Abstract
Background
Awake craniotomy (AC) is an attractive ‘minimally invasive’ anaesthetic technique for intracranial surgical procedures. There is dearth of information on the feasibility of this technique from developing countries.
Material and methods
This is a prospective descriptive study on all the patients who had AC for intracranial surgery over a 2-year period in a developing country. The data regarding their demographics, preoperative, intraoperative and postoperative anaesthetic events and any intraoperative complications were recorded.
Results
There were 18 patients, 11 (61.1%) males, mean age of 47.5 years (SD = 14.71). Propofol and Fentanyl were the sole agents providing conscious sedation during these surgical cases, while 0.25% Plain Bupivacaine and 1% Lidocaine with Adrenaline (1:200,000) were used for operative site anaesthesia. Most of the tumours, 7 (38.9%), were found in the parietal region of the brain; 9 (50.1%) patients had between 5 and 10 mm midline shift on brain MRI/CT Scan; metastatic tumours, 8 (44.4%), were the commonest lesions, and 13 (72.2%) had GCS of 15/15 prior to surgery. Hypertension and tachycardia, 3 cases (16.7%) in each, were the commonest intraoperative complications. All the patients successfully underwent the AC and none was admitted into the Intensive Care Unit postoperatively. At a mean follow-up of six months 10 (55.6%) patients were alive, 6 (33.3%) dead, and 2 (11.0%) of unknown status.
Conclusions
This audit showed AC to be a well-tolerated procedure with low rate of complications in our practice, an encouraging prospect for the feasibility of AC for intracranial surgical procedures in developing countries.
1 Introduction
Awake craniotomy (AC), initially promoted especially for surgical treatment of epilepsy, has subsequently found to be used for many other indications, including supratentorial tumours, arterio-venous malformation, deep brain stimulation, and mycotic aneurysms near critical regions of the brain [Citation1–Citation3]. The awake craniotomy technique in the dominant hemisphere in particular provides a more favourable outcome regarding postoperative language impairment [Citation4].
The importance of the brain in controlling vital functions in the body makes surgical operation a delicate process especially on a lesion located in functional areas; damaging such parts results in dire consequences. Therefore, surgical operations on functional cortical areas, such as the sensory, motor, language or visual, must be done meticulously without incurring undue neurological deficits postoperatively.
Although most craniotomies are still performed under general anaesthesia (GA) with endotracheal intubation for resection of an epileptogenic lesion close to vital areas of the brain (including those responsible for speech and motor activity), an “awake” craniotomy may be preferred to permit mapping of language, motor, and/or sensory area and electrocorticography (ECoG). During this procedure, there is always a concern about patient acceptability, cooperation and safety [Citation5].
Nevertheless, there is evidence that the technique of AC has ceased being considered only for its traditional roles in epilepsy surgery or lesionectomy in functional brain locations. Recently, awake craniotomy has been described as an approach for removal of all supratentorial convexital tumors, regardless of the involvement of eloquent cortex. This technique had a small complication rate and resulted in a considerable reduction in resource use by minimizing intensive care time and total hospital stay without compromising patient care [Citation6].
Awake craniotomy also has additional advantages over the traditional craniotomy with general anaesthesia. The patients have quick functional recovery and ultimately translate into decreased hospital expenses [Citation7,Citation8]. In this study, we present the results of a prospective audit of our initial experience with the perioperative anaesthetic management of the procedure of awake craniotomy in our university teaching hospital in a developing country.
2 Materials and methods
No human subjects were directly involved in this study. The medical records of patients who had intracranial lesions operated neurosurgically using the technique of AC between November 2011 and January 2015 at the University College Hospital, Ibadan, Nigeria were reviewed. All the patients were diagnosed with intra-axial lesions including tumours and haematomas with preoperative imaging studies done before and after the surgery. Discussions concerning each case were held in preoperative clinical meetings and informed consent from each patient or their closest relative was obtained before surgery. The anaesthetic evaluation paid particular attention to the cardiovascular, respiratory, and the renal systems to troubleshoot for any contra-indications. In addition, a pre-anaesthesia visit was paid to each patient a day before surgery on the ward. Anxious patients were pre-medicated with 10 mg oral diazepam the night before surgery. A thorough general physical examination coupled with detailed evaluation for eligibility for AC was done for each patient by the same anaesthetist. Patients were thoroughly evaluated for their fitness for the procedure of AC by both the anaesthetic and surgical teams. Intravenous (IV) fentanyl (1 μg/kg) was given to all the patients at the beginning of the each procedure, while IV Propofol was titrated to sedate them. This was as bolus doses and infusions. They all had scalp field block with a combination of 0.5% plain bupivacaine and 1% lignocaine with adrenaline (1:200,000). The anaesthetic methods used for the awake craniotomy included awake-asleep-awake, asleep-awake-asleep and asleep-awake. This depends largely on each patient’s intraoperative response to the techniques. The surgery fell into three phases: craniotomy, tumour resection and closing.
