1 Introduction
Congenital heart disease is the most common congenital problem in the children representing nearly 25% of all congenital malformations [Citation1]. Children with congenital cyanotic heart disease (CCHD) undergoing corrective cardiac surgery have poorer clinical outcome than acyanotic patients as regard myocardial reoxygenation/reperfusion injury following similar periods of ischemic cardioplegic arrest [Citation2]. Normoxic cardiopulmonary bypass (CPB) has been shown to ameliorate reoxygenation injury in cyanotic pediatric patients and leads to almost complete functional recovery [Citation3].
Cardiopulmonary bypass is associated with variable degrees of vasoconstriction and arteriovenous shunting leading to tissue hypoperfusion, shunting of arterial blood into the venous system without delivery sufficient oxygen with increased endogenous catecholamine levels [Citation4].
Phentolamine is α-adrenergic blocking agent that can antagonize the vasoconstriction produced by endogenous catecholamines that improves the tissue perfusion and decreases the systemic anaerobic metabolism [Citation5]. The aim of this study is to find out the best technique during CPB to improve the immediate postoperative outcome in children with CCHD. We hypothesized that phentolamine infusion may improve the immediate postoperative outcome of open heart surgery in children with CCHD during normoxic CPB. The primary outcome was to assess tissue perfusion as indicated by serum lactate, while the secondary outcome was to evaluate renal and cardiac functions.
2 Materials and methods
After approval from research ethical committee of our institution and informed written consent from the parents of the children. This prospective randomized clinical study was conducted on sixty patients of either sex, their age between 6 and 36 months, with physical status III-IV according to the American Society of Anesthesiologists (ASA) who scheduled for elective open heart surgery for repair of congenital cyanotic cardiac defects [Fallot's tetralogy, transposition of great arteries (TGA), and total anomaly pulmonary venous connection (TAPVC)] in Mansoura University Children Hospital in the period between (June 2015 to June 2016). All patients were in stable condition without preoperative ventilator or inotropic support. Patients with severe coagulopathy, redo open heart surgery, other associated non cardiac congenital anomalies (hydrocephalus, spina bifida or polycystic kidney) or non palpable peripheral pulses preoperatively (e.g., accompanying coarctation of the aorta) were excluded from the study.
All patients were premedicated with intramuscular midazolam (0.1 mg/kg), ketamine (2 mg/kg) and atropine (0.02 mg/kg) 15 min before induction of anesthesia. Anesthesia was induced by sevoflurane in 100% oxygen, fentanyl (3–5 μg/kg iv) and rocuronium (0.6 mg/kg iv) to facilitate endotracheal intubation, and maintained with sevoflurane, rocuronium (0.3 mg/kg/h) and fentanyl (5 μg/kg/h). After induction of anesthesia a radial or femoral arterial catheter and a right internal jugular central venous catheter were inserted under complete aseptic precautions. Mechanical ventilation was adjusted to achieve the end tidal carbon dioxide (Etco2) between 35 and 40 mmhg with fraction of inspired oxygen (fio2) of 0.60 which increased to 1.0 depending on arterial oxygen saturation.
The surgical approach to the heart was through median sternotomy. Heparin 30–40 mg/kg was administered via central vein for anticoagulation to achieve activated clotting time (ACT) greater than 480 s with aortobicaval cannulation before initiation CPB. A membrane oxygenator and a non pulsatile roller pump were used. The pump flow was (100–150) ml/kg/min that maintained mean arterial pressure (40–70) mmHg. The pump was primed with blood or a colloid solution (human plasma) depending on the preoperative hematocrit value allowing moderate hemodilution to maintain hematocrit between 25–28% with cooling the patient to had a mild systemic hypothermia (32 °C).
The patients were randomly distributed via closed envelop assignment into three groups. Each group had twenty patients.
Hyperoxic group (H) (no = 20): according to the protocol of our institution, the pump prime was recirculated with 100% oxygen and the patient received high level of oxygen (100% oxygen) at the beginning of CPB and for 5 min then fio2 was decreased gradually to maintain PaO2 in the range of 200–300 mmHg during CPB.
