Abstract
Airway management in patients with severe post burn mentosternal contracture is always a challenge for the anaesthesiologist. Difficulty in intubation occurs due to contracture and fixed flexion deformity of the neck resulting in nonalignment of oropharyngeal and laryngeal axis. We are reporting a case with severe postburn mentosternal contracture in whom endotracheal intubation was done successfully by using a Pro seal Laryngeal Mask Airway without its introducer along with a tube exchanger after a failed awake fibreoptic intubation.
1 Introduction
Difficult airway due to postburn stern mental contractures with limited head and neck mobility are considered to increase the risk during anaesthesia [Citation1]. Anaesthesiologist must plan strategies to prevent these a critical incidents during such airway management.
We report a case of successful endotracheal intubation by innovative use of Proseal Laryngeal Airway (PLMA) with tube exchanger after failed fibreoptic bronchoscope (FOB) attempt for contracture release.
2 Case report
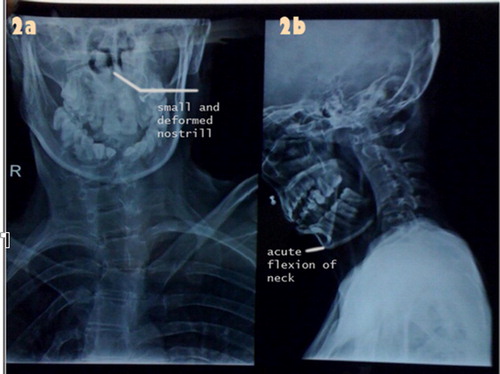
A 20-yr-old woman weighing 35 kgs, American Society of Anaesthesiologists (ASA) Class I with severe orofacial, neck and trunk burns presented to us for release of contracture and split skin grafting. Her medical history was unremarkable other than history of chemical burns one year back. The contracture included thick scar in the anterior neck and lower part of the face up to the angle of the mouth bilaterally with fixed flexion deformity (). The lower lip was totally everted to the extent that it merged with the anterior chest. The nostrils were stretched and narrowed but patent. Mouth opening was just more than one finger width with both the angle of mouth were stretched down. Mallampatti examination could not be done due to microstomia and fixed flexion deformity of neck. Assessment of stern mental and thyromental distance too was impossible because of distortion of neck anatomy. An X-ray neck showed an acute angulation in air shadow at the level of the glottis (). The trachea was not compressed or deviated. All routine blood investigations were normal.
Preoperatively, a difficult intubation was anticipated. Awake oral fiberoptic intubation was planned as first approach followed with an alternative back-up plan:
| (a) | Insertion of Proseal LMA and release of contracture. | ||||
| (b) | Release of the contracture and correction of the microstomia under tumescent anaesthesia, followed by direct laryngoscopy and intubation. | ||||
| (c) | Surgical airway. | ||||
In the preoperative room, an intravenous access was established. Inj Glycopyrrolate 0.2 mg, Inj Ranitidine 50 mg, and Odensetron 4 mg intravenously (IV) was given. The airway was prepared with 4% lidocaine nebulization and gargle and spray.
In operating room, after establishing monitoring, patient was premedicated with Inj. midazolam 1 mg and fentanyl 50 μg IV. An adult FOB with endotracheal tube #7 mm ID mounted on it, was introduced orally. It couldn’t be negotiated beyond vocal cords into the trachea despite the visualization of vocal cord on multiple trials. Next, insertion of Pro Seal LMA #2.5 was failed both in conventional and upside down position. Patient now became uncomfortable. She was reassured and Inj. Propofol 10 mg + ketamine in small aliquots was given. Oxygenation was maintained by nasopharyngeal airway. Proseal LMA #2.5 without its introducer in upside down position was reinserted and was placed successfully. Initially, introduction of the mask portion of the Proseal LMA was difficult and required some force to negotiate beyond the lower incisors because of reduced inter incisor gap and the problem in aligning the plane of the mask with the opening of the mouth (). This was overcome by the flexibility of Proseal LMA tube without its introducer. The correct placement of Proseal LMA was confirmed by capnography. Tube exchanger was introduced through the LMA under visualization of continuous end tidal CO2 trace. First attempt failed, later patient was put in slight right lateral position and possible to advance tube exchanger into trachea. Proseal LMA was than withdrawn over the tube exchanger and the trachea was then successfully intubated over tube exchanger by using armoured tube (6.5 mmID). Placement was confirmed by capnography. General anaesthesia was instituted using standard technique the remainder of the anaesthesia was uneventful.
