Abstract
Background and objective
In this study we evaluated oral ivabradine (a relatively new heart rate lowering agent) versus oral propranolol (a classic commonly used beta-blocker) in achieving a hemodynamic stability and controlling possible changes in blood glucose level due to stress response in microlaryngoscopic surgeries.
Methods
A total of 50 American Society of Anesthesiologists (ASA) 1,2 patients scheduled for microlaryngoscopic surgeries were included in this prospective, randomized controlled double blind study. They were given either oral ivabradine (5 mg tablet) group I or oral propranolol (10 mg tablet) group P in the evening before the operation and 1 h before the induction of anesthesia. Hemodynamic variables (systolic, diastolic, mean blood pressure and heart rate) and blood glucose level were recorded perioperatively.
Results
The changes in blood pressure and heart rate in both groups were mild after intubation, laryngoscope fixation for surgery and extubation but these changes in ivabradine group were significantly less than the changes in propranolol group (P < 0.05). No significant difference (P > 0.05) was found between both groups in blood glucose level perioperatively. No statistically significant complications were observed in both groups.
Conclusion
Premedication with 5 mg of oral ivabradine or 10 mg of oral propranolol before microlaryngoscopic surgeries was effective in achieving a good degree of hemodynamic stability but ivabradine was more effective. Both drugs didn’t show an obvious effect on blood glucose level perioperatively. No complications were recorded.
1 Introduction
There has been an increase in laryngoscopic surgeries which may be due to the marked increase in laryngeal tumours in recent years. Laryngeal tumours may be benign or malignant including vocal nodules, vocal polyps, vocal fold cysts and papilomas. Poor vocal hygiene and smoking are often considered to be risk factors. In some cases, in order to obtain an accurate diagnosis of a vocal fold lesion it is necessary to perform laryngoscopy, which also allows for proper dysphonia treatment through microsurgery [Citation1]. Manipulation of the larynx such as laryngoscopy and tracheal intubation is associated with hemodynamic response consisting of an increase in heart rate, arterial blood pressure, myocardial oxygen demand and induction of dysrhythmias. In microlaryngoscopic surgery, these responses are more intense [Citation2]. In patients with coronary artery disease, hypertension or cerebrovascular disease, these changes may precipitate myocardial ischemia, myocardial infarction and cerebral hemorrhage [Citation3,Citation4]. Laryngoscopy and surgical procedures also induce complex stress responses, manifested by metabolic, neurohumoral, and immunological changes. Hyperglycemia is a feature of this metabolic response [Citation5].
Table 3 Changes in DBP.
Table 4 Changes in MBP.
The choices of premedication and anesthetic techniques are able to influence the neurohormonal stress response by modulating the pathophysiological pathways [Citation6–Citation8].
Ivabradine is a very unique drug. It is a highly selective inhibitor of ‘If’ channels (funny current or funny channels or pacemaker current). It is useful in patients with angina pectoris, coronary artery disease and heart failure. Ivabradine is quite different from a beta blocker as it reduces the heart rate without jeopardizing hemodynamics in unhealthy, compromised patients [Citation9]. The drug can be used not only in hypertensive patients but also in normotensive patients, diabetic patients and patients with bronchial asthma where beta blockers are contraindicated [Citation10].
The rationale of the present study is to minimize stress response in microlaryngoscopic surgeries. We evaluated the effect of oral ivabradine on the hemodynamics and blood glucose level in these surgeries under general anesthesia compared with a commonly used beta-blocker propranolol given orally.
2 Patients and methods
This was a prospective, randomized, double blind, comparative clinical study performed in Ain Shams University Hospitals from March 2015 till October 2015. After getting approval from the institutional ethical committee, an informed consent was taken from every patient enrolled in the study.
Fifty patients aged ⩾25 to ⩽60 years, planned for elective microlaryngoscopic surgeries were included in this study. The exclusion criteria included the following: ASA physical status >2, taking beta-blockers or sedatives or antihypertensives, inability to communicate with the patient due to any reason, patients with history of respiratory troubles or diabetes mellitus and those with anticipated difficult airway. Exclusion criteria also included patients with history of chest pain, palpitations, syncope or with baseline heart rate <60 beats per minute, baseline systolic blood pressure <100 mm Hg and those with ECG abnormalities. Routine preoperative investigations were done for all patients.
