Abstract
Sturge-Weber Syndrome (SWS) is a non-familial neurocutaneous disorder characterized by facial port wine stain and occipital leptoangiomatosis with resulting neurological abnormalities. Ocular involvement is seen in 25–30% cases. We report a case of 12 year old boy having port wine stain on his left side of face with poor left sided vision. Proper examination and anesthetic management of these patients are very important for an anticipated difficult intubation if angiomas involve the airway. Smooth induction and extubation are necessary to avoid increase in intraocular and intracranial pressure.
Keywords:
1 Introduction
SWS also known as Encephalotrigeminal angiomatosis are a group of disorders with involvement of leptomeninges, eyes and face. Port wine stains of face, seizures, mental retardation, glaucoma and ipsilateral meningeal vascular malformations are common.
Port wine stain (PWS) is usually seen in distribution of first branch of the trigeminal nerve. They are unilateral in most of the cases. They carry a psychological impact due to cosmetic deformity although they are not medically threatening.
Severe nature of seizure disorder contralateral to facial naevus and mental retardation are other classical findings of this syndrome. Seizures are initially of focal type which progress to frequent generalized seizure. There is greater chance of refractoriness, mental retardation and neurological involvement if seizures start before the age of two. Other neurological symptoms are hemiparesis, hemianopsia, stroke like episodes, headaches, developmental delay and learning disabilities.
Ocular features include glaucoma (30–71%) most commonly buphthalmos, choroidal hemangioma and strabismus [Citation4]. Ocular features appeared to bear some relationship to the cutaneous manifestations but there is no correlation between the presence and severity of seizure disorder with cutaneous manifestation.
Skull X-ray shows intracranial calcification having a characteristic pattern of a parallel serpentine configuration known as the “tram sign” or the “railroad sign” [Citation3]. They may be used to confirm the clinical picture. Cortical calcifications are usually unilateral, present in occipital or occipito-parietal lobes and may also be found in frontal lobe.
2 Case report
A 12-year-old boy was admitted in the plastic surgery department of our institute for cosmetic correction of a capillary haemangioma on left side of his face (). It was present since birth, was painless and was increasing in size. He also had poor vision in the left eye (4/6). Parents gave a history of slow learning, communication difficulty and recurrent episodes of generalized tonic clonic seizures since last 5 years which last for 4–5 min. Last episode of seizure was reported 6 months back but patient was not on any anticonvulsant.
On general physical examination, PWS was present on left cheek and forehead in the distribution of trigeminal nerve. There was no sensory and motor involvement and gait was normal. On ophthalmic evaluation, pupil was regular round and reactive. There was congestion in left eye (4/6). During preoperative assessment mouth opening was adequate, Mallampati grade I, and no angiomas were found in the oral cavity but possibility of angiomas in the pharynx was considered and difficult airway cart was kept ready.
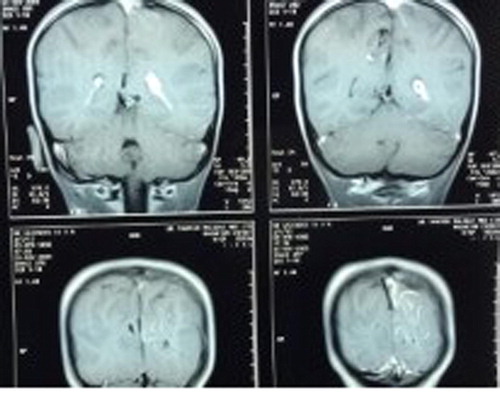
His blood investigations, urine examination, liver function test, Chest X-ray (PA view), and ECG were within normal limits. The clinical picture was confirmed by imaging study which showed calcified lesions in left frontal and occipital lobes ().
