Abstract
Objectives
To compare the effect of remifentanil vs dexmedetomidine on hemodynamic response of noxious stimuli and neonatal outcome in preeclamptic parturient underwent C.S. under G.A.
Methods
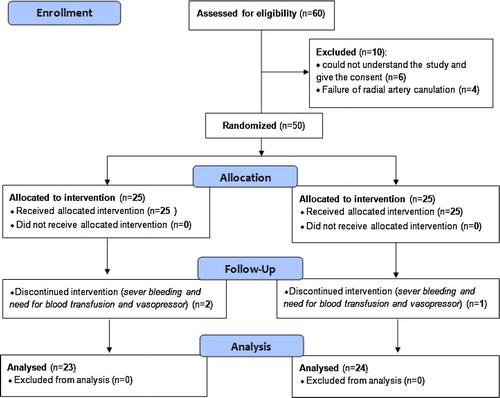
This blinded, prospective, randomized trial included 50 preeclamptic parturients underwent C.S under G.A., randomized into two equal groups [25 patients each]: group R [remifentanil]: received 1 μg/kg loading and 0.05 μg/kg/min infusion doses and group D [dexmedetomidine] received 1/kg loading and 0.2 μg/kg/h infusion doses. Maternal MAP and HR were assessed before medication (T0), just after induction of GA (TI), just after intubation (TT), two minutes after intubation (TT2), just after skin incision (TS), two minutes after skin incision (TS2), just after delivery of the baby (TD), and at the end of operation (TE). Time between induction and fetal delivery (I-D interval), time between incision of the uterus and delivery (U-D interval), and time between stop of the infusion of the tested drugs and delivery (D-D interval) were recorded. Neonatal Apgar score was recorded at 1 and 5 min and the need for resuscitative measures.
Results
Maternal MAP and HR in group R were statistically lower at (TI), (TT), (TT2), (TS) and (TS2). Neonatal Apgar score was statistically lower in group R with higher incidence for tactile stimulation.
Conclusion
Both remifentanil and dexmedetomidine were effective on blunting the pressor response to noxious stimuli in severely preeclamptic parturients. While remifentanil was marginally more effective in suppressing the pressor response, dexmedetomidine was safer for the neonates.
1 Introduction
General anesthesia (GA) is typically used for Cesarean Section (CS) when neuraxial anesthesia is contraindicated: such as with coagulation abnormalities, vertebral deformity, local infection, and patient refusal, or for emergency situations. Endotracheal intubation usually increases arterial blood pressure (ABP) and heart rate (HR) [Citation1]. With preeclampsia, this pressor response to intubation is exaggerated [Citation2]. This abrupt increase in ABP can cause cerebral edema, intracranial hemorrhage [Citation3], cardiac failure, and pulmonary edema, with increased rate of morbidity and mortality in both the mother and fetus [Citation4]. In addition, this pressor response raises maternal plasma catecholamine levels, that can induce utero-placental vasoconstriction and placental insufficiency [Citation5,Citation6]. Therefore, close control of pressor responses during intubation and surgical stimulation can protect both the mother and the fetus in preeclamptic parturients. Opioids are commonly used to attenuate this pressor response. However, because of its adverse neonatal effects, opioids are classically avoided at induction of GA for CS.
Remifentanil was a potent opioid with rapid onset (maximum effect at 1–3 min) [Citation7] and ultra-short duration of action, with a consistent half-time of 3–5 min, regardless of the duration of the infusion [Citation8]. It is an attractive option when GA is required for CS. It has been proved to blunt the pressor response to intubation in healthy [Citation9,Citation10] and severely preeclamptic [Citation11,Citation12] parturients, but the concern of neonatal respiratory depression still exists [Citation13]. The success to blunt the pressor response was defined as a systolic blood pressure (SBP) did not exceed 160 mmHg, a critical point for the risk of intracranial hemorrhage to occur in preeclamptic parturients [Citation14].
