Abstract
Background
The main goal of this review article is to elucidate the merits as well as the safety of nalbuphine as an adjunct to local anesthetics in the sub-arachnoid block, so that its usage will increase considerably. Unlike morphine and fentanyl, nalbuphine, a mixed agonist-antagonist opioid, is not commonly used despite its better features such as good duration of analgesia, lack of pruritus, lesser respiratory depression, nausea and vomiting. There is no review article available in the literature that had analyzed “intrathecal nalbuphine” specifically. The other types of literature available also very few.
Methods
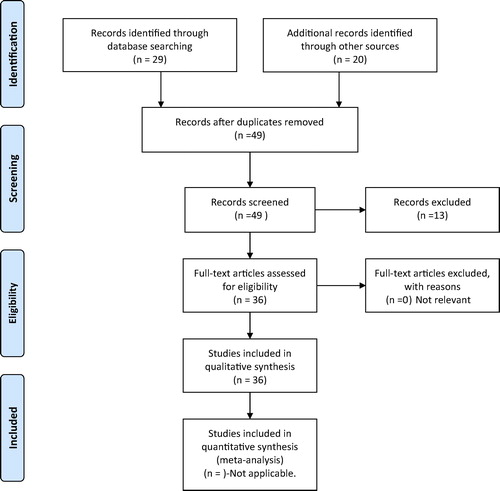
This review article is based on few available literatures that had studied the effects of intrathecal nalbuphine. Total results from PubMed search of “intrathecal nalbuphine” was 29 as on 05 March 2017. Thirteen articles were removed from these 29, as they were not relevant to this topic. Nine more articles were taken from PubMed following an additional search of “similar articles” to support this article further. Two articles were selected from Google and seven articles from Embase indexed journals were collected after initial search from Google. Two review articles were collected from Cochrane database, although not specific to intrathecal route of administration alone.
Conclusion
Nalbuphine is a very useful adjunct to intrathecal local anesthetics because of the good duration of analgesia, anti-pruritic,anti-shivering properties, lesser respiratory depression, nausea, and vomiting. The author hopes that this review article will be a forerunner for many more studies to come in the future, so that its acceptance will become widespread.
Keywords:
1 Introduction
Sub-arachnoid block is a very common and popular technique in the day-to-day practice among anesthesiologists. Various local anesthetics are available with different durations of action and different degrees of safety. The use of opioids in sub-arachnoid block has been in clinical practice since 1979 [Citation1]. Since then, the usage of opioids as adjuvant in sub-arachnoid block had gained momentum and it is a very common practice to use opioids as adjuncts to local anesthetics even today. Various opioids have been used along with local anesthetics or as sole agents [Citation2]. The administration of opioids in intrathecal space as an adjuvant to local anesthetic was found to provide very good analgesia in various surgical procedures [Citation3,Citation4]. The scientific explanation behind the combination of opioids and local anesthetics intrathecally is, that these two drugs act at different sites and hence provide better analgesia than administration of individual drug alone. The local anesthetics produce its effects by acting at nerve axon and opioids at their receptors in the spinal cord. This combination also provides better hemodynamics and lesser side effects than if they were administered alone. The pure mu agonists such as morphine and fentanyl are commonly used in the central neuro-axis blocks. Respiratory depression, pruritus, nausea and vomiting are the common adverse effects associated with these pure mu agonists. Nalbuphine is an opioid with agonist actions in the kappa receptor and antagonist actions in the mu receptor [Citation5,Citation6]. Because of this mixed agonist-antagonist effects, it produces analgesia and sedation through agonism at the kappa receptor and lesser side effects through antagonism at the mu receptor [Citation7]. Hence, intrathecal nalbuphine produces lesser adverse effects like pruritus, nausea and vomiting when compared to intrathecal morphine [Citation8]. Intrathecal nalbuphine does not cause any significant hemodynamic or respiratory complications [Citation9]. Nalbuphine does not cause addiction because of its mu antagonist effects. Therefore, the use of nalbuphine does not require license unlike the pure mu agonists such as morphine, fentanyl etc, which is an additional advantage.