Patient was taken up for surgery, informed written consent was checked and routine monitors were attached. Patient was pre-oxygenated with 100% oxygen for 5 min and premedicated with intravenous midazolam 0.5 mg, ondensetrone 4 mg and fentanyl 30 μg. To attenuate the intubation response intravenous lidocaine 50 mg was given. Induction was done with thiopentone 200 mg, ventilation checked and vecuronium 2.5 mg given. Larynx was anaesthetized with lignocaine 4% spray. Gentle laryngoscopy performed and tracheal intubation was done with a well-lubricated endotracheal tube. Anesthesia was maintained with inhalational sevoflurane, oxygen and nitrous oxide. Intraoperative course was smooth and the patient was hemodynamically stable and was extubated after reversing the neuromuscular blockade with intravenous neostigmine and atropine 0.6 mg.
Patient was shifted to recovery room. For postoperative analgesia Intramuscular diclofenac 50 mg was used. Patient was discharged from the hospital after three days.
3 Discussion
SWS may be suspected when a facial nevus flammeus is found in a newborn in the area of distribution of trigeminal nerve (usually superior eyelid and supraorbital region). In our patient port wine stain was present on his face since birth. Laser treatment should be initiated for optimal results. Photocoagulation and de-bulking surgery can be done if there is hypertropic alteration. If left untreated they can become thick, darker, and even nodular. In SWS angiomas are frequently unilateral but may be bilateral. There may be anticipated difficult intubation if angiomas involve mucous membrane of nose, gingiva, palate, tongue, larynx and trachea [Citation1,Citation2,Citation5]. Intubation should be smooth and performed with soft, non-styletted, well-lubricated endotracheal tubes to avoid any bleeding from these angiomas. Careful tracheo-bronchial suction is also mandatory [Citation1,Citation2,Citation4,Citation5].
Leptomeningeal angiomas may cause hemiparesis, stroke like episodes, seizures, developmental delay, learning disabilities and mental retardation. In our patient seizures were well controlled. Factors precipitating seizures such as hypoxemia, hypoglycemia, hypotension, ischemia and hyperthermia should be avoided [Citation2,Citation4,Citation5]. Thiopentone that is a cerebroprotective barbiturate was used to induce this patient. Increase in intracranial pressure can result in intracranial hemorrhage from associated hemangiomatous lesions so drugs causing increase in intracranial (ICP) and intraocular pressure (IOP) should be avoided. Increase in ICP and IOP can be prevented by avoiding straining, bucking, obstructed airways and light plan of anesthesia during induction or emergence [Citation2,Citation4,Citation5]. Anticholinergics should be avoided in patients with narrow angle glaucoma [Citation4].
4 Conclusion
Patient with Sturge-Weber syndrome should be carefully evaluated. Better recognition and awareness of risk factors associated with specific diseases decrease the likelihood of complications. In the management of such cases a multidisciplinary approach (neurology, ophthalmology, anesthesiology) is indicated. Goal should be directed toward anticipated difficult intubation, maintenance of hemodynamic stability, smooth induction and extubation to avoid rise in intraocular and intracranial pressure.
Funding
This study was not funded by anybody.
Conflict of interest
No author has any conflict of interest to declare.
Ethical approval
This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the report.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- M.G.ButlerG.Hayes BlaineB.S.HayesM.M.HathawayM.L.BegleiterSpecific genetic diseases at risk for sedation/anesthesia complicationsAnesth Analg912000837855
- R.K.BatraV.GulayaR.MadanA.TrikhaAnesthesia and the Sturge Weber SyndromeCan J Anesth411994133136
- M.G.NormanW.C.SchoeneThe ultrastructure of Sturge-Weber disease Acta Neuropathol3731977199205
- M.GandhiH.IyerH.SehmbiK.DatirAnaesthetic management of a patient with Sturge-Weber syndrome undergoing oophorectomyIndian J Anaesth53120096467
- S.WongR.A.RahmanS.Y.ChooN.YahyaSturge-Weber-Syndrome with extreme ocular manifestation and rare association of upper airway angioma with anticipated difficult airwayMed J Malaysia6742012435437