Dexmedetomidine, a highly selective α-2 adrenergic agonist, can induce sedation, analgesia, and amnesia without respiratory depression [Citation15,Citation16]. Preoperative administration of dexmedetomidine, either as a single dose (0.5–1 μg/kg) [Citation17,Citation18] or as continuous infusion (0.6 μg/kg/h) [Citation19], showed to effectively blunt hemodynamic and hormonal responses to tracheal intubation [Citation20], reduce anesthetic requirements [Citation21], and enhance postoperative analgesia [Citation22]. Several studies successfully used dexmedetomidine for labor analgesia or CS under GA, or to improve the quality of pain relief with opioid-based analgesia [Citation23,Citation24]. Other studies employed dexmedetomidine in the healthy [Citation25] and the preeclamptic [Citation26,Citation27] parturients for control of maternal hemodynamics. Later on, a study carried out on 2015, compared the efficacy of remifentanil on hemodynamics, depth of anesthesia, anesthetic consumption and neonatal outcome with that of dexmedetomidine in non-preeclamptic parturients [Citation28]. However, to our knowledge, no study compared the efficacy of these drugs with severe preeclampsia.
In our study, we aimed to compare the efficacy of remifentanil (1 μg/kg iv bolus followed by 0.05 μg/kg/min continuous infusion), with dexmedetomidine (1 μg/kg iv bolus followed by 0.2 μg/kg/min continuous infusion), for attenuation of the pressor response to endotracheal intubation and surgical stimulation, in severely preeclamptic parturient candidate for CS under GA, and to evaluate the neonatal outcome in both studied groups.
2 Materials and methods
Following approval of our institutional ethical committee and obtaining written informed consents, 50 parturients scheduled for elective CS under GA, of ASA grade I or II, 20–40 years old, presented with severe preeclampsia [Citation29,Citation30] were recruited in this blinded, prospective, and randomized, trial. This study was blinded to the data-collecting investigator and the studied drugs were prepared and administered by other investigators blind to the data collected.
GA was required when regional anesthesia was contraindicated or failed, or with patient refusal to regional anesthesia. This study was performed in the Kasr Al-Ainy University Hospitals over a period of six months started from March 2015.
Exclusion criteria included emergency cases, evidence of fetal compromise or intrauterine growth retardation, HELLP syndrome (hemolysis, elevated liver enzymes, and low platelet levels), morbid obesity, diabetes mellitus, or known allergies to the tested drugs. Parturients with history of cardiac, pulmonary, hepatic, renal or other diseases were also excluded. Preoperative monitoring of fetal heart sounds was applied to exclude fetal distress. Preoperatively, all patients were assessed clinically and investigated for the exclusion criteria. Complete blood count, bleeding profile, liver and kidney function tests were routinely recorded for all patients.
All patients were randomly allocated into two groups, Group R (remifentanil) and Group D (dexmedetomidine), using a computer generated randomization list and a sealed envelope technique (n = 25/group). An intravenous line was established and infusion of lactated Ringer’s solution was started at a rate of 15 ml/kg/h till delivery. All patients received a loading dose of iv magnesium sulfate (4 gm), followed by 1 gm/h iv infusion for seizure prophylaxis, and iv hydralazine (5 mg) at 20 min intervals when SBP > 160 mmHg or diastolic arterial pressure (DBP) >110 mmHg. All patients were fasted for six hours and pre-medicated with 30 ml of oral sodium citrate and iv ranitidine 150 mg and ondansetron 4 mg. Patients were placed in the supine position with left lateral tilt and preoxygenated with 100% O2 face mask over three minutes. ECG, pulse oximetry, capnography and train-of-four monitoring were applied. A left radial artery catheter was inserted under local anesthesia for invasive continuous blood pressure measurement.
In group (R), a bolus of intravenous (iv) remifentanil (1 μg/kg) was given over 30–60 sec, followed by a continuous infusion of (0.05 μg/kg/min), while in group (D), a bolus of iv dexmedetomidine (1 μg/kg) was given over 10 min, followed by a continuous infusion of (0.2 μg/kg/h). In both groups, the infusion was stopped with peritoneal incision.