Despite these good qualities, the usage of nalbuphine as an additive to intrathecal local anesthetics is not widespread. In our geo-graphical area also, it is not commonly used. Even the literature search gives only very few results when compared to other opioids administered intrathecally. This review article is based on few available literatures in PubMed, Embase, Cochrane database and Google that had studied the effects of intrathecal nalbuphine as an adjuvant to local anesthetics in different populations. A total of 36 articles were taken after carefully analyzing their relevance and strength to this topic. This article covers the history, safety in different populations, optimum dose of intrathecal nalbuphine as well as nalbuphine usage through different routes of administration.
2 Historical perspective
The first reported literature in PubMed as far as intrathecal nalbuphine is concerned is that of Schmauss C et al. [Citation10]. They found that both intrathecal nalbuphine as well as morphine had inhibited the writhing evoked by intra-peritoneal acetic acid administration. This was an animal study published in the year 1982. They also observed that combination of nalbuphine and morphine resulted in maximum inhibition of writhing with lower doses of both drugs than if they were administered alone. Another study by Schmauss C et al. [Citation11], published subsequently in 1984 had further elucidated the different receptors for opioid effects. This was also an animal study, that tested the effects of various opioids following intrathecal administration. This study observed that intrathecal administration of mu, delta agonists produced dose-dependent inhibition of cutaneous thermal responses. Nalbuphine and buprenorphine, which are partial agonists, also produced the same effects, whereas the pure kappa agonists did not. Another important observation of this study was reduction of visceral pain with mu and kappa agonists but not with delta agonists. The findings of this study would have probably led to the better understanding of the various opioid receptors and its effects, resulting in widespread usage of them clinically, with the exception of nalbuphine. Of course, there were previous studies that had analyzed the effects of intrathecal morphine but not nalbuphine. For historical interest, I would like to mention three previous studies that had tested intrathecal morphine. One published in 1977, was an animal study [Citation12]. The other two studies, involving the human population, were published subsequently in 1979 [Citation1], and in1980 [Citation13].
3 How safe is “intrathecal nalbuphine”?
Rawal et al. had studied the behavioral, motor, electroenchelographic and histopathologic changes following intrathecal administration of large and small doses of butorphanol, sufentanil and nalbuphine in sheep [Citation14]. The opioids were given at every six hours for three days while the control group received intrathecal saline. They observed that butarphanol regardless of the dose and sufentanil in large doses had produced many behavioral changes such as agitation, rigidity and motor paralysis of the hind limbs. They also observed increased seizure activity in the electroencephalogram as well as histopathological changes in these groups. The changes observed in intrathecal nalbuphine group were similar to that of the control group that received saline implying that intrathecal nalbuphine was devoid of neurotoxic effects. This animal study published in 1991, had ensured the safety of intrathecal nalbuphine.
Subsequent study involving human population undertaken by Lin ML, published in 1992, had proved that intrathecal nalbuphine produced lesser side effects than intrathecal morphine [Citation15]. This study had compared nalbuphine 0.4 mg vs morphine 0.4 mg as an additive to intrathecal tetracaine and observed that both provided prolonged duration of analgesia than the control group, but, lesser side effects in the nalbuphine group.
The recent study by Gupta K et al. has also confirmed that intrathecal administration of nalbuphine does not cause significant side effects even at the dose of 2 mg [Citation16]. They had done the comparative study of 2 mg of nalbuphine vs 25 microgram of fentanyl as an adjunct to 3.5 ml of 0.5% bupivacaine intrathecally and concluded that nalbuphine had provided prolonged analgesia as well as motor block without any adverse effect.
