Abstract
PRES, a reversible white matter lesion characterized by cerebral edema, found in 7–20% of the patients with preeclampsia and eclampsia, needs early diagnosis and therapeutic intervention. We report PRES in a young preeclamptic primigravida and the role of dexmedetomidine in controlling her uncontrollable blood pressure in ICU. Dexmedetomidine, has cerebroprotective cardioprotective and renoprotective properties all of which, helped the patient improving clinically.
1 Introduction
PRES is a multifactorial cliniconeuroradiological syndrome characterized by headache, confusion, seizures, sometimes cortical visual disturbances, predominantly affecting the posterior circulation of the brain [Citation1]. The prompt control of blood pressure or discontinuation of the offending medication leads to the reversal of the clinical and radiologic abnormalities. When unrecognized, irreversible cytotoxic edema may occur [Citation2].
Here, we report PRES in a young preeclamptic primigravida and the role of dexmedetomidine in controlling her uncontrollable blood pressure in ICU.
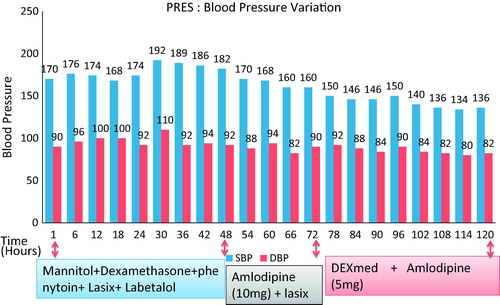
A 23 yrs postpartum patient was referred from Khanpur community health center to emergency department of PGIMS, Rohtak, as she became drowsy with poor mentation following normal preterm delivery of a IUGR baby. Antepartum history revealed that she was a known preeclamptic primigravida on regular antihypertensive medications and her premature induction of labor was done on 36th gestational week in view of uncontrollable high blood pressure (160/96 mmHg). She had no history of fits and her both past and family history was noncontributory. On examination in the emergency department patient was irritable with no response to any verbal commands. Vitals recorded were BP 140/90 mmHg, PR 96/min, Spo2 96% (on room air), normothermic, Resp. rate of 16/min, bilateral vesicular breath sounds audible with normal heart sounds. On pervaginal examination there was no fresh blood loss. All routine investigations were sent and ringer lactate drip was started. NCCT head was done. As the patient remained drowsy it was decided to shift the patient to ICU for close monitoring. Vitals recorded in the ICU were GCS 8/15 (E1 V2 M5), pt. was breathing spontaneously with resp. rate of 15/min, HR 76/min, BP 146/100 mmHg maintaining a Spo2 of 95% on Fio2 0.4 on ventimask. NCCT head revealed hypodensity in bilateral occipital region with no midline shift and intra cranial bleed which are the typical CT scan findings seen in Postpartum Reversible Encephalopathy Syndrome (PRES). Preemptive neuroprotective medications were started with Inj. Mannitol 100cc IV tds, Inj. Dexamethasone 8 mg IV tds and Inj Phenytoin 150 mg IV tds. Inj. Labetalol 10 mg IV tds and Inj Lasix 20 mg IV tds were also started. Routine investigations revealed Hb 9.9 gm/dl, TLC 29,000, DLC 88/10/1/1 platelets 1 lac, blood urea 94 mg/dl, blood sugar 96 mg/dl, serum sodium and potassium were 143 and 4.6 Meq/L respectively. Arterial blood gas revealed pH 7.42, Pco2 26.4, HCO3 16, Spo2 99.4%, SGOT/PT 51/69 IU/L, Serum ALP 384 IU/L, Serum Protein 5.5 gm/dl, A/G ratio 0.6, and Serum Cr 1.1 mg/dl. NIBP was regularly monitored and the BP remained high for the next 2 days with average BP at 184/96 mmHg. After physician opinion Tab Telmisartan 40 mg and Tab Amlodipine 10 mg were started on the 3rd postpartum day. Duplex scan done on both lower limbs ruled out chances of DVT. For the first 3 days patients remained agitated and were delirious with very high blood pressure. Dexmedetomidine infusion was added (3–7 μg/kg) to sedate as well to control the blood pressure. From 4th post partum day she showed signs of improvement in mentation and the average blood pressure remained at 150/94 mmHg. All intravenous medications were gradually stopped but Tab Telmisartan 40 mg and Tab Amlodipine 10 mg were continued. On 5th day patient was conscious with blood pressure at 140/86 mmHg (). Patient was shifted to ward and on 6th postpartum day she was discharged from hospital.