The patients were randomly allocated by simple randomization into two groups (having 25 patients in each group):
GROUP I: who received oral ivabradine, 5 mg one tablet at 8.00 pm in the evening before the day of the surgery and one 5 mg tablet one hour before the induction of anesthesia.
GROUP P: who received oral propranolol, 10 mg one tablet at 8:00 pm in the evening before the day of the surgery and one 10 mg tablet one hour before the induction of anesthesia.
Randomization sequence was concealed in sealed envelopes performed by the help of an independent personnel. An appropriate code number was assigned to each patient, with an allocation ratio of 1:1. The test medications were given to patients by an attending anesthesiologist who was not involved in patient care or data collection. Data collection was carried out by investigators in a double-blind manner. All patients, investigators and anesthesiologists were blinded to the administered test drugs.
No hypnotic medication was given on the evening before surgery. Patients were premedicated with glycopyrrolate 0.02 mg/kg i.v. and ondansetron 4 mg i.v. in the preoperative room. Upon arrival in the operating room, monitors were attached to the patients and heart rate, NIBP, oxygen saturation, temperature, end tidal CO2, and ECG were recorded.
After pre-oxygenation with O2 100% for 3 min, anesthesia was induced with a standard anesthetic protocol using midazolam 0.03 mg/kg, fentanyl 1 μg/kg, thiopentone sodium 3–5 mg/kg, and tracheal intubation was facilitated by atracurium 0.5 mg/kg intravenously. Lungs were mechanically ventilated with O2 50% and anesthesia was maintained with isoflurane 0.8% and atracurium 0.1 mg/kg every 25 min. Ventilation was adjusted to maintain normocapnia (end-tidal carbon dioxide [EtCO2] 40 ± 5 mmHg). After tracheal intubation with a cuffed endotracheal tube (size 5.0–5.5), the surgeon fixed the laryngoscope and the procedure started. During surgery, Ringer’s lactate solution was administered in maintenance dose as per Holliday-Segar formula. The anesthesiologists were ready to manage any hypotension (MAP < 20% preoperative) with a fluid bolus of normal saline 250–300 ml and ephedrine 15 mg i.v if needed. Any incidence of bradycardia (HR < 50/min) was ready to be treated with atropine 0.7 mg i.v.
At the end of the surgery, residual neuromuscular block was reversed by the injection of neostigmine 0.05 mg/kg and glycopyrrolate 0.02 mg/kg i.v. and the patients were extubated when respiration was sufficient, and they were able to obey commands.
Patients were transferred to the postanesthesia care unit (PACU) where they were monitored for at least 3 h for any evidence of complications or adverse events. Systolic (SBP), diastolic (DBP), mean (MBP) arterial blood pressures and heart rate (HR) were recorded at the following points of time:
| (1) | Baseline in the evening before the day of operation immediately before taking the test drugs. | ||||
| (2) | Immediately before induction of anesthesia. | ||||
| (3) | One minute after intubation. | ||||
| (4) | Three minutes after intubation. | ||||
| (5) | Five minutes after laryngoscope fixation. | ||||
| (6) | Fifteen minutes after laryngoscope fixation. | ||||
| (7) | One minute after extubation. | ||||
| (8) | Three minutes after extubation. | ||||
Blood samples were analyzed by glucometer (Abbott Optium Xceed) for blood glucose level at the following points of time:
| (1) | Baseline. | ||||
| (2) | Immediately before induction of anesthesia. | ||||
| (3) | Ten minutes after intubation. | ||||
| (4) | One hour after extubation. | ||||
The results obtained in the study are presented in tabulated manner.
The primary outcomes of our study were as follows: systolic blood pressure, diastolic blood pressure, mean blood pressure and heart rate. The secondary outcome was blood glucose level and any possible side effects of the 2 drugs.