Apart from the fact of the suitability, determined by the neurosurgical and anaesthetic teams, of the cranial lesion for the procedure of AC, the other main inclusion criteria were patient’s consent, and the age: apart from one occasion in a 13-year-old, usually only patients aged 15 years and above were included in the study.
In the operation room all patients had anti-emetic prophylaxis, intravenous Ondansetron at 0.15 mg/kg. Prophylactic antimicrobials, anti-convulsants (as required) and corticosteroid (Dexamethasone at 0.1 mg/kg) were given to each patient immediately before surgery.
Patient’s positioning on the operating table and comfortability was ensured during AC. The heads were placed in a neutral position that maximally exposed the operation sites in a head ring without obstructing venous return. Head pins for patient positioning are not available in our low-resource practice. All our patients received supplemental oxygen via facial mask during the procedure. All the operations were performed by the same surgical team led by AOA, while all the anaesthetic management was also done by the same teams.
Next, the lead surgeon infiltrated the incision site with local anaesthesia following the knowledge of anatomical courses of the cutaneous nerves in relation to the incision sites (e.g. supraorbital nerve, occipital nerve, etc.). The anaesthetic agents used for the local infiltration were 10 ml to 30 ml of 1% lidocaine with 1:200,000 adrenaline and 0.5% bupivacaine mixed with equal volumes of sterile water. The dura was only infiltrated when pain was felt by the patient.
The data obtained were analysed using a Statistical Package for Social Science software, the SPSS version 20(SPSS Inc, Il, USA) and were presented in tables and figures. Descriptive statistics (frequency and percentage) were done for categorical variables.
3 Results
Awake craniotomy was carried out on 18 selected patients. The patients comprised 11 (61.1%) males and 7(38.9%) females with a mean age of 47.5 years (SD = 14.71), ranging from ages 13 to 66 years. The summary of the demographic data of the group is provided in . Seven (38.9%) of them were in the American Society of Anesthesiologists (ASA) Class I and II, while 61.1% was ASA class III.
Table 1 Some demographic characteristics of the patients.
All craniotomies were for full intracranial lesionectomy. None was for brain biopsy, nor for epilepsy per se. The most common preoperative symptoms among the patients were seizure in 10 (55.6%), headache in 8 (44.4%), hemiparesis in 7 (38.8%), altered sensorium in 3 (16.6%) and facioparesis in 1 (5.5%). There were 9 (50%) patient with history of significant co-morbidity, though all were well controlled. Fifteen (72.2%) of the patients had Glasgow Coma Scale (GCS) of 15 and 4 (27.8%) patients had GCS of 14.
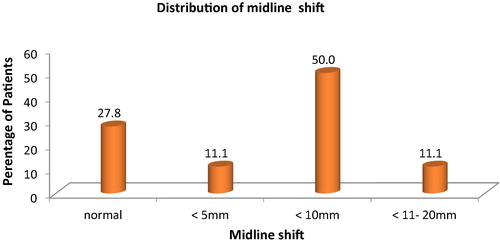
In the preoperative period, cranial computed tomography (CT) scan and/or Magnetic Resonance Imaging (MRI) was performed in all patients for the diagnosis of the intracranial lesion, and also for deciding the suitability of each case for the awake cranial surgical opening. The distribution of the midline shift on cross-sectional imaging (CT Scan and MRI) was as follows: it was absent in 5 (27.8%) patients; ⩽5 mm in 2 patients (11.1%); ⩽10 mm in 9 (50%) patients; and 11–20 mm in 2 (11.1%) patients, .