Anesthesia was then induced in both groups with iv bolus of propofol (2 mg/kg) followed by a continuous infusion of 6–10 mg/kg/h, succinylcholine (1.5 mg/kg) was given, cricoid pressure was applied, the trachea was intubated and the patient was ventilated with a mixture of oxygen in air (50%). Atracurium 0.5 mg/kg was given after succinylcholine effect faded. After delivery, fentanyl 3 μg/kg and oxytocin (30 IU) in 500 ml Ringer’s solution were given. When skin suturing started, propofol infusion was stopped, atropine 0.02 mg/kg and neostigmine 0.05 mg/kg were used for reversal of neuromuscular block under train-of-four monitoring, and the patient was extubated when she was able to localize. Extubation time (from cessation of propofol infusion to extubation) was recorded.
Mean arterial blood pressure (MAP) and heart rate (HR) were recorded five minutes after radial arterial puncture (T0), just after induction of GA (TI), just after intubation (TT), two minutes after intubation (TT2), just after skin incision (TS), two minutes after skin incision (TS2), just after delivery of the baby (TD), and at the end of operation (TE).
Time between induction and fetal delivery (I-D interval), time between incision of the uterus and delivery (U-D interval), time between stop of the infusion of the tested drugs and delivery (D-D interval), and average dose of propofol required to maintain anesthesia were recorded.
Basic neonate examination was performed, Apgar score was recorded at 1 and 5 min, and the need for tactile stimulation, bag-mask ventilation, endotracheal intubation, or mechanical ventilation to the neonate, was recorded. If there was severe respiratory depression, intramuscular naloxone was given to restore ventilation, normal HR and skin color.
Maternal hypotension was defined as MAP < 60 mmHg or decreased more than 30% as compared to its baseline value. It was treated by increase in the rate of iv fluid infusion, followed by iv ephedrine 10 mg boluses. Bradycardia was defined as HR < 50 beats/min and treated with boluses of iv atropine 0.5 mg as required. Adverse effects (such as nausea and vomiting) for 24 h. after the operation were recorded.
3 Statistical analysis
For sample size calculation, mean arterial blood pressure (MAP) was taken as a primary parameter of interest. It was calculated that 21 subjects will be required per group in order to detect a 20% difference in MAP; the α value was 0.05 and the power (1 − β) of the study was 0.80. We enrolled 50 patients (25/group) to allow for dropouts.
Data were analyzed using the SPSS statistics program (Version 16, SPSS Inc, Chicago, IL, USA). According to the type of data they were represented as mean and standard deviation or frequencies and percentages. Comparisons of the two studied groups were performed using either Student t-test (for parametric measures) or Mann-Whitney U test (for nonparametric measures). In all tests results were considered statistically significant if p value was less than 0.5 (see ).
4 Results
The results of the present study showed NO statistically significant difference between the two groups as regards the patients’ characteristics (age, weight and height), average dose of propofol required to maintain anesthesia, and the operative data [duration of the surgery, time between induction and fetal delivery (I-D interval), time between incision of the uterus and delivery (U-D interval), and time between stop of the infusion of the tested drugs and delivery] ().
Table 1 Demographic data of the patients and operative data in the two studied groups.
As regards the mean arterial pressure (MAP) and heart rate (HR), the present study showed that the MAP was statistically significant lower in remifentanil group (R) compared to dexmedetomidine group (D) when measured just after induction (TI), and it was also statistically significant lower compared to the baseline reading (T0) in both groups. When measured just after intubation (TT) and two minutes later (TT2), and just after skin incision (TS) and two minutes later (TS2), both MAP and HR showed slight increase compared to the baseline reading (T0) but it was still lower in group (R) compared to group (D). Later, after delivery of the baby and at the end of the surgery, both MAP and HR showed NO statistically significant difference between the two studied groups ( and ).
Table 2 Mean arterial pressure (MAP) in the two studied groups.
Table 3 Heart rate (HR) in the two studied groups.
