – Post dural puncture headache.
2.9 Statistical analysis
The sample size required for the study was determined based on the primary outcome measure. A power analysis suggested that a sample size of 36 patients should be adequate to detect a 20% reduction in blood pressure and heart rate with a power of 0.8 (alpha = 0.05). However, to avoid potential errors, 40 patients were included in the study.
The statistical analysis was done using SPSS Version 20 for Macintosh.
Comparison of demographic data, and time of surgery were done by Student’s t-test. Two way analysis of variance for repeated measurements was used for heart rate and blood pressure comparison. Values are reported as mean ± SD. P values <0.05 were considered significant.
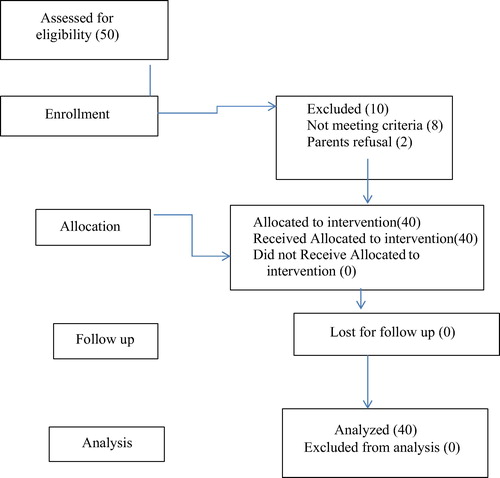
The process of inclusion in the study went on until the required number of patients was reached (see ).
3 Result
Our study was carried out on forty adult patients with cardiomyopathy EF 45% or less. There were no differences in the baseline characteristics of patients including age, body weight, procedure’s duration, and ASA physical status classification ().
Table 1 Demographic data, duration of surgery, duration of performance block and type of surgeries.
showed the level of sensory block, motor block and total dose of bupivacaine dose. 38 patients showed sensory block at T0 while 37 patients showed bromage scale 3. The total dose of bupivacaine was 15.6 ± 0.7 mg.
Table 2 Level of sensory, motor block and bupivacaine dose.
There were no statistical significant changes in heart rate and MABP throughout the procedure ().
Table 3 Hemodynamic changes and vasopressor dose.
Hypotension occurred in 5% of patients, bradycardia occurred in 10% of patients and arrhythmia occurred in 2.5% of patients. There were no postoperative ECG changes and postoperative Troponin was negative ().
Table 4 Incidence of side effects.
There was no Neurological deficit, Post dural puncture headache or postoperative Nausea and vomiting ().
Patients and surgeon satisfaction was excellent ( and ).
Table 5 Surgeon’s satisfaction.
Table 6 Patient’s satisfaction.
4 Discussion
The results of the present study indicate that CSA was effective and safe technique for patients with cardiomyopathy undergoing lower abdominal surgeries, it provided better cardiovascular stability, and it was easier to perform with better patients and surgeon satisfaction. The technique allows titration of the local anesthetic dose which allows controlling the level of the sensory and motor blockade according to surgical needs and provides safe anesthesia, especially for high-risk patients with reduced cardiac function.
The result of the present study could be explained by improvement in cardiac output as a result of decrease in systemic vascular resistance and reduction of after load due to sympathetic blockade produced by low dose of spinal anesthesia [Citation8].
The anesthetic goals for patients with cardiomyopathy are as follows: maintenance of myocardial contractility, drugs induced myocardial depression that should be avoided, prevention of increase in afterload, maintenance of hemodynamic stability, avoidance of arrhythmias, electrolyte imbalance and avoidance of volume overload [Citation1].
The cardiac output depends on two factors, the heart rate and ejection fraction which are controlled by end diastolic volume and myocardial contractility. Patients with cardiomyopathy and reduced contractility, and the cardiac output depend on the left ventricular end diastolic volume and do not depend on increase in heart rate [Citation9,Citation10].
Spinal anesthesia induces sympathetic block and vasodilation causes pooling of the blood in the peripheral circulation leading to decrease in end diastolic volume which reduces cardiac output. Patients with reduced cardiac reserve are preload dependent and were expected to more decrease in cardiac output and major hemodynamic disturbance when spinal anesthesia was given as single shot with large dose of local anesthetic as result of sympathetic block and decrease in stoke volume [Citation8].
