Abstract
Background
Retinal detachment surgery (RDS) is frequently associated with a high incidence of significant perioperative pain and oculocardiac reflex (OCR) intra-operatively. The peribulbar block has gained wide acceptance in ophthalmic anesthetic practice in the recent times. However, there is little current knowledge regarding its efficacy in RDS.
This prospective randomized clinical study evaluated the effect and feasibility of peribulbar block when used in conjunction with general anesthesia on perioperative outcome.
Methods
98 patients, ASA II-III, were randomly allocated to one of two groups to receive either peribulbar block in conjunction with general anesthesia (n = 49) or general anesthesia alone (n = 49).
Parameters compared were incidence of OCR, surgical bleeding, duration of surgery, postoperative pain and patient‘s satisfaction.
Results and discussion
Patients with PB block had a significantly lower incidence of intraoperative OCR (n = 4 vs. n = 13, p < 0.05). It also provided more effective post-operative analgesia with fewer patients requiring rescue analgesia medication (n = 19 vs. n = 27; p = 0.105). Surgical bleeding was more profuse in the general anesthesia group (n = 5 vs. n = 27, p < 0.001), with no cases of bleeding interfering with surgery in the peribulbar group.
Conclusions
PB block combined with GA improved significantly operating conditions and lower incidence of OCR. Patients in the block group also had better postoperative analgesia.
1 Introduction
Retinal detachment surgery (RDS) is frequently associated with a high incidence of significant perioperative pain [Citation1–Citation6] but it is often underestimated [Citation1]. It‘s also frequently associated with oculocardiac reflex (OCR), as a result of traction on the extraocular muscles or pressure on the eyeball [Citation2,Citation7,Citation8].
Needle-based ophthalmologic regional anesthesia (RA) was first described by Knapp [Citation9]. Then, in the early 20th century, Atkinson [Citation10] introduced the retrobulbar (RB) block. RB is a practical means to achieve analgesia and profound akinesia of the globe. The peribulbar (PB) block is a more recently introduced needle-based technique that varies from the RB block in terms of the depth and angulation of needle placement within the orbit. The RB blocks are accomplished by directing a needle toward the orbital apex with sufficient depth and angulation such that the cone is penetrated [Citation11]. The PB block is theoretically safer because the needle tip is kept at a greater distance from vital intraorbital structures and brain.
General anesthesia (GA) or RA either with RB or with PB blocks, is the usual method of providing anesthesia for RDS [Citation2]. In comparison with GA, RA reduces the incidence of OCR [Citation3,Citation7] and decreases postoperative pain [Citation3,Citation6].
RA is still widely used in cases of difficult surgery and extended time surgery [Citation12]. However, surgical dissatisfaction caused by insufficient akinesia with the partial blockade and patient discomfort during prolonged surgery are important limitations to the use of RA alone [Citation13–Citation15].
Traditionally, RB block was the local anesthetic method for ocular surgery. Because of the complications of RB block and the safety and effectiveness of PB block [Citation16,Citation17], the latter has gained wide acceptance in ophthalmic anesthetic practice in the recent times [Citation2].
The combination of GA and PB block may reduces these drawbacks [Citation4]. However, there is little current knowledge regarding the efficacy of PB block in RDS [Citation2–Citation4].
The aim of this study (the primary outcome) was to compare the postoperative pain and rescue analgesia requirements in the first two hours after surgery. Secondary outcomes of interest were to evaluate the efficacy and safety of PB block on perioperative outcome after RDS versus GA alone. The incidence of OCR, duration of surgery, surgical bleeding interfering with the surgical field and patient’s satisfaction were recorded.
2 Material and methods
After approval of the study from the Institutional Ethics Committee at 06-01-2015 and the written informed consent of each patient, 98 patients (ASA II-III) scheduled for elective RDS, were enrolled in this prospective randomized study. Exclusion criteria included age < 18 years, the usual contraindications for eye RA, clotting abnormalities, impaired mental status and patients who had been taking analgesics, drugs that might affect hemodynamics or any pro bleeding medication. All operations were performed by two experienced surgeons.
Patients were randomly allocated to one of two groups to receive either PB anesthesia in conjunction with GA (PB + GA group, n = 49) or GA alone (GA group, n = 49). The technique to be used for each patient was revealed by opening a sealed envelope.
All patients had a pre-anesthetic evaluation and were premedicated with oral midazolam 0.2 mg/kg (maximum 15 mg) given 60 min before surgery.
All punctures were performed in the induction room by an anesthesiologist experienced in the technique prior to the induction of GA under ASA standard monitoring. The study solutions were prepared by this physician at the bedside just before the injection.