3 Discussion
Severe post-burn contracture (PBC) of the neck puts the plastic surgeon as well as the anesthesiologist in a challenging situation. These patients may have restricted mouth opening, decreased oropharyngeal space, heavily fibrosed scars in the neck and limited atlanto-occipital joint extension, making not only very difficult to intubate but are also at high risk of failed ventilation via facemask [Citation2].
The principles of management of the potentially difficult airways as in this patient should include airway assessment, availability human and material resources, airway control by intubation, other contingency plan, monitoring and aftercare of the patients.
It is imperative that an airway assessment should be carried out preoperatively to evaluate the degree of difficulty and to plan strategies for alternatives. Assessment of the thyromental distance, the Mallampati score, and the mouth opening (interdental) distance, flexion–extension mobility of the head on neck can provide important data to anticipate difficult intubation [Citation3]. In our patient face and neck was extremely distorted making measurement of the airway parameters difficult.
Use of standard laryngoscope and intubation was not possible due to non alignment of oral/pharyngeal/laryngeal axis due to fixed flexion deformity. The choices recommended for such airway management include awake FOB intubation [Citation4], supraglottic devices [Citation5], pre-induction neck scar release under local anaesthesia or ketamine, elective tracheostomy or in some cases, discouragement of surgery altogether [Citation6].
Awake intubation is the safest option for patients with known difficult airway [Citation2,Citation7].
Surgeons were made standby for release of contracture under local anaesthesia or emergent tracheostomy.
We kept awake oral FOB guided intubation as our main approach for securing the airway as both the nostrils were narrowed, fibrosed and distorted.
In our patient, we failed to guide FOB beyond glottis opening despite visualization of vocal cord. Rakesh et al. [Citation8] failed to negotiate endotracheal tube over the FOB despite successful tracheal placement of FOB, probably acute bend at the junction of the laryngopharynx and glottic opening in patients with extreme neck flexion.
The supraglottic airway devices, such as the laryngeal mask airway (ILMA, PLMA) have proven to be very useful options as they not only establish the patent airway also maintain adequate ventilation when the facemask ventilation proves difficult or impossible [Citation4,Citation5].
We tried to insert Proseal LMA (PLMA) #2.5 in the conventional technique as well as upside position. A minimum distance between patient’s hard palate and anterior most part of chest/neck is required for it to be introduced. This distance is equal to the shortest distance between the tip of mask portion and its machine end. In a case like ours with fixed flexion deformity of neck, this distance was reduced and the machine end of PLMA could not be lowered enough to align the PLMA with hard palate. Kumar et al. successfully intubated using ILMA in upside down position [Citation8]. Use in upside side down position shifts the machine end of LMA from the chest towards front of patient’s nose, thus avoiding getting stuck at patient chest was beneficial. We failed to introduce PLMA in conventional or upside position when was mounted on introducer. Use of ILMA in fixed flexion deformity has met with success [Citation9] and failures [Citation10] by different authors.
Removing the introducer has been reported to increase the maneuverability, beneficial in patients with a stereotactic frame or a neck collar [Citation11]. After initial difficulty, Proseal LMA without the introducer was successful in establishing the airway in our case. Complications can occur with folding back of the mask, increasing the risk of regurgitation and aspiration but were not seen with our patient. Capnography has been useful in confirming correct placement of the LMA.