3.1 Safety of intrathecal nabuphine in pregnant population
Culebras X et al. [Citation8] had compared the effects of intrathecal morphine 0.2 mg vs different doses of intrathecal nalbuphine [0.4 mg, 0.8 mg and 1.6 mg] as an adjunct to 10 mg of hyperbaric bupivacaine 0.5% in elective cesarean section patients and found that intrathecal morphine not only provided longest duration of analgesia but also produced significant side-effects like pruritus, nausea and vomiting. They also observed that among the nalbuphine groups, 0.8 mg provided good intraoperative and early post-operative analgesia without much side-effects. There was no maternal respiratory depression and the neonatal APGAR scores, arterial blood gas values were also not affected in all groups of patients. This study was published in the year 2000.
Subsequent study by Yoon et al. [Citation17], published in 2002, had compared the effects of intrathecal morphine 0.1 mg (group M), nalbuphine 1 mg (group N) and a combination of morphine 0.1 mg plus nalbuphine 1 mg (group M + N) as an additive to 0.5% bupivacaine 10 mg in 60 patients undergoing cesarean section. They concluded that the duration of effective analgesia was longer in the group M as well as in the group M + N than in the group N. The incidence of pruritus was significantly lower in the group N compared to other two groups, whereas the incidence of nausea and vomiting did not show any significant difference between groups.
Another study published in 2014 by Gomaa et al. [Citation18], also concluded that intrathecal nalbuphine produced lesser side-effects such as pruritus, nausea and vomiting compared to intrathecal fentanyl in cesarean section patients although it was statistically insignificant. They had compared intrathecal nalbuphine 0.8 mg vs fentanyl 25 microgram as an adjunct to 2 ml of 0.5% bupivacaine in elective cesarean section patients and observed no significant difference with regard to onset of sensory block. Duration of sensory and motor block, were also insignificant between the two groups. The onset of complete motor block was significantly faster in the fentanyl group, probably due to its high lipid solubility, as opined by the authors. Although statistically insignificant, the duration of post-operative analgesia was longer in the nalbuphine group. The adverse effects were also lesser in nalbuphine group, though statistically not significant.
Only these few studies are available in PubMed and Embase, that had analyzed the effects of intrathecal nalbuphine in cesarean section patients. However, there are other studies that had analyzed the effects of intravenous nalbuphine either alone in various doses [Citation19] or in comparison with other drugs such as diphenhydramine [Citation20], propofol [Citation21] or ondansetron [Citation22,Citation23] in reducing the incidences of pruritus following intrathecal morphine in cesarean section patients. Intravenous nalbuphine in the dose of 2 to 3 mg was optimum, without increasing the pain or producing other unwanted effects [Citation19]. Intravenous nalbuphine was more effective than diphenhydramine [Citation20] and propofol [Citation21]. Intravenous nalbuphine as well as ondansetron were more effective than placebo [Citation22,Citation23]. Nalbuphine is better than ondansetron as it is not excreted in the breast milk [Citation23].
3.2 Safety of intrathecal nabuphine in geriatric population
Fournier R et al. [Citation24] had conducted a study on geriatric patients undergoing total hip replacement under continuous spinal anesthesia comparing nalbuphine 0.4 mg vs morphine 0.16 mg. They concluded that intrathecal nalbuphine produced significant quicker onset of pain relief as well as shorter duration of action compared to morphine, which is beneficial in this study population. This study ensured the safety of nalbuphine over morphine. This study, published in the year 2000, was the first study as far as geriatric patients are concerned.
Another study by Sapate M et al. [Citation25], had also observed that intrathecal nalbuphine was safe and effective in providing post operative analgesia in patients aged between 50 and 70 years. They used 3 ml of 0.5% hyperbaric bupivacaine with 0.5 mg of nalbuphine as a single dose.
Moustafa et al. [Citation26] also studied the effects of intrathecal nalbuphine in patients undergoing total knee arthroplasty who were aged between 50 and 70 years. In this study, one group of patients received intrathecal bupivacaine 0.5% 3 ml with 0.2 mg morphine while the other group received intrathecal bupivacaine 0.5% 3 ml plus 0.2 mg morphine and nalbuphine 1 mg as an additional opioid intrathecally. This study observed that intrathecal nalbuphine as an additive to bupivacaine plus morphine, had produced lesser side effects such as pruritus and vomiting without affecting the duration of analgesia.