2 Discussion
PRES is mainly characterized by reversible white matter lesions; however, irreversible ischemic injury may occur due to delay in intervention. Though the exact etiopathogenesis remains unclear, it has been hypothesized that the cause of widespread endothelial dysfunction is due to sepsis, toxic agents or release of immunological mediators [Citation3]. In hypertensive patient rapid rise of blood pressure with abnormal cerebral autoregulation breaks the blood brain barrier and leads to cerebral edema in the posterior areas of the brain [Citation4]. When unrecognized, irreversible cytotoxic edema, infarction, hemorrhage and coma may occur. Clinical findings can mimic conditions such as stroke and vasculitis, as well as they are typically indistinguishable among cases of PRES, regardless of the underlying cause and hence can be misdiagnosed. Neuroimaging findings are diagnostic. It is mainly diagnosed by reversible hyperintensities on T2-weighted cranial MRI or bilateral symmetrical areas of low attenuation of white matter on CT scan which provides prognostic information that guides therapeutic decisions [Citation5]. Recognizing characteristic image findings is the key to diagnosing this syndrome and preventing deleterious workups or therapies. 7–20% of the patients with preeclampsia and eclampsia have PRES, as they are prone to excess fluid accumulation due to altered vascular reactivity, deficiency of vasodilating prostaglandins and endothelial dysfunction. Management of PRES mainly includes treatment of the underlying cause and maintaining normotension. Antiepileptics, antihypertensives and steroids (to reduce cerebral edema) are used to control PRES [Citation6].
Dexmedetomidine is a highly selective α2-adrenoreceptor agonist that produces dose-dependent sedation, anxiolysis, and analgesia (involving spinal and supraspinal sites) without respiratory depression making it a potentially attractive sedative for neurocritical care patients [Citation7]. Although α2-adrenoreceptors are located throughout the body, they are present in larger concentrations in vascular smooth muscle and in key arousal areas of the central nervous system (CNS), such as the locus coeruleus. The stimulation of α-2 receptors in the brain and spinal cord inhibits neuronal firing, which leads to hypotension, bradycardia, sedation and analgesia [Citation8]. Activation of presynaptic α2-adrenoreceptor on cortical blood vessels decreases norepinephrine release, whereas postsynaptic α2-adrenoreceptors may directly increase vascular smooth muscle tone so, rapid infusion or loading dose of dexmedetomidine may cause initial transient hypertension and it should be avoided [Citation8,Citation9]. It mainly decreases norepinephrine release by equally acting on α2A, α2B and α2C receptor subtypes [Citation10].
In our case the patient had postpartum neurological symptoms of headache, irritability and confusion with no history of seizures or visual disturbances. The BP recorded in the emergency department was 142/90 mmHg. Eventually she was diagnosed as PRES on CT scan. MRI was not done, as CT scan clearly showed hypodensity in the bilateral occipital region as well as definite history of preeclampsia excluded other factors causing PRES in this period. Recognizing the need for early therapeutic intervention to control blood pressure, patient was shifted to ICU for close monitoring of all vital parameters. She experienced a surge in blood pressure for the initial 2 days which was not controlled by intravenous labetalol, lasix, mannitol and NTG. On 3rd day tab. amlodipine was started with mild decrease in blood pressure. Then, it was decided to start infusion of dexmedetomidine (2–7 μg/dl) which controlled the blood pressure and also helped to improve the delirious state of the patient. Giving rapid infusion would have lead to further increase in blood pressure and hence it was avoided. It has cerebroprotective cardioprotective and renoprotective properties all of which improved our patient clinically.
Diagnosing PRES has important therapeutic implications because of its potential reversibility. Dexmedetomidine could be a rescue therapy for PRES, as it not only improves the hemodynamic parameters of the patient but also, has a known cerebroprotective as well as renoprotective effect, hence beneficial for two vital organs most affected by PRES. Dexmedetomidine could thus be considered as a treatment modality in patients with PRES, though more research in this field is warranted.
Conflict of interest
The authors declared that there is no conflict of interest.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- G.MerraA.Dal LagoL.NataleE.GaetaniA.CaricatoA.CianfoniA case of posterior reversible encephalopathy syndrome (P.R.E.S.)Int J Neurol11200815
- Devakinanda V.PasupuletiLetters to the editor: case report: posterior reversible encephalopathy syndromeAm Fam Physician7212200524302436
- W.S.BartynskiJ.F.BoardmanZ.R.ZeiglerR.K.ShadduckJ.ListerPosterior reversible encephalopathy syndrome in infection, sepsis, and shockAJNR Am J Neuroradiol27200621792190
- M.J.CipollaCerebrovascular function in pregnancy and eclampsiaHypertension5020071424
- V.FinocchiA.BozzaoM.BonaminiMagnetic resonance imaging in posterior reversible encephalopathy syndrome: report of three cases and review of literatureArch Gynecol Obstet271120057985 [Epub 2004 Oct 9. Review]
- N.KumarR.SimghN.SharmaA.JainAtypical presentation of PRES: two casesJOACP31201515
- Henry E.AryaKevin W.BoxbDaliaIbrahimcUshaDesirajubChristopher P.AmesaSafety and efficacy of dexmedetomidine in neurosurgical patientsBrain Injury2082006
- M.A.HaselmanDexmedetomidine: a useful adjunct to consider in some high-risk situationAANA J762008335339
- T.J.EbertJ.E.HallJ.A.BarneyThe effects of increasing plasma concentrations of dexmedetomidine in humansAnesthesiology932000382394
- O.PanzerV.MoitraR.N.SladenPharmacology of sedative-analgesic agents: dexmedetomidine, remifentanil, ketamine, volatile anesthetics, and the role of peripheral mu antagonistsCrit Care Clin252009451469