2.1 Statistics
Statistical presentation and analysis of the present study were conducted, using the mean, standard deviation, Chi-square, paired t-test and unpaired t-test by SPSS V.20. Unpaired Student T-test was used to compare between the two groups in quantitative data. Fisher’s exact test and Yates’ corrected chi-square are computed for 2 × 2 tables.
2.2 Sample size
The sample size was calculated using Epicalc 2000 software depending on the results from previous studies 4 and 11 with the following parameters:
Type I error (α) = 5% with confidence level 95% and power of study 90% (power of test) with type error II 10% (Beta) with expected difference of 0.32. The minimal sample size was 23 in each group. A total of 25 patients in each group were included to compensate for possible dropouts. Corresponding P was computed. P < 0.05 was considered as statistically significant.
2.3 Significant level
Non-significant >0.05, significant <0.05∗, highly significant <0.001∗.
3 Results
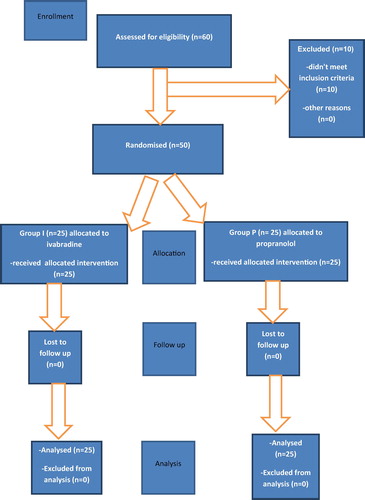
Sixty patients were primarily enrolled in the study. Ten patients were then excluded as they didn’t meet the inclusion criteria ().
Fifty patients were then finally included in the study and divided into two equal groups. There were no significant differences between the two groups as regards demographic data such as age, sex, weight and ASA grade ().
Table 1 Demographic data.
Baseline and preinduction data (SBP, DBP, MBP and HR) were compared between the two groups of patients and no significant difference was found. Systolic arterial pressure, diastolic blood pressure, mean blood pressure and heart rate increased slightly after intubation in both groups.
However in group I, the increase in these parameters was less than in group P and it was statistically significant. SBP, DBP, MBP and HR increased slightly again after laryngoscope fixation for surgery and also in group I the increase was less than in group P and it was statistically significant. After extubation, values showed that the rise in group I in such parameters was also less than in group P and it was also statistically significant (–).
Table 2 Changes in SBP.
Table 5 Changes in HR.
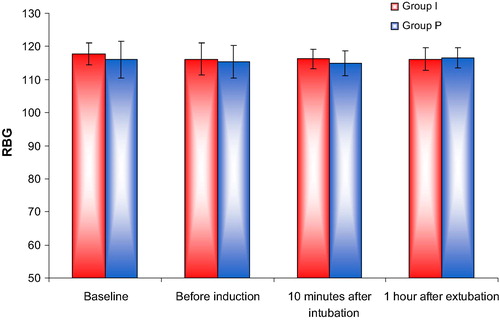
Random blood glucose level (RBG) was analyzed in the patients. Preinduction values were less than baseline values in the two groups but that were not statistically significant. Slight increase in blood glucose level was noticed in both groups shortly after intubation and after extubation but that was also not statistically significant ().
No incidence of possible side effects (bradycardia, hypotension, bronchospasm, etc.) was recorded perioperatively.
4 Discussion
In this study, we compared between the use of oral ivabradine to oral propranolol in patients undergoing laryngoscopic surgeries under general anesthesia to evaluate the efficacy of both drugs in attenuating the rise in blood pressure and heart rate occurring after laryngoscopy and intubation and to check whether they have an effect on blood glucose level perioperatively.
Stress response is a neuroendocrine complex occurring due to anesthesia and surgery. Even with stable anesthesia, laryngoscopy alone without intubation can cause a supraglottic stimulus. This stimulus leads to an increase in BP which is due to norepinephrine, and increase in HR which is due to epinephrine discharge. Placing the endotracheal tube can cause an infraglottic stimulus. In this situation, an extra cardiovascular response and catecholamine discharge occur. Stress response increases at this stage and both SBP and DBP in addition to HR measurements increase by up to 36–40% in contrast to control levels and hyperglycemia can be a feature of this response [Citation11,Citation12]. Bessey et al. [Citation13] have suggested that increased circulating concentrations of catecholamines, glucagon, and cortisol can evoke the changes in carbohydrate metabolism, occurring immediately after trauma.