3.3 Safety of nabuphine in pediatric population
To date, there is no study available that has analyzed the effects of intrathecal nalbuphine in children. However, few studies are available that had tested the effects of intravenous administration of nalbuphine in pediatric patients. The one published in 2010 by Schmitz A et al. [Citation27], had tested the effects of intravenous infusion of nalbuphine as an adjuvant to intrathecal morphine or sufentanil in severely handicapped children undergoing spine surgeries and concluded that nalbuphine infusion was very effective in 93% of children, resulting in early extubation. Other two studies had concluded that intrathecal morphine was better than intravenous nalbuphine patient controlled analgesia in thoracic or abdominal operations in children [Citation28] or intermittent on-demand intravenous nalbuphine in children who had undergone frontal encephelocle operations [Citation29].
It is quite heartening to note that nalbuphine has been used as an adjuvant in caudal anesthesia in children recently [Citation30,Citation31]. These two studies published in the year 2016, had concluded that caudal nalbuphine as an adjuvant to levo bupivacaine had not only prolonged the postoperative analgesia significantly, but safe as well [Citation30,Citation31]. One study had tested nalbuphine 0.1 mg per kg with 1 ml per kg of levo bupivacaine 0.25% [Citation30], whereas, another study had tested nalbuphine 0.2 mg per kg with 1 ml per kg of levo bupivacaine 0.125% [Citation31].
4 What is the optimum dose of intrathecal nalbuphine?
As already mentioned, Culebras X et al. [Citation8] had observed that intrathecal nalbuphine 0.8 mg provided good intraoperative and early post-operative analgesia without much side-effects in cesarean section patients after comparing it with various doses as well as with morphine. Gomaa et al. [Citation18] had also observed lesser side effects with the same amount of nalbuphine i.e. 0.8 mg with the same amount of local anesthetic bupivacaine [10 mg] in cesarean section patients. However, another study by Mukherjee et al. [Citation32] had observed that 0.4 mg of nalbuphine was effective in providing good post-operative analgesia without side effects compared to 0.8 mg of nalbuphine. However, they had used 2.5 ml of the local anesthetic 0.5% hyperbaric bupivacaine and in the different population. The assurance that we get from the studies of Culebras et al. [Citation8] and Gomaa et al. [Citation18] is, “intrathecal nalbuphine” is safe at the dose of 0.8 mg even in pregnant patients. Indeed, it is safe even up to the dose of 1 mg that too with morphine 0.1 mg in cesarean section patients according to a study by Yoon et al. [Citation17]. Mukherjee et al. had observed that 0.8 mg of nalbuphine had produced the longest duration of analgesia but with significant side effects in the postoperative period like hypotension and bradycardia, although none of their patients had respiratory depression [Citation32].
Tiwari AK et al. [Citation9] had used 2.5 ml of 0.5% hyperbaric bupivacaine with 0.2 or 0.4 mg of nalbuphine in adult patients. Sapate M et al. [Citation25] had used the 3 ml of 0.5% hyperbaric bupivacaine with 0.5 mg of nalbuphine in elderly patients and observed that it was safe and effective.
Jyothi B et al. had observed that the intrathecal dose of 0.8 mg of nalbuphine as an additive to 15 mg of bupivacaine was optimum in providing long lasting quality analgesia and safe, compared to 1.6 mg or 2.5 mg [Citation33]. As previously stated, according to the recent study by Gupta K et al., intrathecal administration of nalbuphine is safe even at the dose of 2 mg in adult patients [Citation16].
