Abstract
Paraganglioma is a rare neuroendocrine catecholamine producing tumour in childhood which arises outside the adrenal medulla. We present a 12 year old girl with giant paraganglioma with severe hypertension and end organ damage. Diagnosis was confirmed with 24 h urinary Vanillymandelic Acid (VMA) and CT scan. Preoperative blood pressure was controlled with intravenous nitroprusside, and oral prazosin, amlodepine, labetalol and metoprolol. General anaesthesia with epidural analgesia was given. Intra operative blood pressure rise was managed with infusion of nitriglycerine (NTG), esmolol, nitroprusside and propofol.
Keywords:
1 Introduction
Paragangliomas are tumours derived from specialized chemoreceptor tissue nest, thought to be of neural crest origin outside the adrenal medulla [Citation1]. They can arise in posterior mediastinum, retro-peritoneum in general, the base of skull, neck and vagal aortic bodies. It most commonly presents with paroxysmal spells of headache, sweating, palpitations and hypertension. Early diagnosis with aggressive peri operative management is required for reducing morbidity and mortality. Twenty-eight per cent of these tumours are bilateral, malignant and occur in children. In childhood, these tumours are more prevalent in boys than in girls, but trend reverses during adolescence with greater tendency for familial occurrence [Citation2–Citation4]. This case report describes peri-operative anaesthetic management in a child with giant paraganglioma which had encased the aortic adventitia, inferior venacava (IVC) and portal vessels.
2 Case history
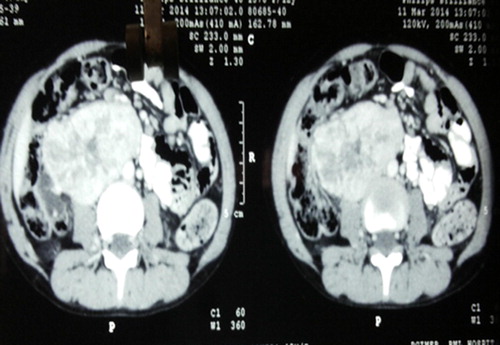
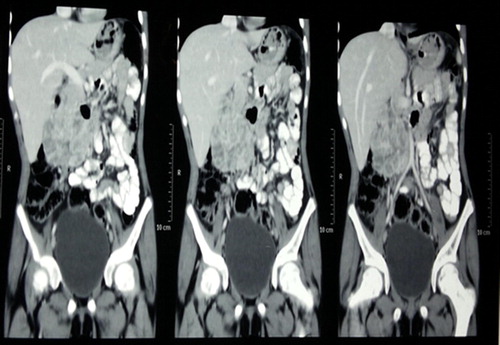
A 12 year old girl presented in hypertensive crisis with fronto-temporal headache for 1 month and blurring of vision and palpitation for 15 days. On examination, blood pressure (BP) was 196/160 mmHg. Cardiovascular examination revealed systolic murmur. Fundus examination showed hypertensive retinopathy with optic disk oedema in both eyes. A 10 × 8 cm smooth, fixed, hard retro-peritoneal lump was felt on abdominal palpation. Paraganglioma was confirmed on CECT abdomen which showed a heterogenous 10 × 8 × 5 cm mass in right para-aortic region encasing aorta (). Metaiodobenzylguanidine (MIBG) scan showed MIBG concentrating tumour. Gallium68 dotatate Positrion emission topogram (PET) scan showed a retro peritoneal mass extending from superior mesenteric artery (SMA) to L4/5 vertebrae level. The 24 h urinary analysis showed VMA to creatinine ratio of 71.33 mg/g creatinine [normal 1.5–5.1] and metanephrine 63.8 μg [25–31.2]. CT head did not reveal any metastasis. Thyroid function test and S. Calcium were found to be normal. Pre-operative stabilization was done with intravenous nitroprusside and furosemide and maintained on prazosin 5 mg tid, amlodepin 50 mg bid, labetolol 75 mg bid and metoprolol 5 mg bid. The child was taken up for excision of tumour with blood pressure of 140/90 mmHg and heart rate of 90/min. The medications were continued till the morning of surgery. As the paragalionoma was encasing the major vessels of abdominal cavity including aorta, IVC and portal vessels, a cardiopulmonary bypass machine was kept ready in case of any eventuality. In the operation room, intravenous line of 18 g was secured. Fentanyl 50 μg, midazolam 1 mg and hydrocortisone 50 mg were administered intra venously. All the standard monitors were attached. Left radial artery cannulation was done under local anaesthesia. After pre-oxygenation, anaesthesia was induced with propofol 2 mg/kg, fentanyl 2 μg/kg, vecuronium bromide 0.1 mg/kg, nitrous oxide:oxygen [60:40] and isoflurane 1%. Trachea was intubated with 6.5 mm cuffed endotracheal tube. Before intubation, vocal cords were sprayed with 10% lignocaine and intravenous Xylocard 30 mg was also given. Blood pressure rose to 180/110 mmHg after intubation which was controlled with bolus dose of propofol and isoflurane 2%. Internal juglar vein cannulation was performed with 5.5 Frg double lumen catheter. Epidural catheter 19G was inserted at L3−4 intervertebral space and 6 ml of 0.25% bupivacaine was administered in epidural space. Intraoperatively intermittent boluses of 3–4 ml of 0.25% bupivacaine was given hourly. Maintenance was done with 60% nitrous oxide in oxygen, isoflurane 1–2%, and intermittent vecuronium. Infusion of NTG 0.5 μg/kg/min and esmolol 50–100 μg/kg/min was started to control intra operative rise of BP and heart rate. Nitroprusside and propofol infusion was started during tumour manipulation. The BP did not rise beyond 190/110 mm HG, and heart rate went up to 110/min even during the tumour manipulation. But there was precipitous fall of BP to 80 mmHg after tumour resection; immediately, we discontinued infusions of esmolol, nitroglycerin, nitroprusside and propofol. To restore the blood pressure dopamine infusion was also started at 5 μg/kg/min and blood products, crystalloids and colloids were given. Arterial blood gas analysis showed a hematocrit of 25% and moderate acidosis. The blood loss was around 1.5 l. Fluid administered was 4 l of crystalloid, 1500 ml of blood and 2 units of fresh frozen plasma. Urine output was adequate. CVP was maintained at 7–8 cm of water and temperature was 35 °C. Tumour was shaved from inferior venacava, aorta and portal structures successfully (). BP was normalized before sending the patient to ICU for elective ventilation with dopamine infusion. At 6 month follow-up the child was normotensive, recurrence free and normal urinary VMA.