The lesions were more common on the right side of the brain, 13 (72.2%), while it was found on the left side in 5 (27.8%) of the cases. The commonest location was the Parietal lobe in 6 (33.3%), while extension to or from parietal lobe locations was found in 5 (27.7%). Ten (55.5%) cases had primary brain lesions, while 7 (44.5%) had metastatic brain lesions, . Sixteen (88.8%) of our patients had 20% Mannitol at the dose of 0.5 g/kg intraoperatively. The mean preoperative packed cell volume (PCV) was 38.5% (SD = 4.718) while the mean intraoperative estimated blood loss (EBL) was 531.7 ml: 5(27.8%) and 3 (16.7%) of the patients were transfused with 1 and 2 units of blood respectively, and 10 (55.6%) did not require any perioperative blood transfusion.
Table 2 The distribution of histology and complications.
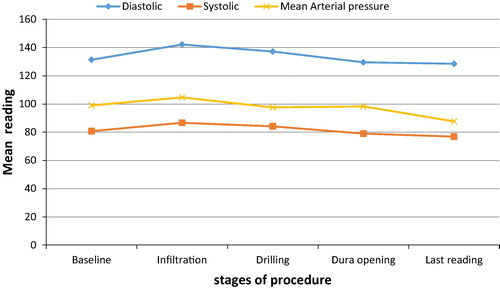
The haemodynamic changes recorded during the procedure, , showed baseline mean systolic, diastolic and mean arterial blood pressures as follows: 131.4, 80.8 and 97.7 mmHg respectively. During the time of infiltration of the scalp with the local anaesthetic agents, the mean systolic, diastolic and mean arterial blood pressures rose to 142.0, 86.7 and 105.1 mmHg respectively. During the drilling and opening of the skull the mean systolic, diastolic and mean arterial blood pressure had started to reduce to 137.2, 84.22 and 101.9 mmHg respectively. And by the time the dura was opened the mean systolic, diastolic and mean arterial blood pressure had further reduced to 129.6, 79.0 and 95.9 mmHg respectively. The last readings at the end of the procedure showed that mean systolic, diastolic and mean arterial blood pressure had gotten lower than the baseline values. They were 126.6, 76.0 and 93.4 mmHg respectively. The mean duration of surgery was 184 min (SD 45.19).
The sedation score for the 18 patients was between 4 and 5: majority 16 (88.9%) scored a mean of 5 (responds readily to name spoken in normal tone) on Observer’s assessment of alertness/sedation (OAA/S) scale score during the surgery, while the other patients scored mean of 4 (Lethargic responds to name in normal tone).
The commonest anaesthetic complication following the surgery was hypertension. This was found in 3 (16.7%) patients, as shown in .
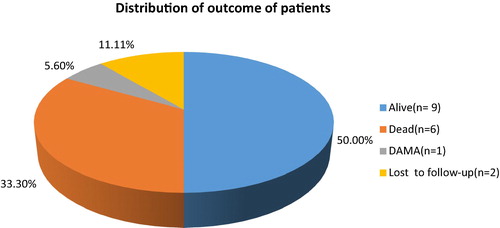
All the patients, apart from one who was discharged against medical advice for some personal reasons, were alive and in stable state one week post-operatively. Six months later 9 of them were still alive, 6 had died from progression of their diseases, and 2 were lost to follow-up, .
4 Discussion
Awake craniotomy first arose for its place in epilepsy surgery, but it has recently become an increasingly more frequent neurosurgical procedure, even for supratentorial tumoral and/ or non-tumoral lesions [Citation6]. Even when used for some other brain surgeries that are traditionally done under general anaesthesia the end points are encouraging. Awake surgery may be employed in extensive tumour resection in low-grade gliomas involving the functional areas, and it significantly improves the quality of life of patients [Citation6,Citation9,Citation10]. Awake craniotomy is also employed for stereotactic surgery, deep brain stimulation (DBS) surgery for Parkinson’s disease, and interventional pain procedures such as pallidotomy, thalamotomy and even in neuroendoscopic procedures involving ventriculostomy, endoscopy, including excision of small lesions [Citation11]. The traditional rationale for awake craniotomy in intracranial lesions is that it allows for brain mapping, which facilitates maximum resection and minimizes the risk of postoperative neurological deficits. Continuous assessment of neurological function has also facilitated the excision of tumors that might otherwise be considered inoperable. In this audit, our patients had supratentorial AC surgery in keeping with many reports in the literature [Citation6,Citation9–Citation11]. The peculiarity of AC made us to be highly selective of the cases in this study. There was a report where AC is now being used routinely and non-selectively for supratentorial tumour excision [Citation12]. The mean age of the patients was 47.5 years, and this is in contrast to other studies who found the mean age either lower, or higher than the mean age of this study [Citation13,Citation14]. Younger patients, especially children, can also undergo awake functional testing during craniotomy, although general anaesthesia is usually required for the first part of the procedure [Citation11,Citation15]. One of our patients who had AC was aged 13 years, according to Berger et al., the general consensus is that patients must be older than 11 years of age [Citation16].