Normoxic group (N) (no = 20): Fio2 on CPB was controlled and increased gradually by initiating CPB with an fio2 of 0.21. The pump prime was recirculated with room air before initiating CPB. Immediately after full flow of CPB, fio2 was increased gradually from 0.21 to 0.5 within five minutes to maintain PaO2 in the range of 150–200 mmHg.
Phentolaminenormoxic group (P) (no = 20): phentolamine (Regitine: Ciba-Geigy, Basel, Switzerland) was infused at a dose 0.5 μg/kg/min during normoxic CPB and fio2 was managed as normoxic group.
Each patient received 50 ml/kg as a single bolus dose cold cardioplegia (Custdiol), this is HTK crystalloid cardioplegia which is given once and provides myocardial protection up to 3 h, immediately after aortic cross clamping in ante grade manner in the aortic root. After full filling the criteria of weaning off CPB, the patients was separated from CPB and protamine sulphate was administered slowly in a dose of 1 mg for each 1 mg heparin over (5–10) minutes, if ACT was greater than 20% of the preoperative value, additional dose of protamine was given. All patients were transferred to ICU after surgery while they were intubated and mechanically ventilated.
3 Recorded data
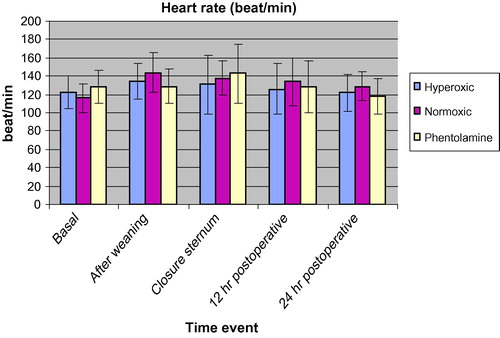
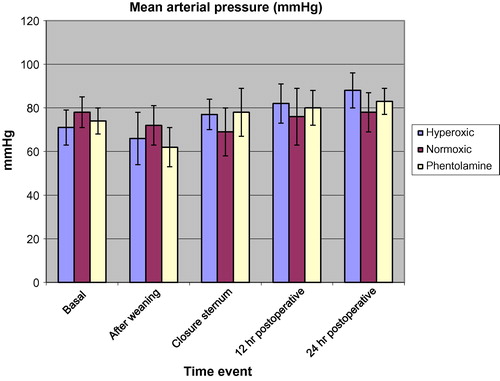
The perioperative heart rate (HR) and mean arterial blood pressure (MAP) were recorded; before induction of anesthesia (basal value), 15 min after weaning off CPB, after closure of the sternum and 12, 24 h after surgery. Aortic cross clamp time (min), CPB time (min), nasopharyngeal to rectal temperature gradient (°C) at the time of weaning, type of inotropic support and its dose (μg/kg/min) and duration of surgery (h) were also recorded. Serum lactate (m mol/L) was measured at the end of CPB and 6 h after surgery, also urine output (ml/kg/min) was assessed at the time of weaning fromCPB. The evidence of myocardial injury was indicated by measuring cardiac troponin T (ng/ml) and CPK MB (ng/ml) 15 h after surgery. The following postoperative data were also recorded, time to extubation (h), intensive care unit (ICU) (hr) and hospital (days) length of stay, duration of inotropic support (hr) and serum creatinine (mg/dl) at the first, third and fifth days after surgery. The postoperative neurologic function was assessed for any evidence of seizures, sensory or motor deficits.
4 Sample size calculation
A Priori G-power was done to estimate study sample size. A power of 80% was estimated with type Í error of 0.05 using the difference in serum lactate between the groups as the primary outcome with the effect size 0.5 to yield of total sample size of 60 cases (20 cases per group).
5 Statistical analysis
Statistical analysis was performed using SPSS version 22 (IBM, SPSS Inc, Chicago, IL, USA). Data were tested for normality using the Kolmogorov-Smirnov test. Continuous data of normal distribution were analyzed with the ANOVA test. Non-normally distributed data were analyzed with the Mann-Whitney U test. Nominal data were analyzed with the Chi-square test and Fisher’s exact test. Post hoc intergroup comparisons were obtained via Bonferonni’s correction. Data of normal distribution are presented as mean ± standard deviation (SD) or number and percentage (n %). A p-value, 0.05 or less was considered statistically significant.