After analyzing these studies, this author opines that intrathecal nalbuphine in the dose of 0.4 mg to 0.8 mg will be acceptable as an adjuvant to local anesthetic like 0.5% bupivacaine 2.5 ml to 3 ml in adult patients. Because of the ceiling effect, it is not going to be useful if the dose of nalbuphine is higher than 0.8 mg. The dose of local anesthetic can be 1.8 to 2 ml with nalbuphine 0.4 mg in cesarean section patients. The dose of local anesthetic can be 2.5 ml to 3 ml with nalbuphine 0.4 mg in elderly patients. The author recommends further randomized, controlled studies after pilot study to know the optimum dose of intrathecal nalbuphine. Of course, it is difficult to determine the optimum dose because of different geo-graphical areas, patient populations, properties of local anesthetic, nature of surgical procedures etc. Nevertheless, we can further ensure the safe margin of the dose of intrathecal nalbuphine in various study populations.
5 Role of intrathecal nalbuphine in reducing shivering
Shivering during spinal anesthesia is a common problem which is not only discomfort for the patient but poses difficulties for the anesthesiologist as well, because it causes disturbances in monitors, increases oxygen consumption and carbon dioxide production. Recent study has concluded that intrathecal nalbuphine 0.4 mg as an adjuvant to bupivacaine is significantly reducing the incidence of shivering during knee arthroscopy under spinal anesthesia [Citation34].
6 Review articles on various routes of nalbuphine administration
Although there is no review article available that is specific to “intrathecal nalbuphine”, two recent review articles on nalbuphine are worth mentioning here [Citation35,Citation36].
One review article by Jannuzzi RG [Citation35], published in 2016, had analyzed nine randomized controlled trials and one case report and observed that the incidence of pruritus was more in the neuraxial administration of opioids than through intravenous administration. This study concluded that nalbuphine was more efficient in providing relief to opioid induced pruritus than placebo, diphenhydramine, naloxone and propofol. It also observed that low dose intravenous nalbuphine (2.5 to 5 mg) did not cause attenuation of analgesia or excess sedation compared to 10 mg of nalbuphine. The additional observation was that nalbuphine caused reduction of nausea and vomiting and reversal of respiratory depression as well. This study has recommended that nalbuphine should be used as first choice in opioid induced pruritus.
Another review article by Zheng Zeng et al. [Citation36] published in 2015, was a meta-analysis of various studies that had compared the efficacy of morphine vs nalbuphine in different routes of administration such as intramuscular, intravenous, intrathecal and epidural. They concluded that nalbuphine has analgesic efficacy that is comparable to morphine, but nalbuphine is safer than morphine with regard to adverse effects such as pruritus and respiratory depression.
7 Scope of intrathecal nalbuphine in future
The author hopes that many studies will be undertaken on “intrathecal nalbuphine”, because of its safety and better features. More so, as an adjuvant to newer intrathecal local anesthetics such as levo bupivacaine and ropivacaine that have gained popularity in this century because they are also safer. The author also hopes that many studies are possible on caudal nalbuphine in children, based on the few literature, published in the year 2016 [Citation30,Citation31].
8 Summary
| 1. | Only few studies are available with regard to intrathecal nalbuphine, although its safety and advantages over other opioids had been ensured about three decades ago involving animals as well as human population. | ||||
| 2. | No study is available as far as pediatric patients are concerned with regard to intrathecal nalbuphine. However, very few studies are available that had tested the effects of caudal nalbuphine in children. | ||||