In this study majority of the patients presented with seizure as one of the symptoms before the surgery. Other symptoms included headache, altered sensorium and facial asymmetry. This is in contrast to the report of Serletis and Bernstein, who found headache in patients who underwent awake craniotomy as the mostly reported deficit, followed by motor, speech, cognitive, visual and sensory deficits as well as seizures [Citation11]. Among patients who underwent AC and had intraoperative complication, 3 (37.5%) had hypertension, 3 (37.5%) had tachycardia, 1 (12.5%) had hypotension and 1 (12.5%) had on table focal seizure, that was transient (lasted less than 5 s). Only few 4 (22.2%) of our patients had postoperative complications, and this result is in contrast to the findings by Serletis and Bernstein, who found 14.8% as overall complication rate in their study including neurological deficits, wound complications, intraoperative events, postoperative medical events, and haematoma formation [Citation11] and with the findings by See et al., who found 39% as overall complication rate in their study on the anaesthetic management of awake craniotomy for tumour resection [Citation17].
Other postoperative complication found among our patients was aphasia (temporary), while deep vein thrombosis, hypotension and pulmonary oedema were as a result of the progression of the primary illness. The latter complications were found only in patients with metastatic diseases. Majority 17 (94%) of the patients were alive and in stable clinical state one week post operatively. The median duration of the hospital stay was 7 days. The patients were followed up for six months, and the study established that at least half 9 (50%) of the patients were still alive; a third 6 (33.3%) died from progression of their diseases, and 2 (11.11%) were lost to follow-up.
Skucas and Artru revealed that propofol infusion is the most commonly used sedative agent for awake craniotomy. Propofol as the only anaesthetic with spontaneously breathing patients has been described as safe [Citation18]. It is our choice of drug used as a sedative agent. Propofol unlike some volatile anaesthetics such as halothane, isoflurane, and sevoflurane among others, increases cerebral perfusion pressure, decreases neurophysiologic monitoring interference, appears to ensure neuroprotection and decreases the incidence of nausea and vomiting [Citation19].
Opioid addition to the sedative agent is the most utilized drug for analgesia in AC. It does not only improve the analgesic quality (scalp block already been done) but also reduces the requirements for hypnotics. A comparison of different types of opioids, including fentanyl, alfentanil, or sufentanil, found no significant difference in the operative condition, electrocorticography and stimulation testing [Citation20]. In another study by Manninen et al., a comparison of continuous remifentanil infusion or intermittent fentanyl, both narcotics yielded similar patient satisfaction, recall, and intraoperative complications, although fewer patients experienced reversible respiratory depression with the use of remifentanil [Citation21]. For a successful outcome of awake craniotomy anaesthesia must be effective and safe. Awake craniotomy, just like regional block, especially without sedation, offers the surgical/anaesthetic teams and the patients a real-time opportunity to interact during surgical operation. For this reason, patients scheduled for awake craniotomy should be well motivated, so that they can cooperate actively during the procedure so as to reduce postoperative neurological complications. Occasionally, a patient may be considered to be unsuitable due to emotional or psychological reasons; however, this is unusual and even teenagers have tolerated the procedure well [Citation6,Citation8].
5 Conclusion
There is increasing evidence from advanced neurosurgical anaesthetic units in the West that an awake craniotomy would be an appropriate choice for removal of many supratentorial tumors non-selectively. This study suggests a very encouraging prospect for the feasibility of AC for intracranial lesion resection even in low-resource practice regions of the world like our own.
Sources of support
No external support was received for this work.
Conflicts of interests
The authors of this study, each and all, declared no conflict of interests with any materials/devices mentioned in this work please.