3 Discussion
Paragangliomas arise from neural crest and are usually syndromic [MEN II, Von-Hippel-Lindau, NF-1, etc.]. The well-known ‘10%’ rule does not apply to paediatric paragangliomas. In children, they are more likely to be extra-adrenal, malignant, recurrent syndromic and bilateral. Hypertension due to paraganglioma in children is more severe and refractory than in adults [Citation5]. Paraganglioma secretes mainly norepinephrine. It is seen more commonly in pre adolescent boys and teenage girls with male preponderance 2:1 [Citation2]. Manifestations are seen due to paroxysmal or sustained release of norepinephrine resulting in constriction of arteriolar and venous segment thereby decreasing the circulatory blood volume [Citation6]. The patients of paraganglioma generally present with headache, severe hypertension, palpitation and end organ failure. In our case, the child had developed features of end organ damage such as hypertensive retinopathy and cardiac dysfunction. Diagnosis is usually confirmed by raised 24 h free urinary catecholamine levels and their metabolites. Localization of tumour is done with CT scan, MIBG scan and PET scan. Preparation for surgery includes pharmacological control of adverse effects of circulatory catecholamine and restoration of blood volume by appropriate alpha blockade and achieve adequate control of blood pressure [Citation7,Citation8]. Beta blockers may also be sometimes necessary to control heart rate [Citation9]. We used both prazosin and propranolol in our case.
The goals of anaesthetic management aim at providing optimal surgical conditions and suppress the response to endotracheal intubation, surgical stimulation, tumour handling and revascularization. Epidural analgesia with general anaesthesia helps to increase vascular capacity and is the preferred method of anaesthesia [Citation10] (see ).
We successfully controlled blood pressure and heart rate with infusion of NTG, esmolol, isoflurane and intermittent bolus of propofol.
In conclusion, the diagnosis and management of paraganglioma in adults can also be applied in children. Early involvement of anesthesiologist is necessary. Apart from hypertension control, we should be ready for radical surgery including nephrectomy, vascular grafts and extensive re-construction of gastro-intestinal system to manage such complicated tumours. With better understanding of the pathophysiology of tumour, early diagnosis and good preoperative stabilization of patient, the surgical resection of paraganglioma has become safe even in children with tumours involving major vascular structures like in our case and operative mortality has reduced to 3%.
4 Key messages
The successful outcome to perioperative management of pediatric giant paraganglioma depends on adequate preoperative stabilization and intraoperative vigilance with careful titration of blood pressure controlling pharmacological agents. The cardiopulmonary bypass machine should be kept ready in case of any eventuality while dealing with a paraganglioma encasing major vascular structures of abdomen.
Contribution details
Conflict of interest
We have no conflict of interest to declare.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- J.M.Kissane9th ed.Anderson’ pathology1990C.V. Mosby Company1613
- R.H.StackpoleM.N.MelicowA.C.UsamPhaeochromocytoma in children. Report of 9 cases and review of first 100 published cases with follow up studiesJ Pediatr631963314330
- C.Prys-RobertsPhaeochromocytoma recent progress in its managementBr J Anaesthesia85120004457
- G.StringelS.H.EinR.CreightonD.DanemanN.HowardR.M.FillerPhaeochromocytoma in children. An updateJ Paediatric Surg1541980496500
- H.K.BruceL.R.TelenderJ.A.HeerdanPhaeochromocytoma in paediatric age group: current statusJ Paediatric Surg1861983879883 643–6
- J.N.CohnParoxysmal hypertension and hypervolemiaN Engl J Med.2751966643646
- J.R.KizerL.S.KoniarisJ.D.EddmanM.G.St John SuttonPhaeochromocytoma crisis. Cardiomyopathy and haemodynamic collapseChest1182000221223
- J.M.WallaceD.P.GillPrazocin in diagnosis and management of phaechromocytomaJAMA240197827522753
- J.PullertisEinSigmundM.S.WilliamsAnaesthesia for phaechromocytomaCan J Anaesthesia3551988526534
- Roizen Michael F, Fleisher Lee A. Anesthetic implications of concurrent diseases. Chapter 35; Miller’s Anesthesia. 7th ed. Philadelphia: Churchill Livingstone; p. 1084–5.