As regards the neonatal outcome and need for resuscitation, the results of the present study showed that the Apgar score was statistically significant lower in group (R) compared to group (D), at both 1 min [6 (4–8) and 7 (5–9)], and 5 min [8 (6–9) and 9 (7–9)], respectively. Consequently, the number of neonates required resuscitative measures was clinically higher in group (R) [40% required tactile stimulation, 12% required bag-mask ventilation and 4% required tracheal intubation] compared to group (D) [24% required tactile stimulation, 4% required bag-mask ventilation and 0% required tracheal intubation]. But, only the number of patients required tactile stimulation was statistically significant (). None of the neonates required naloxone to restore spontaneous ventilation. There were NO maternal or neonatal complications noticed in both groups.
Table 4 Neonatal outcome and resuscitation measures in the two studied groups.
5 Discussion
The present study showed a successful influence of both remifentanil and dexmedetomidine for blunting of stress response to tracheal intubation and skin incision in severely preeclamptic parturients. However, remifentanil was marginally more effective than dexmedetomidine, while dexmedetomidine showed a safer profile on the neonatal outcome. Remifentanil-exposed neonates showed lower Apgar score at the 1st. and 5th min which required more resuscitative measures (tactile stimulation), but neonates in both groups did not require aggressive resuscitation measures in form of tracheal intubation and subsequent mechanical ventilation.
The results of the present study were in agreement with the study done by Yoo et al. [Citation11] who examined different doses of remifentanil to attenuate the pressor response to airway management in severely preeclamptic underwent C.S. under G.A., which showed that the effect of remifentanil was dose-dependent with ED50 and ED95 of remifentanil were 0.59 and 1.34 μg/kg respectively.
Again, the results of the present study were in accordance with those of the study done by Park et al. [Citation12] who examined two doses of remifentanil (0.5 and 1.0 μg/kg) on attenuating the hemodynamic response to tracheal intubation in preeclamptic patients underwent C.S. under G.A. which showed that both doses successfully maintained the blood pressure and heart within the baseline preoperative values after intubation with the dose of 1.0 μg/kg was more effective.
But contrary to the present study, the results of Park et al. [Citation12] showed more lower Apgar score of the neonates at 1 and 5 min and more need for resuscitative measures (in the 1.0 μg/kg remifentanil group, Apgar score was <7 in 58% of the neonates and 25% of them required tracheal intubation). These contradictions with the present study could be explained by the longer U-D interval in their study (115 ± 61 sec) compared to the present study (74.8 ± 17) at the same dose of remifentanil.
Also, the results of the present study were in agreement with those of the study done by Saleh ElSayed [Citation27] which showed that dexmedetomidine infusion of 0.4 μg/kg/h was superior to fentanyl single dose of 1 μg/kg to suppress the hemodynamic response to surgical stimulation in preeclamptic parturients underwent C.S. under G.A. with the neonatal outcome was comparable between the two groups. Although a lower dose of dexmedetomidine infusion was used in the present study (0.2 μg/kg/h), the use of loading dose (1 μg/kg), together with the use of propofol total intravenous anesthesia and MgSO4 and hydralazine (if needed), all these factors could compensate for the difference between the two studies in the maintenance dose of dexmedetomidine.
Contrary to the present study, the results of study done by El-Tahan et al. [Citation25], showed that dexmedetomidine was more effective in doses 0.4 and 0.6 μg/kg/h rather than the 0.2 μg/kg/h dose in attenuating the pressor response to noxious stimuli. This contradiction as regards the proven effect of the low dose 0.2 μg/kg, (used in the present study) may attribute to the total intravenous anesthesia using propofol and also to the preoperative use of MgSO4 and hydralazine to control the blood pressure in the present study.
The results of the present study were matched with those of the recent study done by Li et al. [Citation28] who compared the effects of both remifentanil and dexmedetomidine on both the parturient hemodynamics and the neonatal outcome in non-preeclamptics underwent C.S. under G.A. and showed that remifentanil was more potent in suppressing the MAP response to noxious stimuli, although dexmedetomidine showed lower heart rate values intraoperatively, but the neonatal outcome was in favor of dexmedetomidine as Apgar score was higher at 1 and 5 min and less neonates required bag-mask ventilation compared to remifentanil. These neonatal depressive effects of remifentanil may be attributed to their use of higher loading dose (2 μg/kg) compared to the dose, (1 μg/kg or less), used in the present study and studies done by other investigators [Citation11,Citation12,Citation31].