Author contributions
AOA, SDA and OKI performed conception of study; AOA and OKI contributed to data gathering and analysis; OKI and AOA contributed to manuscript drafts; AOA and SDA supervised the intellectual and ethical contents; AOA, OKI and SDA approved the final manuscript for submission.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- K.J.BurchielH.ClarkeG.A.OjemannR.G.DaceyH.R.WinnUse of stimulation mapping and corticography in the excision of arteriovenous malformations in sensorimotor and language-related neocortexNeurosurgery241989322327
- H.DuffauL.CapelleJ.P.SichezT.FaillotL.AbdennourJ.D.Law KouneIntra-operative direct stimulations of the central nervous system: the Salptrière experience with 60 patientsActa Neurochir (Wien)141199911571167
- J.C.LüdersM.P.SteinmetzM.R.MaybergAwake craniotomy for microsurgical obliteration of mycotic aneurysms: technical report of three casesNeurosurgery562005 ONS-E201
- A.KannoN.MikuniEvaluation of language functions under awake craniotomyNeurol Med Chir552015367373
- F.PiccioniM.FanzioManagement of anaesthesia in awake craniotomyMinerva Anestesiol742008393408
- M.D.TaylorM.BernsteinAwake craniotomy with brain mapping as the routine surgical approach to treating patients with supratentorial intraaxial tumors: a prospective trial of 200 casesJ Neurosurg9019993541
- T.BrownA.H.ShahA.BregyAwake craniotomy for brain tumor resection: the rule rather than the exception?J Neurosurg Anesthesiol252013240247
- P.PeruzziS.D.BergeseA.ViloriaE.G.PuenteM.Abdel-RasoulE.A.ChioccaA retrospective cohort-matched comparison of conscious sedation versus general anesthesia for supratentorial glioma resection Clinical articleJ Neurosurg1142011633639
- L.C.M.PereiraK.M.OliveiraG.L.L’AbbateR.SugaiJ.A.FerreiraL.A.da MottaOutcome of fully awake craniotomy for lesions near the eloquent cortex: analysis of a prospective surgical series of 79 supratentorial primary brain tumors with long follow upActa Neurochir151200912151230
- O.SackoV.Lauwers-CancersM.SesayA.BrennerF.E.RouxAwake craniotomy vs surgery under general anesthesia for resection of supratentorial lesionsNeurosurgery68201111921199
- D.SerletisM.BernsteinProspective study of awake craniotomy used routinely and nonselectively for supratentorial tumorsJ Neurosurg107200716
- V.BonhommeC.FranssenP.HansAwake craniotomyEuro J Anaesthesiol742008393408
- D.LowI.NgW.H.NgAwake Craniotomy under local anaesthesia and monitored conscious sedation for resection of brain tumours in eloquent cortex-outcome in 20 patientsAnn Acad Med Singap362007326331
- A.HadabM.D.MohammedA.R.MohammedM.D.ArbabM.D.SalimA.H.SawsanAwake craniotomy an usual indicationJ Neurol Neurosci4201338233833
- C.HagbergA.GollasJ.BerryThe laryngeal mask airway for awake craniotomy in the pediatric patient: report of three casesJ Clin Anesth1620044347
- S.G.SorianoE.A.EldredgeF.K.WangL.KullJ.R.MadsenP.M.BlackThe effect of propofol on intraoperative electrocorticography and cortical stimulation during awake craniotomies in childrenPaediatr Anaesth1020002934
- J.J.SeeT.W.LewT.K.KwekK.J.ChinM.F.WongQ.Y.LiewAnaesthetic management of awake craniotomy for tumour resectionAnn Acad Med Singap362007319325
- A.P.SkucasA.A.ArtruAnesthetic complications of awake craniotomies for epilepsy surgeryAnesth Analg1022006882887
- P.HansV.BonhommeWhy we still use intravenous drugs as the basic regimen for neurosurgical anaesthesiaCurr Opin Anaesthesiol192006498503
- E.GignacP.H.ManninenA.W.GelbComparison of fentanyl, sufentanil and alfentanil during awake craniotomy for epilepsyCan J Anaesth401993421424
- P.H.ManninenM.BalkiK.LukittoM.BernsteinPatient satisfaction with awake craniotomy for tumor surgery: a comparison of remifentanil and fentanyl in conjunction with propofolAnesth Analg1022006237242