Continuous spinal anesthesia (CSA) was expected to produce less decrease in cardiac output and mean arterial blood pressure than single shot spinal anesthesia as, sympathetic blockade was less because small dose of local anesthetic was injected with CSA [Citation11].
Sanatkar et al. [Citation8] found that, the decrease in mean arterial blood pressure was less in patients with low ejection fraction who received low dose spinal block with bupivacaine and concluded that Spinal block with low dose local anesthetic was a safe and effective method for lower limb surgery in patients with low ejection fraction which supports our results.
Advantages of regional anesthesia over general anesthesia include the following: It allows patient communication of subjective feelings of distress, the hemodynamic changes of laryngoscopy and intubation are avoided, it attenuates stress response to surgery, produces vasodilatation thereby decreasing afterload, decreases incidence of DVT, and decreases incidence of pulmonary embolism, postoperative analgesia can be given via catheter, opioid use was minimized, less postoperative nausea and vomiting, and better patients and surgeon satisfaction, associated with early recovery [Citation12].
Continuous spinal anesthesia offers many of the advantages over epidural anesthesia, and the onset of peripheral sympathetic block develops in a gradual and controlled fashion because very small dose of local anesthetic was used in continuous spinal anesthesia compared to epidural anesthesia. Also catheter placement is technically easier and aspiration of CSF provides confirmation of correct catheter placement, and also the catheter can be left in place for postoperative pain management, minimizing the need for systemic opiates and their risks [Citation13].
Advantages of CSA over single shot spinal anesthesia: with the continuous spinal anesthesia (CSA) technique, local anesthetic dose can be repeated, thus making it possible to use this spinal anesthesia method in operations with long duration [Citation14]. CSA enables to titrate the dose of local anesthetic thus allowing better control of sensory and motor block level, no risk of local anesthetic toxicity and providing shorter recovery periods, and it provides better hemodynamic stability. Furthermore, spinal catheter may be inserted in regional anesthesia preparation room before the operation, thus preventing loss of time between operations [Citation15–Citation17].
However, continuous spinal anesthesia has potential complications: worsening hypotension in situation of major blood loss, myocardial ischemia, postdural puncture headache, persistent paresthesia, low back pain, and risk of infection.
Our result is in agreement with Lux et al., and they concluded that continuous spinal anesthesia appears to be a safe and appropriate anesthetic technique in lower leg surgery for aged patients [Citation18].
Additionally, Denny et al. concluded that, continuous spinal anesthesia has clear advantages over epidural and single shot spinal anesthesia, especially in elderly or high-risk patients. CSA offers possibilities of reduced interference with the cardiovascular and respiratory systems and the duration can be extended to match the needs of prolonged surgery [Citation19].
Imbelloni et al. found that, CSA provided good surgical conditions with low incidence of complications. The hemodynamic changes were lower with CSA [Citation20].
Moreover, Baydilek et al. concluded that, continuous spinal anesthesia can be used safely in older patients for transurethral prostate resection operations [Citation21].
Also, Jaitly et al. suggests that, CSA can be used as a sole anesthetic technique for laparotomy especially in patients with severe cardio-respiratory disease who would otherwise be considered unlikely to tolerate general anesthesia or where general anesthesia could result in a prolonged stay in the intensive care unit [Citation22].
Fyneface-Ogan and Ojule reported a successful anesthetic management of parturient with peripartum cardiomyopathy with continuous spinal anesthesia without any adverse events to mother or baby and CSA was associated with more stable hemodynamic changes [Citation23].
5 Conclusion
We can conclude that, CSA was effective and safe technique and can be used as an alternative to single shot spinal anesthesia, epidural anesthesia and general anesthesia for patients with cardiomyopathy undergoing lower abdominal surgeries. CSA provided better cardiovascular stability with low dose of local anesthetic. Proper training is vital for the optimal use of CSA.