In microlaryngoscopic surgery, these responses are more intense than in laryngoscopy for endotracheal intubation because the laryngoscope is introduced into the upper airways for 15–20 min compared to 15–30 s in tracheal intubation [Citation2].
Tachycardia along with hypertension increases ischemia risk in patients with coronary artery disease. The increase in the plasma concentration of catecholamines may provoke myocardial ischemia and cerebral hemorrhage [Citation8].
As controlling stress response is so important to the anesthesiologist, many strategies to circumvent this pressor response were tried such as minimizing the duration of laryngoscopy, IV narcotics, topical lidocaine, vasodilators, beta-blockers, oral gabapentin, oral clonidine and calcium channel blockers [Citation2,Citation3,Citation11,Citation14].
Also some studies were performed in microlaryngeal surgeries specifically, for example, Bharti et al. [Citation15] compared the hemodynamic changes and emergence characteristics of sevoflurane versus propofol anesthesia for microlaryngeal surgery. They found that sevoflurane was better than propofol in intraoperative cardiovascular stability without increasing recovery time. Boussofara et al. [Citation2] evaluated the effect of esmolol on cardiovascular changes during microlaryngeal surgery. They showed that the infusion of esmolol can prevent cardiovascular changes after microlaryngeal surgery. Ayatollahi et al. [Citation16] showed that 800 mg gabapentin 90 min before the microlaryngoscopy can attenuate increasing diastolic blood pressure and mean arterial blood pressure in the first 15 min after this procedure, but has no effect on systolic blood pressure or heart rate.
Propranolol is non-selective ß blocker. ß1 effect decreases heart rate and ß2 effect on skeletal muscle vascular bed may help in decreasing after load of heart. It may cause bradycardia, AV dissociation and hypoglycemia. Bronchospasm, congestive heart failure and drowsiness can occur even with low doses. Propranolol can be given orally and intravenously [Citation17].
Some studies evaluated the efficacy of beta-blockers including propranolol in decreasing stress response due to laryngoscopy [Citation18–Citation21].
Maharjan [Citation21] showed that 1 mg propranolol i.v. is superior to 0.5 mg in controlling hemodynamics after laryngoscopy and intubation without significant bradycardia in postoperative period.
Ivabradine is a relatively new HR lowering agent that not only decreases myocardial oxygen demand as assessed by the rate pressure product, to the same extent as propranolol, but also acts without any evidence of a depressant effect on cardiac function [Citation22]. If is thought to be one of the most important currents in pacemaking in the sino-atrial node [Citation23]. Animal studies indicate that ivabradine is a selective and specific inhibitor of If, and has few effects other than to slow the rate of diastolic depolarization and hence reduces HR. This specificity may explain the absence of significant negative inotropic actions of ivabradine observed in entire animal studies [Citation24–Citation26].
Ivabradine has been very useful in controlling the hemodynamics particularly the heart rate in all types of patients especially in patients where beta blockers are contraindicated such as asthmatics and diabetics. It can be given orally and intravenously [Citation22].
Some studies were done to evaluate the effectiveness of ivabradine in cardiac patients. Fox et al. [Citation27] showed that in coronary patients with a heart rate more than 70 bpm, ivabradine significantly reduces the risk of myocardial infarction by 36%.
In a study done by Swedberg et al. [Citation28] administration of ivabradine to heart failure patients significantly reduced the risk of death from heart failure and hospitalization for heart failure by 26%.
Raghuram et al. [Citation29] evaluated the efficacy of oral ivabradine to attenuate the hemodynamic responses after intubation. They found that ivabradine is an extremely useful drug to prevent abnormal increase in heart rate and blood pressure to a lesser extent seen during laryngoscopy and endotracheal intubation and recommended its routine use in all patients at risk for hypertension and tachycardia during laryngoscopy and endotracheal intubation.
