Abstract
Lung bulla occupying more than 30% of hemithorax is described as giant bulla which is now treated surgically with positive outcomes. During intraoperative period, these patients are vulnerable to hyperinflation, hypoxia and hypercarbia due to significantly increased dead space and reduced functional alveoli, gas exchange and oxygen reserve. Real hazard is rupture of bulla, which can lead to life threatening tension pneumothorax if it occurs before lung isolation. Hence, a technique of induction wherein spontaneous breathing is maintained is thought to be ideal.
Here we present a patient with giant lung bulla in left lower lobe with severely reduced pulmonary reserves and significant air-trapping posted for VAT assisted bullectomy. Anaesthesia challenges including pathological changes, its effects during induction of anaesthesia, and issues related to placement of double lumen tube in a spontaneously breathing patient are discussed with possible advantages of dexmedetomidine in this special group of patients.
1 Introduction
Anaesthesia management of patients with giant pulmonary bulla is a challenge owing to effects of smoking, chronic obstructive pulmonary disease (COPD), and impaired gas exchange with extremely poor respiratory reserve. The severity of these problems directly depends on size, number and extent of the emphysematous bullae.
2 Case history
A 65 years hypertensive male patient case of COPD with multiple bilateral emphysematous bullae was scheduled for thoracoscopic left lung bullectomy. He was a chronic smoker since 38 years, and discontinued since 2 years. On examination, pulse rate was 82/min, BP 106/70 mmHg, respiratory rate 16–18/min. On auscultation air entry was decreased in left infra-mammary region and was absent in left infrascapular region of the lung.
Investigations revealed haemoglobin of 14.5 gm/dl, rest within normal limits. Echocardiography was suggestive of moderate Pulmonary Hypertension (57 mmHg). HRCT Thorax revealed panlobular emphysema in both lungs (A) with a giant bulla (17 cm × 9.5 cm × 9.4 cm) in left lower lobe (B). Preoperative arterial blood gas analysis is shown in .
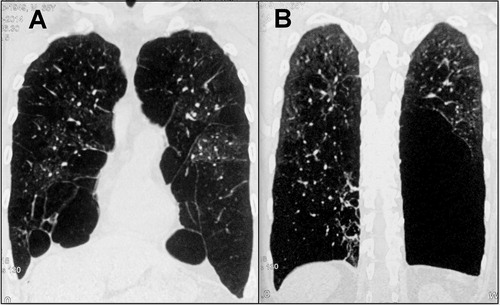
Table 1 Preoperative arterial blood gas analysis.
The pulmonary function tests () revealed severe decrease in FVC, FEV1 and FEV1/FVC (46.9%, 23.3% and 49.7% predicted respectively). Bronchodilator therapy exhibited no improvement. Total lung capacity was significantly decreased (57.46% pred) and residual volume was disproportionately high (134.9%) suggestive of air trapping.
Table 2 Pulmonary function TEST.
Preoperatively, his regular bronchodilator nebulisations with salbutamol and budesonide were continued and incentive spirometry and steam inhalation started. The patient was kept fasting for 8 h prior to surgery.
Inside operating room, Standardised monitors including pulse oximeter, electrocardiogram and noninvasive blood pressure were applied and oxygen supplementation at 2 L/min was started. Left radial artery and right internal jugular vein were cannulated. Xylocaine viscous 10% gargles given and glycopyrrolate 0.2 mg injected intravenously. With the patient in 20 degree head up position, dexmedetomidine intravenous infusion was started in a loading dose of 1 μg/kg over 10 min followed by maintenance at 1 μg/kg/h, while continuing oxygen supplementation (6 l/min) with mask. Five minutes after completion of loading dose, patient was in a state of sedation with Ramsay sedation score 4, breathing comfortably without any signs of respiratory depression or airway obstruction. Laryngoscopy was attempted with No. 4 McIntosh blade while patient breathing spontaneously. Vocal cords were visualised and sprayed with 1 ml 2% xylocaine and 5 ml 2% xylocaine instilled into trachea, and oxygen supplementation continued for 3 more minutes. Under direct laryngoscopic vision, 39 Fr left sided double lumen tube (DLT) (Bronchocath®) was introduced transtracheal during inspiration and intubation was accomplished. Tracheal and bronchial cuffs were inflated, and lung isolation was achieved and confirmed. Patient continued to breathe spontaneously throughout this process without any evidence of coughing, straining, and unanticipated movements.
Anaesthesia was then induced intravenously with Fentanyl 2 mcg/kg, Propofol and Atracurium intravenously. Anaesthesia was maintained with sevoflurane (MAC 0.7-1.0) in oxygen – air mixture (50:50) (FiO2 60%) and Atracurium boluses. Volume control ventilation initiated with tidal volume of 8 ml/kg, I:E ratio 1:3, with a respiratory rate targeting peak airway pressure less than 25 cm H2O and ETCO2 35–40 mmHg. At the beginning of Thoracoscopy, one lung ventilation (OLV) was commenced and tidal volume readjusted to 4 ml/kg, I:E ratio 1:3, FiO2 75% and RR adjusted to maintain ETCO2 between 35 and 40 mmHg and peak airway pressure < 25 cm H2O. Dexmedetomidine infusion was stopped at the beginning of skin closure. Neuromuscular blockade reversed with neostigmine 2.5 mg and glycopyrrolate 0.4 mg intravenously. Patient was extubated after an arterial blood gas analysis (pH 7.26, pCO2 54 mmHg, PO2 301 mmHg, HCO3 24 mmol/l).