6 Results
The demographic data (age, weight, sex, gender and height) and type of congenital cyanotic heart disease were comparable in the three studied groups ().
Table 1 Patient demographic data and type of congenital cyanotic heart disease in the studied groups.
The recorded readings of HR and MAP of the three groups did not show any statistical significance ( and respectively).
The surgical and CPB characteristics including aortic cross clamp time, CPB time, type of inotropic support and its dose and duration of surgery were similar in the studied groups ().
Table 2 Intraoperative variables in the studied groups.
Nasopharyngeal to rectal temperature gradient at the time of weaning off CPB was significantly lower (P < 0.05) in phentolamine group when compared with both hyperoxic and normoxic group ().
, showed that serum lactate measured at the end of CPB and 6 h after surgery was significantly lower (P < 0.05) in phentolamine group when compared with both hyperoxic and normoxic group, also urine output at the time of weaning off CPB was significantly higher in phentolamine group than both hyperoxic and normoxic group.
Table 3 Serum lactate (m mol/L) at the end of CPB and 6 h after surgery, urine output at end of CPB (ml/kg/min), cardiac troponin T (ng/ml) and Cardiac CPK MB (ng/ml) 15 h after surgery.
Cardiac troponin T and CPK MB measured 15 h after surgery was significantly lower (P < 0.05) in phentolamine and normoxic groups than hyperoxic group ().
The time for extubation was significantly shorter (P < 0.05) in phentolamine and normoxic groups than hyperoxic group (). The other postoperative data, ICU and hospital length of stays, duration of inotropic support and serum creatinine at the first, third and fifth days after surgery showed no significant difference between the studied groups (). As regard postoperative neurological outcome, one patient in normoxic group developed seizures once 22 h after surgery without any evidence of sensory or motor deficits.
Table 4 Postoperative variables in the studied groups.
7 Discussion
The aim of this randomized controlled study was to determine the effects of phentolamine infusion during CPB when combined with normoxia on the immediate postoperative outcome in children with cyanotic congenital heart disease when compared with normoxic CPB without phentolamine infusion and the standard hyperoxic bypass.
The current study demonstrated that phentolamine infusion when combined with normoxic CPB led to significant decreases in the gradient of temperature between nasophrynx and rectum measured at the end of CPB, decrease in serum lactate measured at the time of weaning off CPB and 6 h after surgery and increased urine output during CPB when compared with both hyperoxic and normoxic CPB. Normoxia or the combination of normoxia and phentolamine infusion were associated with significant decreases in serum cardiac troponin T and CPK MB measured 15 h after surgery with shorter intubation time when compared with hyperoxic group.
Cardiopulmonary bypass represents a non physiologic condition associated with impaired hemostasis, changes in hormonal levels and decreased organ perfusion which is tolerated during hypothermia [Citation6].
Hypothermic CPB is associated with intense vasoconstriction with decreased blood flow to the peripheral vascular beds such as muscles and skin which is slowly rewarmed during the rewarming phase of CPB leading to inadequate perfusion of peripheral tissues which results in metabolic acidosis. The temperature of peripheral compartment represented by rectal probe remains hypothermic despite of the normal core temperature represented by the nasopharyngeal probe [Citation7]. Phentolamine is an alpha adrenergic antagonist which is reversible and non selective, its main action is vasodilatation caused by alpha 1 blockade [Citation8].
In accordance to the current study, Koner et al. [Citation22] showed that, phentolamine infusion during CPB is associated with homogenous heat distribution as regard core and peripheral temperature with decreased lactate level [Citation5]. They attributed these results to improvement of tissue perfusion resulting from phentolamine infusion during CPB. Sodium nitroprusside, another vasodilator, when infused during rewarming phase of CPB improves the rewarming of peripheral compartment and reduces the incidence of postoperative hypothermia [Citation9].