There were some limitations of our study. One of them was the lack of resources to compare plasma levels of the studied drugs in both parturient and neonate circulations. Our study was not designed to estimate the preemptive analgesic effect of studied drugs on postoperative analgesia after CS, hopping to do so in further studies. Also, our study excluded cases with fetal distress, one of the main indications for CS under GA. We excluded them from the current study due to the lack of proof about their effect on neonatal outcome.
6 Conclusion
Both remifentanil and dexmedetomidine were effective on blunting the pressor response to noxious stimuli in severely preeclamptic parturients. While remifentanil was marginally more effective in suppressing the pressor response, dexmedetomidine was safer for the neonates.
Conflict of interest
We have no conflict of interest to declare.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- C.Prys-RobertsL.T.GreeneR.MelocheP.FoëxStudies of anaesthesia in relation to hypertension. II. Haemodynamic consequences of induction and endotracheal intubationBr J Anaesth431971531547
- H.ConnellJ.G.DalgleishJ.W.DowningGeneral anaesthesia in mothers with severe pre-eclampsia/eclampsiaBr J Anaesth59198713751380
- C.-J.HuangY.-C.FanP.-S.TsaiDifferential impacts of modes of anaesthesia on the risk of stroke among preeclamptic women who undergo Caesarean delivery: a population-based studyBr J Anaesth1052010818826
- E.G.LawesJ.W.DowningP.W.DuncanB.BlandN.LaviesG.A.GaneFentanyl-droperidol supplementation of rapid sequence induction in the presence of severe pregnancy-induced and pregnancy-aggravated hypertensionBr J Anaesth59198713811391
- P.G.LoughranJ.MooreJ.W.DundeeMaternal stress response associated with caesarean delivery under general and epidural anaesthesiaBr J Obstet Gynaecol931986943949
- T.GinM.E.O’MearaA.F.KanR.K.LeungP.TanG.YauPlasma catecholamines and neonatal condition after induction of anaesthesia with propofol or thiopentone at caesarean sectionBr J Anaesth701993311316
- P.S.GlassD.HardmanY.KamiyamaT.J.QuillG.MartonK.H.DonnPreliminary pharmacokinetics and pharmacodynamics of an ultra-short-acting opioid: remifentanil (GI87084B)Anesth Analg77199310311040
- A.KapilaP.S.GlassJ.R.JacobsK.T.MuirD.J.HermannM.ShiraishiMeasured context-sensitive half-times of remifentanil and alfentanilAnesthesiology831995968975
- W.D.Ngan KeeK.S.KhawK.C.MaA.S.Y.WongB.B.LeeF.F.NgMaternal and neonatal effects of remifentanil at induction of general anesthesia for cesarean delivery: a randomized, double-blind, controlled trialAnesthesiology10420061420
- G.DraisciA.ValenteE.SuppaL.FrassanitoR.PintoF.MeoRemifentanil for cesarean section under general anesthesia: effects on maternal stress hormone secretion and neonatal well-being: a randomized trialInt J Obstet Anesth172008130136
- K.Y.YooD.H.KangH.JeongC.W.JeongY.Y.ChoiJ.LeeA dose-response study of remifentanil for attenuation of the hypertensive response to laryngoscopy and tracheal intubation in severely preeclamptic women undergoing caesarean delivery under general anaesthesiaInt J Obstet Anesth2220131018
- B.Y.ParkC.W.JeongE.A.JangS.J.KimS.T.JeongM.H.ShinDose-related attenuation of cardiovascular responses to tracheal intubation by intravenous remifentanil bolus in severe pre-eclamptic patients undergoing Caesarean deliveryBr J Anaesth10620118287
- M.HeesenS.KlöhrT.HofmannR.RossaintS.DevroeS.StraubeMaternal and foetal effects of remifentanil for general anaesthesia in parturients undergoing caesarean section: a systematic review and meta-analysisActa Anaesthesiol Scand5720132936