The oral forms of propranolol and ivabradine are well tolerated, rapidly and completely absorbed from the gastrointestinal tract. The onset of action of the oral forms is within 20–30 min, with peak plasma concentration attained within 60–90 min [Citation28,Citation30].
Therefore we preferred to use the oral forms to benefit from their possible effects as preanesthetic medications. The doses given to the patients were the lowest starting doses as guided by the manufacturing pharmaceutical companies.
In our study, blood pressure and heart rate responses to laryngoscopy, intubation, fixation of laryngoscope and extubation were studied in both groups. Although there were mild increases in blood pressure and heart rate values in both groups after each stage, both ivabradine and propranolol provided a good general hemodynamic stability. However, ivabradine was more effective than propranolol with less changes in blood pressure and heart rate values.
Random blood sugar values were compared between the 2 groups perioperatively, and the preinduction values were slightly lower than baseline values which was due to fasting (around 8 h preoperatively). Both drugs didn’t show any significant effect on perioperative blood glucose level. We didn’t notice any possible side effects of either drugs as none of the patients complained of bradycardia, hypotension nor bronchospasm (a common side effect of propranolol).
The limitation of this study is that hemodynamics and blood glucose levels are not the only variables in the stress response as many hormones can be affected such as catecholamines, glucagon and cortisone.
In conclusion, both ivabradine and propranolol provide a good degree of hemodynamic stability in microlaryngoscopic surgeries but using ivabradine is more effective in addition to the avoidance of some side effects of beta blockers and the ability to be used in patients intolerant to beta-blockers. However, in our study, both drugs didn’t show any obvious effect in blood glucose level.
Conflict of interest
No conflict of interests.
Source of funding
No funding.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- F.G.DikkersA.M.SulterSuspension microlaryngoscopic surgery and indirect microlaryngostroboscopic surgery for benign lesions of the vocal foldsJ Laryngol Otol108199410641067
- M.BoussofaraD.BracoC.KaddourControl of haemodynamic variations secondary to suspension microlaryngoscopyTunis Med792001503507
- S.M.MarashiM.H.GhafariA.SaliminiaAttenuation of haemodynamic responses following laryngoscopy and tracheal intubation—comparative assessment of clonidine and gabapentin premedicationMiddle East J Anesthesiol202009233237
- G.BhandariK.ShahiEffect of gabapentin on pressor response to laryngoscopy and tracheal intubation: a double blind randomized placebo controlled studyPeople’s J Sci Res6201316
- T.SchrickerR.LattermannM.SchreiberW.GeisserM.GeorieffP.RadermacherThe hyperglycemic response to surgery: pathophysiology, clinical implications and modulation by the anesthetic techniqueClin Intensive Care91998118128
- H.KehletManipulation of the metabolic response in clinical practiceWorld J Surg242000690695
- H.F.GalleyM.A.DiMatteoN.R.WebsterImmunomodulation by anesthetic, sedative and analgesic agents: does it matter?Intensive Care Med262000267274
- A.Ashgan RaoufGohary M.ElH.Salah El-din AshmawiH.M.El-KerdawyH.H.EssaEfficacy of preoperative oral gabapentin in attenuation of neuro-endocrine response to laryngoscopy and endotracheal intubationJ Med Sci920092429
- J.S.BorerJ.C.TardifEfficacy of ivabradine, a selective I (f) inhibitor, in patients with chronic stable angina pectoris and diabetes mellitusAm J Cardiol10520102935
- S.N.MuratS.OrcanR.AkdemirArrhythmic effects of ivabradine in patients with coronary artery diseaseClin Invest Med322009322326