Imoto et al. studied the effects of chlorpromazine as a systemic vasodilator administered during CPB in neonatal cardiac surgery, they found that the rate of rise of core temperature didn’t differ significantly between the chlorpromazine and control group, while the rate of rise in peripheral temperature is significantly higher in chlorpromazine group indicating more homogenous heat distribution. They found also that urine output is significantly higher in chlorpromazine group than the control group [Citation10]. The adequacy of tissue perfusion during CPB is monitored by lactate level, base excess and urine output. Lactate is the main indicator of tissue perfusion [Citation11]. Microcirculation is impaired during non pulsetile hypothermic CPB leading to tissue hypoxia which may be compensated by redistribution of blood without any change in serum lactate that will be elevated when the regional perfusion is returned to normal level (wash out) [Citation12,Citation13].
The current study demonstrated that serum cardiac troponin T, CPK MB and intubation time were significantly lower in phentolamine and normoxic groups than the hyperoxic group, this in agreement to Babu et al. who studied thirty-one cyanotic children assigned into two groups, in one of them CPB was initiated with fio2 0.21 for one minute, then increased gradually to 0.6 over 5 min (intervention group), while in hyperoxic group, CPB was initiated from the start with Fio2 greater than 0.6. They found that the intervention group was accompanied with significantly lower postoperative cardiac CPK MB level and shorter intubation time when compared with the hyperoxic group [Citation14].
Caputo et al. studied sixty-seven child with cyanotic heart disease undergoing either controlled noromoxic or htperoxic CPB for corrective cardiac surgery, they reported lower serum troponin T level in controlled noromoxic than hyperoxic group [Citation15].
Re oxygenation injury occurs during hyperoxic CPB in children with cyanotic heart disease as demonstrated in both experimental and clinical studies [Citation16–Citation18]. Modi et al. studied twenty-nine children with CHD undergoing CPB, 20 of them were cyanotic. All patients were exposed to hyperoxic CPB for at least 30 min at the beginning of bypass. They reported an increase in serum level of cardiac troponin T in all patients which was significantly higher in cyanotic than acyanotic children by three folds [Citation18].
In contrast to our study Smit et al. found that, the near physiologic oxygen state don’t reduce myocardial damage as indicated by CPK MB and troponin T when compared with moderate hypoxia in patients submitted to coronary bypass surgery [Citation19].
Decreased CPK MB level in phentolamine and normoxic in this study indicates the lower extend of myocardial injury during the period of myocardial ischemia caused by aortic clamping and reperfusion of myocardium after declamping the aorta [Citation14]. The short intubation time in phentolamine and normoxic groups may be attributed to earlier myocardial recovery with maintenance of cardiac output together with preservation of both lungs. Experimental studies in immature hypoxic piglets have been reported reduced pulmonary function as a result of hyperoxic CPB [Citation20].
One patient in normoxic group developed seizures once 22 h after surgery without any neurological deficits which may be caused by micro emboli of air bubbles occurred during CPB. Naim et al. reported that continuous electroencephalographic monitoring after cardiac surgery in neonates with CPB detected seizures in 8% of neonates. Most of seizures had no clinical significance and occurred once without any subsequent relapse [Citation21].
8 Conclusion
Phentolamine infusion during normoxic CPB is associated with improved immediate post operative outcome in children with CCHD. This is in the form of preservation of myocardial function (as indicated by postoperative cardiac enzymes, CPK MB and cardiac troponin T), renal function (as indicated by increased urine output), tissue perfusion (decreased lactate level) and more homogenous heat distribution as regard core and peripheral temperature.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
No fund sources.
Acknowledgments
We would like to thank dr: Nabil Abd el raouf (professor of anesthesia and intensive care) and dr: Adel El Gamel (professor of pediatric cardiac surgery) for their cooperation and advice to achieve this study.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- J.I.HoffmanS.KaplanThe incidence of congenital heart diseaseJ Am CollCardiol39200218901900
- H.ImuraM.CaputoA.ParryA.PawadeG.D.AngeliniM.S.SuleimanAge-dependent and hypoxia-related differences in myocardial protection during pediatricopen heart surgeryCirculation103200115511556
- K.IhnkenK.MoritaG.D.BuckbergDelayed cardioplegicreoxygenation reduces reoxygenation injury in cyanotic immature heartsAnn Thorac Surg661998177182
- CK.TanSN.GlissonAA.El-EtrKB.RamakrishnaiahLevels of circulating norepinephrine and epinephrine before during and after cardiopulmonary bypass in manJ ThoracCardiovasc Surg711976928931
- Ö.KönerS.TekinA.KönerN.SoybirS.SerenK.KaraogluEffects of phentolamine on tissue perfusion in pediatric cardiac surgeryJ CardiothoracVascAnesth131999191197
- Farsak B, Mehmet Öç, Gümüş F, BaharÖç, Erentuğ V. Effects of Perfusion Temperature on Inflammatory Response and Outcome Following Cardiopulmonary Bypass. J Acad Res Med (JAREM) 2012;2:10–4.
