Abstract
For superficial parotidectomy general anesthesia is ideal, but certain patients may be unfit. The present case had uncontrolled hypertension together with difficult airway. To avoid any suspected complications, we decided to do the operation under local anesthesia. We planned to block the maxillary nerve and superficial cervical plexus with greater auricular nerve together with incision site infiltration. A mixture of bupivacaine 0.25% and lignocaine 1% with adrenaline 1: 200,000 was prepared. The block was effective after about 15–20 min and the surgery was performed uneventfully using only the nerve blocks with mild sedation.
1 Introduction
The percentage of occurrence of primary parotid malignancies is about 1–3% of all head and neck malignancies. The surgical management is individualized due to wide variability in the clinical behavior and presentation and influenced by tumor location, histological grade, extent, and spread. The surgical management includes superficial parotidectomy, total conservative parotidectomy, and radical parotidectomy, palliative biopsy only, and neck dissection [Citation1].
One of the most common procedures of the parotid is superficial parotidectomy. General anesthesia is ideal but certain patients may be at risk or unfit for general anesthesia [Citation2].
A method of obtaining an effective anesthesia for such cases is nerve block. To effectively block the parotid area, the maxillary, superficial cervical including greater auricular nerve block and local skin infiltration were planned to be performed. A written consent had been obtained from the patient for the publication of this case report.
2 Case description
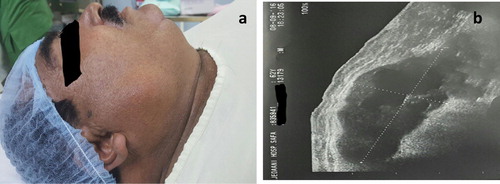
62 years old male complained from swelling just below angle of mandible right side which was gradually increasing for 6 months, with no relation with meals. The swelling was cystic in some and solid in other areas, non-tender, non-fluctuant, and partially mobile swelling. Stensen’s and Warthin’s duct openings were normal. Ultrasound examination revealed 2.3 × 5.3 × 3.4 cm well-defined lobulated margined soft tissue mass with cystic component and multiple tiny irregular sponge like anechoic areas.
Preoperative evaluation showed the following: 1- Obese patient weighed 130 kg with BMI of 47.8. 2- history of obstructive sleep apnea. 3- Poorly controlled chronic hypertensive (BP was 200/110 mmHg) on double antihypertensive medications (Calcium channel blocker and angiotensin converting enzyme inhibitor). 4- Poor R wave progression and left ventricular hypertrophy in ECG. 5- Airway evaluation revealed short neck, large tongue, Mallampati score of III, limited neck mobility and mentosternal distance of 9.5 cm.
All Laboratory investigations were within normal except mild elevation in serum creatinine (1.6 mg/dl).
The patient postponed twice for blood pressure control. On the day of surgery his BP was 160/100 mmHg.
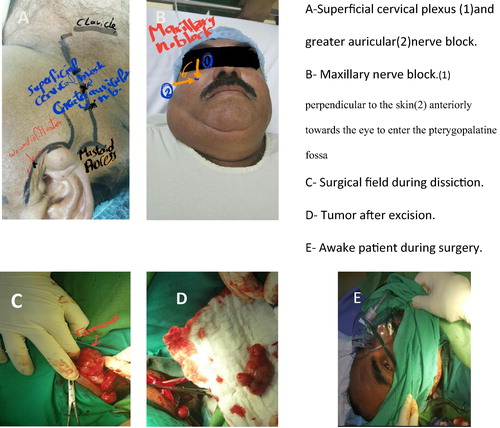
The increased risk for complications from a general anesthetic, gave rise to use local or regional anesthesia. We decided to perform maxillary, superficial cervical including greater auricular nerve block and local skin infiltration for excision biopsy of the parotid tumor, after a discussion with the patient and surgeon to avoid general anesthesia and complications related to hypertension and difficult airway (see ).
3 Operation technique
The surgery was done in a fully equipped operation theatre with full support of general anesthesia and all emergency resuscitation measures. A plan was made to manage the suspected difficult airway according to ASA guidelines. Different blade sizes, Mc Coy’s laryngoscope, fiberoptic, and an assistant anesthesiologist were all ready.
Premedication with midazolam 3 mg with 40 μg fentanyl and Ringers lactate 1000 ml. Patient was positioned with head turned to the opposite side on a headrest. An injection of bupivacaine 0.25% (2 mg/kg) and lignocaine 1% with adrenaline 1: 200,000 (7 mg/kg) was prepared.
The plan was to block the maxillary nerve and superficial cervical plexus with greater auricular nerve together with incision site infiltration. The posterior border of sternomastoid muscle was marked at the middle and at the junction of the upper and middle one-third ().
3.1 Superficial cervical plexus and Grater auricular nerve block
Technique
After cleaning the skin with povidine iodine solution, the needle was inserted at midpoint of posterior border of the sternomastoid, and behind it three injections of 5 mL of local anesthetic are injected subcutaneously, perpendicularly, cephalad, and caudal in a 'fan' fashion.
Then at the junction of the upper and middle one-third another three injections in three directions, first cephalad at the posterior border of sternomastoid muscle and then anterior and upwards superficial to it and then posterior and upward.
3.2 Maxillary nerve block (V2 block)
Technique: external approach
A needle was inserted just below the zygomatic arch midway between the coronoid and condyle of the mandible. It was inserted perpendicular to the skin until the pterygoid plate was felt (B (1)). The needle was then withdrawn and guided anteriorly towards the eye to enter the pterygopalatine fossa (B (2)). Five ccs of local were injected when paraesthesia of the upper jaw is elicited.
3.3 Wond site infiltration
Skin wound site infiltration of local anesthesia with 10 cc mixture of local anesthetic prepared before.