3 Discussion
Abnormal increase in the size of airspaces distal to terminal bronchiole is termed as emphysema. An air space more than 1 cm diameter in lung is described as lung bulla [Citation1]. When the lung bulla occupies more than 30% of hemithorax, it is termed as giant bulla [Citation2]. It is most commonly related to COPD [Citation1], though it can be idiopathic or secondary to infection.
Bullae increases dead space and consequently decreases gas exchange and oxygen reserve. Bilateral/multiple/larger bullae are more hazardous, as the number of functional alveoli is significantly reduced and gas exchange is severely compromised [Citation1]. It makes these patients vulnerable for hyperinflation, hypoxia and hypercarbia in perioperative period. During induction of anaesthesia, there is a higher possibility of rupture of the bullae leading to tension pneumothorax either spontaneously or secondary to positive pressure ventilation. Use of positive pressure ventilation may be elective or may be secondary to apnoea/airway collapse due to use of sedatives, induction agents and/or muscle relaxants. Thus use of muscle relaxants and respiratory depressants during induction of anaesthesia has been questioned. A technique of induction wherein spontaneous breathing is maintained is thought to be ideal and has been recommended [Citation3].
Our patient had severe COPD with bilateral pan-lobular bullae and severe reduction in respiratory reserve. As this patient was having giant pulmonary bulla, with massive air trapping and extremely low compliance, he was at risk of rupture of bullae and consequent fatal pneumothorax. Thus we had planned placement of DLT and isolation of lung while patient breathing spontaneously.
Thus, the agent used for cortical suppression during airway control and placement of DLT, should provide adequate sedation, analgesia and stress attenuation without causing respiratory depression, apneic spells and/or airway collapse, thus nullifying the need for positive pressure ventilation. Care should also be taken to attenuate airway reflexes during placement of bulkier and stiffer DLT, stimulation of which can cause (1) coughing, straining and struggling in non-paralysed patients and (2) haemodynamic hyper activity due to sympathoadrenal response.
Dexmedetomidine is a highly selective α-2 adrenergic agonist which is sedative, anxiolytic, and hypnotic agent [Citation4]. The most promising property of dexmedetomidine is that it does not predispose to respiratory depression and airway obstruction [Citation4,Citation5] and maintains PaCO2 levels close to that seen during normal sleep [Citation6]. Also, it provides hemodynamic and sympathoadrenal stability during procedure by reducing the circulating catecholamines [Citation7]. Dexmedetomidine also appears to have effect of reducing airway reflexes as it has been used to reduce coughing during extubation [Citation8].
In the present case, we used dexmedetomidine based anaesthesia technique for lung isolation and anaesthesia maintenance. We observed that patient tolerated the procedure of intubation with DLT well while maintaining spontaneous respiration and patency of airway. From commencement of laryngoscopy till achieving lung isolation, no difficulty in terms of coughing, straining, and unanticipated movements, difficulty in continuing laryngoscopy/visualisation of glottis, and difficulty in insertion or manipulation of DLT were encountered. No significant changes in haemodynamic parameters were observed during laryngoscopy.
Thus, intravenous dexmedetomidine with simple topicalization of airway appears to provide a substantial balance between optimum conditions for placement of double lumen tube and maintenance of adequate spontaneous ventilation and patency of airway. However further studies and experiences are required to verify the same.
Conflict of interest
None.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- S.Y.RuanC.T.HuangJ.Y.ChienNon-surgical management of giant lung bullae during mechanical ventilationRespir Care56201116141616
- J.A.GreenbergS.SinghalL.KaiserGiant bullous lung disease: evaluation, selection, techniques and outcomesChest Surg Clin N Am1342003631649 12/2003
- E.G.PavlinRespiratory diseasesJ.KatzJ.L.BenumofL.B.KadisAnesthesia and uncommon diseases3rd ed.1990W.B. SaundersPhiladelphia305332
- X.Y.HeJ.P.CaoQ.HeX.Y.ShiDexmedetomidine for the management of awake fibreoptic intubation (review)Cochrane Database Syst Rev12014CD009798 2014 Jan 19
- T.KunisawaS.HanadaS.TakahataAwake intubation under sedation infusion of dexmedetomidineJ Anesth242010789792
- T.J.EbertJ.E.HallJ.A.BarneyT.D.UhrichM.D.ColincoThe effects of increasing plasma concentrations of dexmedetomidine in humansAnesthesiology932000382394
- K.GuptaM.JainP.K.GuptaDexmedetomidine premedication for fiberoptic intubation in patients of temporomandibular joint ankylosis: a randomized clinical trialSJA632012219223
- G.GulerA.AkinZ.TosunSingle dose dexmedetomidine attenuates airway and circulatory reflexes during extubationActa Anaesthesiol Scand498200510881091