- C.D.DeakinG.W.PetleyD.SmithPharmacological vasodilatation improves efficiency of rewarming from hypothermic cardiopulmonary bypassBr J Anaesth811998147151
- G.BrockOral phentolamine (Vasomax)Drugs Today (Barc)362000121124
- P.N.FymanJ.E.CottrellL.KushinsP.A.CasthelyVasodilator therapy in the perioperative periodCan AnaesthSoc J331986629643
- Y.ImotoH.KadoM.MasudaH.YasuiEffects of chlorpromazine as a systemic vasodilator during cardiopulmonary bypass in neonatesJpn J ThoracCardiovasc Surg502002241245
- R.MunozP.C.LaussenG.PalacioChanges in whole blood lactate levels during CPB for surgery for congenitalcardiac disease: an early indicator of morbidity and mortalityJ ThoracCardiovasc Surg1192000155162
- L.LandowSplanchnic lactate production in cardiac surgery patientsCrit Care Med211993S84S91
- Adluri RK, Singh AV, Skoyles J, Baker M, Mitchell IM. Measurement of intraperitoneal metabolites during hypothermic cardiopulmonary bypass using microdialysis. ScandCardiovasc J 2011;45:229–35.
- Babu B, Bhat S, Prabuswamy HP, Kamalapurkar G, Kumar HJ, Libu KG, et al. Controlling oxygenation during initiation of cardiopulmonary bypass: can it improve immediate postoperative outcomes in cyanotic children undergoing cardiac surgery? A prospective randomized study. World Journal for Pediatric & Congenital Heart Surgery(WJPCHS) 2012;3:310–6.
- M.CaputoA.MokhtariC.A.RogersN.PanayiotouQ.ChenM.B.T.GhorbelThe effects of normoxic versus hyperoxic cardiopulmonary bypass on oxidative stress and inflammatory response in cyanotic pediatric patients undergoing open cardiac surgery: a randomized controlled trialJ Thoracic Cardiovascul Surg1382009206214
- Buckberg, GD. Studies of hypoxemic/reoxygenation injury without aortic clamping. I. Linkage between cardiac function and oxidant damage: an overview. J ThoracCardiovascSurg 1995;110:1166–70.
- Ihnken K, Morita K, Buckberg GD, Sherman MP, Young HH. Studies of hypoxemic/reoxygenation injury: without aorticclamping. III. Comparison of the magnitude of damage by hypoxemia/reoxygentation versus ischemia/reperfusion. J ThoracCardiovascSurg 1995;110:1182–9.
- P.ModiH.ImuraM.CaputoA.PawadeA.ParryG.D.AngeliniCardiopulmonary bypass induced myocardial reoxygenation injury in pediatric patients with cyanosisJ ThoracCardiovascSurg124200210351036
- B.SmitYM.SmuldersMC.WaardC.BoerAB.VonkKD.VeerhoeModerate hyperoxic versus nearphysiological oxygen targets during and after coronary artery bypass surgery arandomized controlled trialCrit Care20201655
- K.S.BollingA.HalldorssonB.S.AllenS.RahmanT.WangM.KrononPrevention of the hypoxic reoxygenation injury with the use of a leukocyte depleting filterJ ThoracCardiovasc Surg113199710811089
- M.Y.NaimJ.W.GaynorJ.ChenS.C.NicolsonS.FullerT.L.SpraySubclinical seizures identified by postoperative electroencephalographic monitoring are common after neonatal cardiac surgeryJ ThoracCardiovasc Surg1502015169178
- O.I.KonerS.TekinA.KonerEffects of phentolaminne on tissue perfusion in pediatric cardiac surgeryJ Cardiothorac Vas Anesth1321999191197