In the PB-GA group, a single transcutaneous injection was performed using a 25-gauge 25 mm short-bevel needle into the peribulbar space through the inferior eyelid at the junction of the lateral third and the medial two thirds of the inferior orbital edge. After negative aspiration, 3–4 ml of 0.75% ropivacaine was slowly injected. Immediate complications while performing the block, including OCR, were noted. After the block, gentle digital ocular massage was given. Sensory block was assessed according to abolition of the corneal reflex and the eye was dressed until induction of anesthesia.
General anesthesia was induced with remifentanil (0.5–1 mcg/kg/min) and propofol (1.5–2.5 mg/kg) and a laryngeal mask airway (reinforced LMA) was inserted. Anesthesia was maintained with a mixture of O2/air and sevoflurane. The inspired concentration of sevoflurane was adjusted to maintain comparable depths of anesthesia (BIS values 40–60). Intra-operatively, heart rate (HR), ECG, SpO2, non-invasive blood pressure, end-tidal CO2 (target values: 30–40 mmHg) and Bispectral Index (BIS) were monitored. During surgery, an increase in mean arterial pressure (MAP) or HR more than 20% above the patient‘s baseline was treated with remifentanil infusion titrated stepwise by 0.05 mcg/kg/min increments. A drop of MAP below 30% of the patient‘s baseline was managed with adjustments to the rate of infusion of remifentanil or intravenous fluid boluses of 200 ml or ephedrine 5–10 mg boluses.
Postoperative analgesia was started 30 min before the end of surgery by administration of paracetamol 1 g and ketorolac 30 mg. Infusion of remifentanil was stopped as soon as the eye as been dressed (end of anesthesia).
Assessments were performed by the anesthetic responsible for providing general anesthesia and the surgeon.
The OCR was considered to present if the HR decreased by 20% from baseline value or if dysrhythmias or sinus arrest occurred during ocular manipulation [Citation3,Citation10]. If the heart rate did not increase after release of surgical manipulation, atropine 0.5 mg was then administered. Peri-operative bleeding was scored using a 3-point rating scale as follows: 0 = absent; 1 = bleeding does not interfering with surgery; 2 = bleeding interfering with surgery. A 10-point verbal numerical scale (VNS) (0 = no pain at all, 10 = the worst pain imaginable) was used to assess postoperative pain in the first two hours in post-anesthesia care unit (PACU). VNS was used for pain rather than a visual analogue scale (VAS) because of its simplicity and its correlation with VAS for pain and because patients with partial or total blindness might find it difficult to complete VAS [Citation18].
If the patient complained of pain postoperatively (VNS ⩾ 4), intravenous meperidine 10 mg was given as rescue medication. Bolus of meperidine 10 mg was administered until VNS < 4.
The evaluation of pain in the PACU was performed by a nurse blinded as to the treatment group.
Data were collected by the physician responsible for anesthesia during surgery and by nurses caring for the patient in the recovery room.
A global assessment of the entire anesthetic procedure was made using a 5-point verbal numeric scoring system (1 = very dissatisfied, 2 = dissatisfied, 3 = neither dissatisfied nor satisfied, 4 = satisfied, 5 = very satisfied).
The SPSS 21.0 (Statistical Package of Social Science) was used for all statistical analysis.
We chose meperidine consumption as the primary endpoint to calculate the required sample size for study. The number of patients was determined on the basis of the results of preliminary investigations during we established that for similar retinal surgery performed under G, the mean ± SD consumption of meperidine was 15 mg during the first 2 h postoperatively. The required sample was calculated to be 50 patients per group with α = 0.05 and a power of 90% to detect a difference of at least 25% in meperidine consumption.
The duration of surgery and patient satisfaction scores were compared using Mann-Whitney tests. The incidence of OCR, perioperative bleeding and rescue medication was compared by Chi-squared tests. Results were expressed as mean (SD) and p-values < 0.05 were considered statistically significant.
3 Results
Ninety-eight (forty-nine patients in each group) were included in this study. The two groups were comparable with respect to age, sex and ASA physical status ().
Table 1 Patient Characteristics.
The duration of surgery was longer in the GA group (120.9 ± 44.3 min versus 104.5 ± 30.4 min; ).
Table 2 Surgery characteristics and perioperative events.
Patients with PB block had a significantly lower incidence of intraoperative OCR (p < 0.05; ). While performing the PB block, none of the patients manifested an OCR.