| 3. | No study is available which had used intrathecal nalbuphine as an adjuvant to newer local anesthetics such as levo bupivacaine and ropivacaine. | ||||
9 Conclusion
Paucity of literature may be considered as an indirect evidence that nalbuphine is not commonly used, especially in intrathecal route as an adjuvant, despite its better features such as anti-pruritic, anti-shivering, lesser respiratory depression, nausea and vomiting. Hence, it is high time that usage of nalbuphine as an adjunct in sub-arachnoid block should increase a lot, particularly with newer local anesthetics such as ropivacaine and levo-bupivacaine, to extend the duration of analgesia. The author eagerly expects many studies on this topic, which will certainly result in its widespread acceptance, and hopes that this review article will be a forerunner for the same.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- J.K.WangL.A.NaussJ.E.ThomasPain relief by intrathecally applied morphine in manAnesthesiology501979149151 PMID:373503
- M.MorganThe rational use of intrathecal and extradural opioidsBr J Anaesth631989165188
- M.WilwerthJ.L.MajcherP.Van der LindenSpinal fentanyl vs. sufentanil for post-operative analgesia after C-section: a double-blinded randomised trialActa Anaesthesiol Scand609201613061313
- S.ChakrabortyJ.ChakrabartiD.BhattacharyaIntrathecal tramadol added to bupivacaine as spinal anesthetic increases analgesic effect of the spinal blockade after major gynaecological surgeriesIndian J Pharmacol40200841804182
- J.C.ChenE.R.SmithM.CahillR.CohenJ.B.FishmanThe opioid receptor binding of dezocine, morphine, fentanyl, butorphanol and nalbuphineLife Sci521993389396
- C.G.PickD.PaulG.W.PasternakNalbuphine, a mixed kappa 1 and kappa 3 analgesic in miceJ Pharmacol Exp Ther262199210441050
- M.K.GunionA.M.MarchionineC.T.M.AndersonUse of the mixed agonist–antagonist nalbuphine in opioid based analgesiaAcute Pain620042939
- X.CulebrasG.GaggeroJ.ZatloukalC.KernR.MartiAdvantages of intrathecal nalbuphine, compared with intrathecal morphine, after cesarean delivery: an evaluation of postoperative analgesia and adverse effectsAnesth Analg912000601605
- A.K.TiwariG.S.TomarJ.AgrawalIntrathecal bupivacaine in comparison with a combination of nalbuphine and bupivacaine for subarachnoid block: a randomized prospective double blind clinical studyAm J Ther62013592595
- C.SchmaussC.DohertyT.L.YakshThe analgetic effects of an intrathecally administered partial opiate agonist, nalbuphine hydrochlorideEur J Pharmacol861198217
- C.SchmaussT.L.YakshIn vivo studies on spinal opiate receptor systems mediating antinociception. II. Pharmacological profiles suggesting a differential association of mu, delta and kappa receptors with visceral chemical and cutaneous thermal stimuli in the ratJ Pharmacol Exp Ther22811984112
- T.L.YakshR.L.KohlT.A.RudyInduction of tolerance and withdrawal in rats receiving morphine in the spinal subarachnoid spaceEur J Pharmacol4231977275284
- E.GebertJ.SarubinK.A.YoeungMorphine intrathecally in postoperative and cancer-induced painAnaesthesist29121980653655
- N.RawalL.NuutinenP.P.RajS.L.LoveringA.H.GobutyJ.HargardineBehavioral and histopathologic effects following intrathecal administration of butorphanol, sufentanil, and nalbuphine in sheepAnesthesiology756199110251034
- M.L.LinThe analgesic effect of subarachnoid administration of tetracaine combined with low dose of morphine or nalbuphine for spinal anaesthesiaMa Zui Xue Za Zhi301992101105
- K.GuptaB.RastogiP.K.GuptaI.SinghM.BansalV.TyagiIntrathecal nalbuphine versus intrathecal fentanyl as adjuvant to 0.5% hyperbaric bupivacaine for orthopedic surgery of lower limbs under subarachnoid block: a comparative evaluation. IndianJ Pain3020169095
- J.Y.YoonY.S.JeeJ.Y.HongA comparison of analgesic effects and side effects of intrathecal morphine, nalbuphine and morphine–nalbuphine mixture for pain relief during a caesarean sectionKorean J Anaesthesiol422002627633