- J.N.MartinB.D.ThigpenR.C.MooreC.H.RoseJ.CushmanW.MayStroke and severe preeclampsia and eclampsia: a paradigm shift focusing on systolic blood pressureObstet Gynecol1052005246254
- J.E.HallT.D.UhrichJ.A.BarneyS.R.ArainT.J.EbertSedative, amnestic, and analgesic properties of small-dose dexmedetomidine infusionsAnesth Analg902000699705
- T.KamibayashiM.MazeClinical uses of α2-adrenergic agonistsAnesthesiology93200013451349
- V.HanciG.ErdoğanR.D.OkyayB.S.YurtluH.AyoğluY.BaydilekEffects of fentanyl-lidocaine-propofol and dexmedetomidine-lidocaine-propofol on tracheal intubation without use of muscle relaxantsKaohsiung J Med Sci262010244250
- H.BasarS.AkpinarN.DoganciU.BuyukkocakC.KaymakO.SertThe effects of preanesthetic, single-dose dexmedetomidine on induction, hemodynamic, and cardiovascular parametersJ Clin Anesth202008431436
- T.KunisawaO.NagataM.NagashimaS.MitamuraM.UenoA.SuzukiDexmedetomidine suppresses the decrease in blood pressure during anesthetic induction and blunts the cardiovascular response to tracheal intubationJ Clin Anesth212009194199
- V.M.KeniyaS.LadiR.NaphadeDexmedetomidine attenuates sympathoadrenal response to tracheal intubation and reduces perioperative anaesthetic requirementIndian J Anaesth552011352357
- M.YildizA.TavlanS.TuncerR.ReisliA.YosunkayaS.OtelciogluEffect of dexmedetomidine on haemodynamic responses to laryngoscopy and intubation: perioperative haemodynamics and anaesthetic requirementsDrugs R D720064352
- J.MálekF.MarecekL.HessA.KurzováM.OcadlíkM.VotavaA combination of dexmedetomidine with ketamine and opioids results in significant inhibition of hemodynamic changes associated with laparoscopic cholecystectomy and in prolongation of postoperative analgesiaRozhl v Chir Měsíčník Československé Chir Společnosti892010275281
- A.PalanisamyR.J.KlickovichM.RamsayD.W.OuyangL.C.TsenIntravenous dexmedetomidine as an adjunct for labor analgesia and cesarean delivery anesthesia in a parturient with a tethered spinal cordInt J Obstet Anesth182009258261
- S.A.Abu-HalawehA.-K.S.Al OweidiH.Abu-MaloohM.ZabalawiF.AlkazalehH.Abu-AliIntravenous dexmedetomidine infusion for labour analgesia in patient with preeclampsiaEur J Anaesthesiol2620098687
- M.R.El-TahanH.A.MowafiI.H.Al SheikhA.M.KhidrR.A.Al-JuhaimanEfficacy of dexmedetomidine in suppressing cardiovascular and hormonal responses to general anaesthesia for caesarean delivery: a dose-response studyInt J Obstet Anesth212012222229
- A.El-SakkaN.HelmyJ.HelmyH.RafaatThe hemodynamic and analgesic profile of dexmedetomidine against fentanyl in preeclamptic parturients undergoing Cesarean section under general anesthesiaAin-Shams J Anaesthesiol82015183
- R.S.Saleh ElSayedStudy of the effect of dexmedetomidine in reducing hemodynamic responses to general anesthesia for elective cesarean section in patients with preeclampsiaJ Anesth Clin Res62015
- C.LiY.LiK.WangX.KongComparative evaluation of remifentanil and dexmedetomidine in general anesthesia for cesarean deliveryMed Sci Monit21201538063813
- W.GogartenPreeclampsia and anaesthesiaCurr Opin Anaesthesiol222009347351
- G.LambertJ.F.BrichantG.HartsteinV.BonhommePYD. Preeclampsia: an update. BelgicaActa Anaesthesiol652014137149
- A.PournajafianF.RokhtabnakA.KholdbarinM.GhodratiS.GhavamComparison of remifentanil and fentanyl regarding hemodynamic changes due to endotracheal intubation in preeclamptic parturient candidate for cesarean deliveryAnesthesiol Pain Med220129093