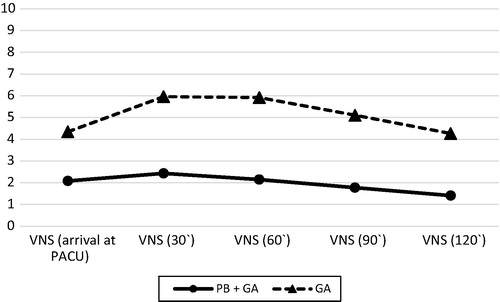
It also provided more effective post-operative analgesia with lower opioid consumption and fewer patients requiring rescue analgesia medication in the first two hours after the end of surgery (PB-GA group n = 19 vs. GA group n = 27, p = 1.05; ). The VNS for pain was greater in the GA group during the first two hours at the PACU compared with same values in the PB-GA group ().
There were no cases of bleeding interfering with surgery (grade 2) in the PB + GA group versus 9 cases in GA group. Surgical bleeding was reported by the surgeon as having been more profuse (grades 1 and 2) in the GA group than in the PB + GA group (p < 0.001).
Patients in the PB + GA group had higher general satisfaction scores than those in the GA group (4.5 vs. 4.2), although the generally satisfaction with anesthesia in both groups.
No differences in surgical procedures were reported between the two groups. No complications or incidents occurred in either group. All blocks were successful.
4 Discussion
In this randomized study, the use of PB plus GA was associated with a significantly lower incidence of intraoperative OCR. It also provided more effective post-operative analgesia with lower opioid consumption and fewer patients requiring rescue analgesia medication. These findings can be attributed to blocking the afferent limb of the OCR [Citation7] and reducing the afferent stimuli from muscle traction, preventing central hyperexcitability by noxious stimuli [Citation19]. Similar results have been described in previous studies [Citation2–Citation4,Citation20].
A crucial result of our study was the decreased bleeding observed in the PB + GA group. Surgical difficulties related to excessive bleeding were more frequent in the GA group and might have prolonged surgery. The reduced bleeding might possibly have been related to the decrease in intraocular pressure (IOP) induced by PB block [Citation3,Citation21]. Relaxation of extraocular muscles and the resulting decreased muscle traction on the sclera, and possibly a smaller intraocular blood volume resulting from the vasoconstrictive properties of ropivacaine, have been proposed to explain the reduction in IOP after PB block accomplished with ropivacaine [Citation3,Citation21]. This remains a hypothesis because IOP was not measured after PB block in our study.
In the PB + GA group there were observed episodes of hypotension (n = 23), despite was used the same protocol for induction and maintenance of general anesthesia in both groups. It is also very likely that relative hypotension contributed to the reduction in bleeding seen in this group. Deliberate induction of hypotension has been advocated as a means of facilitating intraocular surgery by reducing IOP [Citation22]. However, scientific proof of such an effect is lacking [Citation3].
In our study, we performed PB blocks with a small volume (3–4 ml) of ropivacaine with the intention to provide peri-operative analgesia rather than akinesia, and seems to be shown that ropivacaine is relatively safe and effective anesthetic for this type of surgery. Our results suggest that the beneficial effects of PB block combined with GA are primarily related to sensory block.
Complications associated with PB block are infrequent, but nevertheless do occur [Citation3], and can be catastrophic [Citation23]. Complications such as globe perforation, orbital hemorrhage, penetration of the optic nerve and the artery are reduced with this RA technique; however, the complications associated with RB block have been subsequently described with PB block with less, but still unacceptably frequency [Citation23–Citation27]. Moreover, RA itself can stimulate OCR [Citation2].
In our study, there were no complications due to PB block, including episodes of OCR while performing the block.
Patient satisfaction was higher in the PB + GA group, mainly due to the superior postoperative pain relief.
Overall, PB block combined with GA improved operating conditions and postoperative analgesia in RDS.
5 Conclusions
In conclusion, PB block combined with GA was superior to GA alone for RDS, resulting in more effective post-operative analgesia. Two crucial results of our study were a significantly better intra-operative surgical conditions and lower incidence of OCR in the PB block group.
These effects may thereby result in reduced postoperative ocular morbidity and better recovery from anesthesia. Further studies are needed to confirm whether other techniques of RA might offer the same benefit as PB block 0.75% ropivacaine.
Conflict of interest
None.