- A.L.KovacControlling the hemodynamic response to laryngoscopy and endotracheal intubationJ Clin Anesth819966379
- C.Prys-RobertsL.T.GreeneR.MelocheP.FoexStudies of anaesthesia in relation to hypertension. II. Haemodynamic consequences of induction and endotracheal intubationBr J Anaesth801998106122
- P.Q.BesseyJ.M.WattersT.T.AokiCombined hormonal infusion simulates the metabolic response to injuryAnn Surg2001984264281
- O.EbertJ.O.PearsonB.GelmanCirculatory responses to laryngoscopy the comparative effects of placebo, fentanyl and esmololCan J Anaesth361989301306
- N.BhartiP.ChariP.KumarEffect of sevoflurane versus propofol-based anesthesia on the haemodynamic response and recovery characteristics in patients undergoing microlaryngeal surgerySaudi J Anaesth62012380384
- VidaAyatollahiParvaneMirshamsiShekoufehBehdadMehdiAmirdosaraSedigheVaziribozorgEffect of oral gabapentin on haemodynamic variables during microlaryngoscopic surgeryAnaesth Intensive Therapy46120141722
- G.JonssonC.G.RegardhClinical Pharmacokinetice of ß-adrenoreceptor blocking drugsClin Pharm11976233263
- A.RathoreH.K.GuptaG.L.TanwarH.RehmanAttenuation of the pressure response to laryngoscopy and endotracheal intubation with different doses of esmololIndian J Anaesth4662002449452
- S.P.SinghA.QuadirP.MalhotraComparison of esmolol and labetalol, in low doses, for attenuation of sympathomimetic response to laryngoscopy and intubationSaudi J Anaesth432010163168
- P.DassM.GulabaniB.V.PatilS.H.VardhamaneComparative assessment of efficacy of lignocaine (1.5 mg/kg), esmolol (300 μg/kg), and dexmedetomidine (0.5 μg/kg) in minimizing the pressor response to laryngoscopy and intubationInt J Basic Clin Pharmacol422015306311
- S.K.MaharjanPropranolol is effective in decreasing stress response due to airway manipulation and CO2 pneumoperitoneum in patients undergoing laparoscopic cholecystectomyKathmandu Univ Med J3102005102106 2
- P.MulderS.BarbierA.ChagraouiV.RichardJ.P.HenryF.LallemandS.RenetG.LereboursF.Mahlberg-GaudinC.ThuillezLong-term heart rate reduction induced by the selective if current inhibitor ivabradine improves left ventricular function and intrinsic myocardial structure in congestive heart failureCirculation109200416741679
- D.Di FrancescoThe contribution of the ‘pacemaker’ current (If) to generation of spontaneous activity in rabbit sino-atrial node myocytesJ Physiol43419912340
- L.SimonB.GhalehL.PuybassetJ.-F.GiudicelliA.BerdeauxCoronary and hemodynamic effects of S 16257, a new bradycardic agent, in resting and exercising conscious dogsJ Pharmacol Exp Ther2751995659666
- P.BoisJ.BescondB.RenaudonJ.LenfantMode of action of bradycardic agent, S 16257, on ionic currents of rabbit sinoatrial node cellsBr J Pharmacol118199610511057
- C.ThollonC.CambarratJ.VianJ.F.ProstJ.L.PeglionJ.P.VilaineElectrophysiological effects of S 16257, a novel sino-atrial node modulator, on rabbit and guinea-pig cardiac preparations: comparison with UL-FS 49Br J Pharmacol11219943742
- K.FoxI.FordP.G.StegIvabradine for patients with stable coronary artery disease and left ventricular dysfunction: a randomized, double-blind, placebo-controlled trialLancet3722008807816
- K.SwedbergM.KomajdaM.BohnIvabradine and outcomes in chronic heart failure (SHIFT): a randomized placebo-controlled studyLancet3762010875885
- C.G.RaghuramDeeprajSinghAditya VikramKabraAttenuation of haemodynamic response to laryngoscopy and endotracheal intubation using intra-oral ivabradine: a clinical studyJ Evol Med Dental Sci33920149944995510.14260/jemds/2014/3289 August 28
- B.ApipanD.RummasakEfficacy and safety of oral propranolol premedication to reduce reflex tachycardia during hypotensive anesthesia with sodium nitroprusside in orthognathic surgery: a double-blind randomized clinical trialJ Oral Maxillofac Surg682010120124