- Hala MostafaGomaaNashwa NabilMohamedHeba Allah HusseinZoheirMohamad SaeidAliA comparison between post-operative analgesia after intrathecal nalbuphine with bupivacaine and intrathecal fentanyl with bupivacaine after cesarean sectionEgypt J Anaesth302014405410
- C.SomratK.OranuchU.KetchadaS.SiriprapaR.ThipawanOptimal dose of nalbuphine for treatment of intrathecal-morphine induced pruritus after caesarean sectionObstet Gynaecol Res2531999209213
- J.A.AlhashemiE.T.CrosbyW.GrodeckiP.J.DuffyK.A.HullC.GallantTreatment of intrathecal morphine-induced pruritus following caesarean sectionCan J Anaesth4410199710601065
- S.CharuluxanananO.KyokongW.SomboonviboonS.LertmaharitP.NgamprasertwongK.NimcharoendeeNalbuphine versus propofol for treatment of intrathecal morphine-induced pruritus after cesarean deliveryAnesth Analg9312001162165
- S.CharuluxanananO.KyokongW.SomboonviboonA.NarasethakamolP.PromlokNalbuphine versus ondansetron for prevention of intrathecal morphine-induced pruritus after cesarean deliveryAnesth Analg966200317891793
- A.A.MoustafaA.S.BaarorI.A.AbdelazimComparative study between nalbuphine and ondansetron in prevention of intrathecal morphine-induced pruritus in women undergoing cesarean sectionAnesth Essays Res102201623824410.4103/0259-1162.167839
- R.FournierE.Van GesselM.MacksayZ.GamulinOnset and offset of intrathecal morphine versus nalbuphine for postoperative pain relief after total hip replacementActa Anaesthesiol Scand4482000 Sep940945 PMID:10981570
- M.SapateP.SahuW.S.ThatteR.DubeyA randomized, double blind, control study of the effects of adding nalbuphine to spinal bupivacaine for lower abdominal surgeries in elderly patientsAnaesth Pain Inten Care1722013145148
- Moustafa AbdelazizMoustafaRabab SaberSalehNalbuphine added to intrathecal morphine in total knee arthroplasty; effect on postoperative analgesic requirements and morphine related side effectsAlex J Med482012175178
- A.SchmitzB.SalgoM.WeissC.M.DillierA.FrotzlerA.C.GerberIntrathecal opioid medication for perioperative analgesia in severely handicapped children undergoing spinal operationsAnaesthesist597201061462010.1007/s00101-010-1733-7 PMID:20574762
- S.W.KrechelM.A.HeliksonD.KittleG.W.EggersJr.Intrathecal morphine (ITM) for postoperative pain control in children: a comparison with nalbuphine patient controlled analgesia (PCA)Paediatr Anaesth531995177183
- J.D.TobiasC.MateoM.J.FerrerD.F.JimenezC.M.BaroneL. Reyesde CastroIntrathecal morphine for postoperative analgesia following repair of frontal encephaloceles in children: comparison with intermittent, on-demand dosing of nalbuphineJ Clin Anesth941997280284
- Riham HusseinSalehMohammad FaroukYousefHeba MohammadNassarTamer Fathy.YounesEffect of nalbuphine as an adjuvant on levobupivacaine induced caudal analgesia in children undergoing surgical procedures, controlled randomized double blinded studyEgypt J Anaesth32201697102
- Atef KamelSalamaComparison between caudal levobupivacaine versus levobupivacaine–nalbuphine for postoperative analgesia in children undergoing hernia repair: A randomized controlled double blind studyEgypt J Anaesth3220168387
- ArghyaMukherjeeAnirbanPalJitendraAgrawalAmritaMehrotraNidhiDawarIntrathecal nalbuphine as an adjuvant to subarachnoid block: what is the most effective dose?Anesth Essays Res522011171175 PMCID: PMC4173402
- B.JyothiS.GowdaS.I.ShaikhA comparison of analgesic effect of different doses of intrathecal nalbuphine hydrochloride with bupivacaine and bupivacaine alone for lower abdominal and orthopedic surgeriesIndian J Pain2820141823
- Ashraf M.EskandrAyman M.EbeidRole of intrathecal nalbuphine on prevention of postspinal shivering after knee arthroscopyEgypt J Anaesth322016371374
- R.G.JannuzziNalbuphine for treatment of opioid-induced pruritus: a systematic review of literatureClin J Pain32120168793
- ZhengZengJianhuaLuChangShuYuanliChenTongGuoQing-pingWuA comparison of nalbuphine with morphine for analgesic effects and safety: meta-analysis of randomized controlled trialsSci Rep5201510927