Acknowledgments
We thank the anesthesia department, in particular, Dr. Paulo Figueiredo (the director of the department) and the ophthalmology department of our institution (Centro Hospitalar de Entre o Douro e Vouga) that allowed this study to be conducted.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- S.MarzakY.MiloudiN.El HarrarA.BensaidK.ZaghoulA.AmraouiPostoperative pain in retinal detachment surgeryJ Fr Ophtalmol30102007992997 Dec
- D.ShendeS.SadhasivamR.MadanEffects of peribulbar bupivacaine as an adjunct to general anaesthesia on peri-operative outcome following retinal detachment surgeryAnesthesia552000970975
- J.MorelJ.PascalD.CharierPreoperative peribulbar block in patients undergoing retinal detachment surgery under general anesthesia: a randomized double-blind studyAnesth Analg102200610821087
- R.SubramaniamS.SubbarayuduV.RewariR.P.SinghR.MadanUsefulness of pre-emptive peribulbar block in pediatric vitreoretinal surgery: a prospective studyReg Anesth Pain Med2820034347
- M.MandelcornN.TabackE.MandelcornC.AnanthanaryanRisk factors for pain and nausea following retinal and vitreous surgery under conscious sedationCan J Ophtalmol341999281285
- N.WilliamsA.StruninW.HeriotPain and vomiting after vitreoretinal surgery: a potential role for local anaesthesiaAnaesth Intensive Care231995444448
- V.K.GroverN.BhardwajN.ShobanaS.P.GrewalOculocardiac reflex during retinal surgery using peribulbar block and nitrous narcotic anesthesiaOphthalmic Surg Lasers2931998207212 Mar
- C.E.AllisonJ.J.De LangeF.D.KooleW.W.ZuurmondH.H.RosN.T.van ShagenA comparison of the incidence of the oculocardiac and oculorespiratory reflexes during sevoflurane or halothane anesthesia for strabismus surgery in childrenAnesth Analg902000306310
- H.KnappOn cocaine and its use in ophthalmic and general surgeryArch Ophthalmol131884402
- W.S.AtkinsonRetrobulbar injection of anesthetic within the muscular coneArch Ophthalmol161936494
- S.GrayerOphthalmic anesthesia: more than meets the eyeA.J.SchwartzASA refresher courses in anesthesiology2006Lippincott Williams & WilkinsPhiladelphia55
- A.S.CrandallAnesthesia modalities for cataract surgeryCurr Opin Ophthalmol122001911
- A.M.GhaliA.M.El BtarnyThe effect on outcome of peribulbar anesthesia in conjunction with general anesthesia for vitreoretinal surgeryAnaesthesia652010249253
- E.CalendaP.OlleM.MuraineG.BrasseurPeribulbar ansthesia and sub-Tenon injection for vitreoretinal surgery: 300 casesActa Ophthalmol Scand782000196199
- R.S.NewsonA.C.WainwrightC.R.CanningLocal anesthesia for 1221 vitreoretina, proceduresBr J Ophthalmol852001225227
- D.B.DavisM.R.MandelPosterior peribulbar anesthesia: an alternative to retrobulbar anaesthesiaIndian J Ophthalmol3719895961
- P.N.ArnoldProspective study of a single-injection peribulbar techniqueJ Cataract Refractive Surg181992157161
- D.M.MurphyA.McDonaldMeasurement of pain: a comparison of VAS with non-visual analogue sideClin J Pain31988197199
- H.KehletControlling acute pain – role of preemptive analgesia, peripheral treatment, balanced analgesia and effects on outcomeM.MaxPain 1999 – an updated review1999IASP PressSeattle207212
- E.CalendaM.MuraineJ.C.QuintynG.BrasseurSub-Tenon infiltration or classical analgesic drugs to relieve postoperative painClin Exp Ophthalmol322004154158
- J.R.NocitiP.S.SerzedoE.B.ZuccolottoA.M.NunesS.B.FerreiraIntraocular pressure and ropivacaine in peribulbar block: a comparative study with bupivacaineActa Anaesthesiol Scand452001600602
- K.B.HollowayControl of the eye during general anaesthesia for intraocular surgeryBr J Anaesth521980671679
- L.RizzoM.MariniC.RosatiPeribulbar anesthesia: a percutaneous single injection technique with a small volume of anestheticAnesth Analg10020059496
- W.S.GrizzardN.M.KirkP.R.PavanM.V.AntworthM.E.HammerR.L.RosemanPerforating ocular injuries caused by anesthesia personnelOphthalmology98199110111016
- R.EdgeS.NavonScleral perforation during retrobulbar and peribulbar anesthesia: risk factor and outcome in 50,000 consecutive injectionsJ Cataract Refract Surg25199912371244
- M.S.LeeJ.F.RizzoS.LesselNeuro-ophthalmologic complications of cataract surgerySemin Ophthalmol172002149152
- C.M.KumarT.C.DowdComplications of ophthalmic regional blocks: their treatment and preventionOphthalmologica220220067382