Use of the laryngeal mask for release of contracture and reconstruction may be hazardous for the associated anatomical abnormalities and airway maintenance may be jeopardized in operations which require turning of the patient [Citation12].
Thus securing an airway with endotracheal tube is a safer approach. Tracheal intubation through the Proseal LMA requires a long narrow tracheal tube or a tube exchanger [Citation13].
The passage of an orotracheal tube of 6 mm through the LMA size #3 and 4 has been recommended as a means of achieving tracheal intubation [Citation13]. However, this was not possible in this case as Proseal #2.5 was used. We thought of passing ET tube exchanger through Proseal LMA #2.5 under continuous end tidal CO2 tracing. In first attempt we failed when the patient was supine, probable reason being that the tube exchanger was getting coiled up or stuck anteriorly in the supraglottic area because of acute angulation of neck and later on turning the patient to right may have resulted in extension of neck and tube exchanger could slide across the vocal cords. Slight right lateral position has also been described to improve position of Proseal LMA [Citation14]. After successful placement of tube exchange, airway was successfully secured with passage cuffed ETT # 6.5 (armoured) without difficulty.
4 Conclusion
In patient with severe sterno mental postburn contractures, airway management by direct laryngoscopy and induction by conventional method may prove disastrous. Proper preoperative assessment and multiple contingency plan to secure airway is necessary for a positive outcome to handle such airway.
This case has demonstrated the use of Laryngeal Mask Airway (Proseal LMA without its introducer + tube exchanger) as an effective alternative for securing airway and intubation in patients of fixed flexion deformity even with limited mouth opening (⩽2 cm)and after failed FOB and PLMA in conventional way.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- PramodGuptaVandanaTalwarSumitVermaSaurabhMahajanAnoop RajGogiaModified mouth prop for orotracheal Fiberoptic intubationJ Anaesth Clin Pharmacol2220066568
- R.A.KaplanJ.L.BenumbedF.A.BerryR.H.BodeF.W.CheneyPractice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult AirwayAnesthesiology98200312691277
- SunandaGuptaRajeshSharmaDimpelJainAirway assessment: predictors of difficult airway assessmentIndian J Anaesth4942005257262
- J.V.DivatiaS.M.UpadhyeR.SareenFiberoptic intubation in cicatricial membranes of the pharynxAnaesthesia471992486489
- G.NathV.MajorThe laryngeal mask in the management of a difficult airwayAnaesth Intens Care41992518519
- P.AggarwalSafe method for release of severe post burn neck contracture under tumescent local anaesthesia and ketamineIndian J Plastic Surg37120045154
- S.M.LarsonD.H.ParksManaging the difficult airway in patients with burns of the head and neckJ Burn Care Rehabil919885556
- R.KumarPrashasA.WadhwaS.AkhtarThe upside down intubating laryngeal mask airway: a technique of cases of fixed flexed neck deformityAnesth Analg95200214541458
- T.AsaiK.ShinguTracheal intubation through the intubating laryngeal mask in a patient with affixed flexed neck and deviated larynxAnaesthesia534199811991208
- H.G.WakelingJ.NightingaleThe intubating laryngeal mask does not facilitate tracheal intubation in the presence of a neck collar in simulated traumaBr J Anaesth842000254256
- J.BrimacombeC.KellerThe Proseal laryngeal mask airwayAnesth Clin N Am202002871891
- M.KreulenD.MackieR.KreisF.GroeneveltSurgical release for intubation purposes in post-burn contracture of the neckBurns221996310312
- A.A.MatiocG.A.ArndtIntubation using the Proseal laryngeal mask airway and a Cook airway management airway catheter setCan J Anaesth482001932
- Y.MatsuoK.MurashimaT.SataIncidence of insertion difficulty using Proseal laryngeal mask airway and the efficacy of recommended insertion maneuversMasui5610200711681173