Onset of anesthesia occurred within 15–20 min. The facial nerve and its branches were saved. No other lymph nodes were identified during surgery. Superficial parotidectomy was done. The surgery was performed uneventfully using only the nerve blocks.
4 Discussion
Parotidectomy is generally indicated for histopathological diagnosis of a parotid mass. Parotid masses are generally benign, the incidence of which is around 2.4 per 100,000 [Citation3].
Factors determining the extent of surgery include tumor size and degree of local extension. Facial nerve and its peripheral branches are at risk during superficial parotidectomy surgery under GA. About 30–65% of patients suffer from transient facial nerve paralysis and 3–6% has permanent dysfunction of the facial nerve following total superficial parotidectomy [Citation4].
Preservation of facial nerve peripheral branches requires high surgical skills and it can be done by using nerve stimulator which is costlier and usually available at tertiary care hospitals. Local or regional anesthesia can be used to preserve facial nerve. Under LA, patient complaints of pain and discomfort if dissection involves facial nerve sheath or its peripheral branches thus helping in its identification and prevention of iatrogenic nerve injury [Citation1].
There have been a few reports of parotid surgeries under local anesthesia [Citation5–Citation7] using different techniques [Citation5–Citation7] with the use of a mixture of bupivacaine and lidocaine for local anesthesia [Citation8].
Bupivacaine is four times more potent than lidocaine and has a longer duration of action of 6 h. However, lidocaine has a faster onset of action within 3–5 min. Offering a mixture of both to the patient provides a quick onset with a larger duration of action, adequate for the surgery. Recently parotidectomy under LA has come in vogue [Citation8–Citation10].
Surgical anesthesia or supplemental pain control can be provided for any surgery involving the inferior portion of the external ear, the area overlying the mastoid process, procedures of the parotid gland, or procedures involving the angle of the mandible by blocking greater auricular nerve [Citation11].
We found that LA technique can be really helpful if patient is at risk during general anesthesia like in our case of uncontrolled high BP. It also had an advantage of avoiding airway manipulations in case of suspected difficult intubation as in our case. Smooth recovery postoperatively with less usage of narcotics and other drugs with less pain and complications leading to shorter hospital stay with early healing are added advantages.
Steckler [Citation12] had enumerated the advantages of a parotidectomy using local anesthesia:
| (1) | No muscle relaxants are required as the surgery is conducted in a relatively superficial plane. This allows for easy testing of the integrity of the facial nerve. | ||||
| (2) | Various manoeuvres for identifying the facial nerve, such as use of a nerve stimulator or injecting a dye into the parotid duct are rendered superfluous. | ||||
| (3) | Chances of drug overdose are minimised as not more than 20–25 ml of 0.5% of bupivacaine are required. | ||||
| (4) | The present-day concept of out-patient parotidectomy is promoted, as a procedure under local anesthesia facilitates early discharge. | ||||
The performed technique was different as none of previously described techniques used the combination of maxillary, superficial cervical with greater auricular nerve block together with wound site infiltration. I think that incision site infiltration and overlaps in sensory innervation between maxillary nerve from above with that of superficial cervical plexus and greater auricular nerve from below helped in dispensing the block of mandibular nerve.
5 Conclusion
Parotidectomy under LA is an effective alternative to general anesthesia that can be considered in patients who are at high risk during GA. It gives the advantage as patient is conscious and awake thus maintaining good airway. Discomfort if dissection is too near to the facial nerve help in protection of it from injury.
Conflicts of Interest
None.
Contribution
Anesthetist who performed the block.
Funding
Not funded.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- I.D.SinghJ.R.GalagaliHotaMaj AbhipsaA case series of superficial parotidectomy under local anesthesiaInt J Otorhinolaryngol Head Neck Surg1120152730
- K.S.SethnaM.A.SenguptaS.PrabhakarLocal anesthesia for parotidectomy – a new techniqueAmbul Surg419969394
- A.GunnN.R.ParrottParotid tumors: a review of parotid tumor surgery in the Northern Regional Health Authority of the United Kingdom 1978–1982Br J Surg75198811441146
- C.J.KerawlaN.McAloneyL.F.StassenProspective randomized trial of the benefits of a sternocleidomastoid flap after superficial parotidectomyBr J Oral Maxillofac Surg402002468472
- T.FujimuraY.YonemuraT.KamataS.TakegawaK.SugiyamaG.NishimuraA case of parotid tumor showing remarkable regression following hyperthermo-chemo-radiotherapyGan To Kagaku Ryoho141987723727
- K.S.SethnaM.A.SenguptaS.PrabhakarLocal anesthesia for parotidectomy: a new techniqueAmbul Surg419969394
- P.H.ReeceM.E.PapeschN.S.TolleySuperficial parotidectomy under local anesthesiaJ Laryngol Otol1142000983984
- K.ShahidB.K.SiddiquiM.H.TahirAyubSalman binG.M.MemonA.YousufTotal parotidectomy under local anesthesia: a novel techniqueJ Coll Physicians Surg Pak1722007 Feb116117
- T.L.ChowC.Y.ChoiS.H.LamParotidectomy under local anesthesia - report of 7 casesAm J Otolaryngol34120137981
- M.SafioleasM.StamatakosP.SafioleasA.DiabR.IannescuC.SafioleasSuperficial parotidectomy under local anaesthesiaChirurgia10342008453454
- Michael K.RitchieColin A.WilsonBrian W.GrosePavithraRanganathanStephen M.HowellMatthew B.EllisonUltrasound-Guided Greater Auricular Nerve Block as Sole Anesthetic for Ear Surgery. Clin Pract.622016856
- R.M.StecklerOutpatient parotidectomyAm J Surg1621991303305