Conflict of interest disclosure
No conflict and no fund.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- P.H.L.ThiagarajahS.ThiagarajahE.A.FrostAnesthetic considerations in patients with cardiomyopathies – a reviewMiddle East J Anesthesiol2032009347354
- B.S.MartinezI.GasanovaA.O.AdesanyaAnesthesia for kidney transplantation – a reviewJ Anesth Clin Res41201316
- W.KlimschaC.WeinstablW.IliasN.MayerA.KashanipourB.SchneiderContinuous spinal anesthesia with a micro-catheter and low-dose bupivacaine decreases the hemodynamic effects of centroneuraxis blocks in elderly patientsAnesth Analg771993275280
- A.L.TabibL.ChalabreysseC.BarelC.DuracherR.LoireD.MalicierSudden death during anesthesia: human error drug, related or cardiac deathTherapie5662001735738
- L.CeremuzyńskiJ.GebalskaR.WolkE.MakowskaHypomagnesemia in heart failure with ventricular arrhythmias. Beneficial effects of magnesium supplementationJ Intern Med247120007886
- A.KashanipourK.StrasserW.KlimschaR.TaslimiA.AloyContinuous spinal anesthesia versus continuous epidural anesthesia in surgery of the lower extremities. A prospective randomized studyReg Anaesth1419918387
- W.KlimschaC.WeinstablW.IliasN.MayerA.KashanipourContinuous spinal anesthesia with a microcatheter and low-dose bupivacaine decreases the hemodynamic effects of centroneuraxis blocks in elderly patientsAnesth Analg771993275278
- M.SanatkarM.SadeghiN.EsmaeiliH.SadrossadatM.ShoroughiThe hemodynamic effects of spinal block with low dose of bupivacaine and sufentanil in patients with low myocardial ejection fractionActa Med Iran5172013438443
- G.FanelliB.BorghiA.CasatiL.BertiniM.MontebugnoliG.TorriUnilateral bupivacaine spinal anaesthesia for outpatient knee arthroscopyCan J Anesth4782000746751
- L.ElzingaM.MarcusD.PeekP.BorgJ.JansenJ.KosterD.EnkHemodynamic stability ensured by a low dose, low volume, unilateral hypobaric spinal block: modification of a techniqueActa Anaesthesiol Belg6042009217220
- S.SeldaK.AydinG.DiscigilHypotension induced by lateral decubitus or supine spinal anesthesia in elderly with low ejection fraction undergoing hip surgeryJ Clin Monit Comput2122007103107
- C.DeshpandeS.FernandesG.DhakneDialated cardiomyopathy and end stage renal disease with renal osteodystrophy for bilateral transcervical fracture femur fixationInt J Anesthesiol20200913
- T.R.LubenowA.D.IvankovichR.J.McCarthyManagement of acute postoperative painP.G.BarashB.F.CullenR.K.StoeltingClinical anesthesia2nd ed.1992JB LippincottPhiladelphia
- B.K.BevacquaContinuous spinal anaesthesia: what’s new and what’s notBest Pract Res Clin Anaesthesiol172003393406
- A.SellK.T.OlkkolaJ.JalonenR.AantaaMinimum effective local anaesthetic dose of isobaric levobupivacaine and ropivacaine administered via a spinal catheter for hip replacement surgeryBr J Anaesth942005239242
- J.F.Favarel-GarriguesF.SztarkM.E.PetitjeanM.ThicoïpeP.LassiéHemodynamic effects of spinal anesthesia in the elderly: single dose versus titration through a catheterAnesth Analg8221996312316
- D.MichaloudisA.PetrouP.BakosContinuous spinal anaesthesia/analgesia for the perioperative management of high-risk patientsEur J Anaesthesiol1742000239247
- E.A.LuxContinuous spinal anesthesia for lower limb surgery: a retrospective analysis of 1212 casesLocal Reg Anesth520126367
- N.M.DennyD.E.SelanderContinuous spinal anesthesiaBr J Anaesth8141998590597
- L.E.l.ImbelloniM.A.GouveiaJ.A.CordeiroContinuous spinal anesthesia versus combined spinal epidural block for major orthopedic surgery: prospective randomized studySao Paulo Med J12712009711
- Y.BaydilekB.S.YurtluV.HanciH.AyoğluR.D.OkyayThe comparison of levobupivacaine in continuous or single dose spinal anesthesia for transurethral resection of prostate surgeryBraz J Anesthesiol64220148997
- V.K.JaitlyC.M.KumarContinuous spinal anaesthesia for laparotomyCurr Anaesth Crit Care20096064
- S.Fyneface-OganJ.D.OjuleContinuous spinal anaesthesia for caesarean section in a parturient with peripartum cardiomyopathyNiger J Med2322014178182