Abstract
Background
Reduction of anesthesia cost has become a necessity, especially in developing countries. Recently, automated control of end-tidal sevoflurane concentration (EtSev) has been proposed as a new technique with both cost-effectiveness and safety profiles. In this study, sevoflurane consumption (primary outcome variable) was evaluated during living donor hepatectomy using automated control of EtSev (EtC) at fresh gas flow (FGF) of 0.5 and 2 L/min compared to manual control (MC) technique at FGF of 2 L/min.
Materials and methods
Prospective, randomized, controlled trial including 60 Potential donors scheduled for living donor right hepatectomy. patients were randomized into 3 equal groups (according to target control of sevoflurane), MC group, EtC-2L group, and EtC-0.5L group. In MC group: FGF was set to 2 L/min, inspired concentration of Sevoflurane (FiSev) was set to 1.5–2% in 0.4 fractional inspired oxygen concentration (FiO2), while in EtC-2L group: FGF was set to 2 L/min, EtSev was set to 1–1.5% with end tidal oxygen concentration (EtO2) target of 0.35. In EtC-0.5L group, FGF was set to minimal flow and EtSev target to 1–1.5% and EtO2 target of 0.35. Anesthetic gases consumption (sevoflurane ml, Oxygen L, and air consumption L) per anesthesia hour were recorded at the end of surgery. Other recorded data included intraoperative hemodynamics, the number of user adjustments, and extubation time.
Results
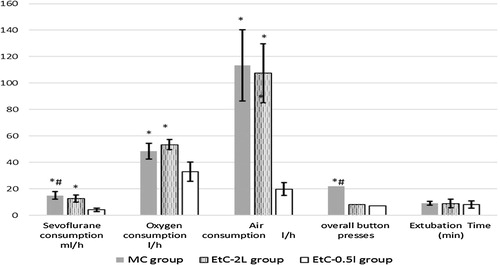
Significant reduction in sevoflurane consumption when EtC-0.5L is used (4.2 ± 1.3 ml/h, 12.6 ± 2.6 ml/h, and 15 ± 2.9 ml/h respectively, p. 0.001). Also, a significant decrease in overall numbers of user adjustments between the three groups (8 times for EtC-0.5L group, 7 times in EtC-2L group, 22 times for MC group, p. 0.008) was observed.
Conclusion
automated control of EtSev during anesthesia of living donor hepatectomy significantly lowers sevoflurane consumption and decreases required user interventions without deleterious effect on patient safety.
1 Introduction
Economic load of health care including costs for anesthesia delivery has been increasing. Facing the global economic constraints, reduction of anesthesia cost has been a necessity [Citation1,Citation2]. Inhalational anesthetics accounts for 20% of the cost related to anesthetic drug costs [Citation3,Citation4]. Recently, End-tidal control (EtC) of sevoflurane anesthesia has been proposed as a new technique applying for both cost-effectiveness and safety concerns. Additionally, EtC mode requires less anaesthesiologist interventions; expressed mostly as press-buttons, which was an extra burden when minimal or low flow anesthetic technique is applied especially in long surgeries [Citation5].
Classically, the inspired concentration of inhalational anesthetic, fresh gas flow rate (FGF), and inspired concentration of oxygen (FiO2) are manually modified by anesthesiologists according to operative findings. New anesthetic machines; Drager Zeus, GE Aisys, and Maquet flow-I, incorporated a closed loop system, in which the target end-tidal anesthetic concentration, minimum flow rate, and target end-tidal oxygen concentration (EtO2) are set, then the machine automatically modifies inspired agent and fio2 to maintain end-tidal concentrations determined by the anesthesiologist. This is assumed to lower anesthetic gases consumption with more stable brain concentration resulting in less required anesthesiologist interventions to modify either inhaled anesthetic or oxygen concentrations [Citation5–Citation7].
Most of the studies that investigated EtC were conducted for relatively short period surgeries and non-homogenous patients [Citation6,Citation8–Citation12]. In our study, we applied EtC mode (Aisys CS2 anesthesia delivery systems, USA) during living donor right hepatectomy where the average anesthetic duration is around 6 h [Citation7,Citation13]. This offers an optimal situation to investigate the effects of the new technique of inhalational anesthetic control. To our knowledge, this is the first study that utilized automated end-tidal control mode in such long surgery and homogenous patient population.
Gas sparing effect of EtC can be attributed to lower FGF applied [Citation3]. To investigate this point, this study applied ETC mode at two different FGF rates (0.5 L/min in one group and 2 L/min in another group). Both groups were compared to manual control (MC) group. Sevoflurane consumption was evaluated as the primary outcome variable while secondary variables included hemodynamic effects and number of anesthesiologist interventions.
2 Materials and methods
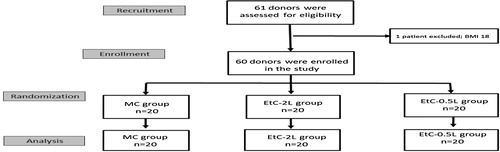
After obtaining institutional review board approval (R-15.12.84) and clinical trial registry (http://www.clinicaltrials.gov: NCT02676934), a written consent was taken from donors scheduled for living donor hepatectomy from July 2015 to September 2016. Included patients were of either sex, aging from 20 to 45 years, body mass index (BMI) between 20 and 30 kg/m2, with residual liver volume more than 500 g or 30% measured total liver volume (calculated by computed tomography liver volumetry). Patients were randomly allocated (using closed envelope technique in 4 blocks of 15) into three groups according to target control of sevoflurane; MC group n = 20 and EtC-2L group n = 20, and EtC-0.5L (n = 20). .
Patients were assessed according to local policy of our liver transplantation program. Prior to induction of Anesthesia, patients were monitored for electrocardiography (ECG), non-invasive blood pressure (NIBP), peripheral oxygen saturation (Spo2). Pantoprazole 40 mg and Midazolam 3 mg were injected intravenously as a premedication. After preoxygenation, anesthesia induction was done by intravenous injection of 1–2 mg/kg propofol 1% (Propofol 1%, Fresenius) till loss of verbal contact, 2 µg/kg fentanyl citrate (Fentanyl-Janssen) and 0.9 mg/kg rocuronium bromide (Esmoron, Organon). Anesthesia was maintained with sevoflurane (sevoflurane, Abbott) to obtain a bispectral index (BIS) value between 40 and 60 (BIS View Monitoring System, Aspect Medical System, Norwood, MA, USA). Muscle relaxation was ensured by intravenous infusion of rocuronium (0.6 mg/kg/h) to maintain 0–2 train-of-four responses of the adductor pollicis muscle after the stimulation of the ulnar nerve throughout Anesthesia (TOF, Aisys Anesthesia Care station). Intraoperative analgesia provided during anesthesia with IV infusion of fentanyl (1 µg/kg/h). Core body temperature (esophageal probe) was kept above 36 °C and EtCO2 was maintained between 30 to 35 mmHg. Inspired sevoflurane concentration (FiSev), end-tidal concentration of sevoflurane (EtSev), inspired fraction of oxygen (FiO2), end-tidal fraction of oxygen (EtO2), end-tidal carbon dioxide concentration (EtCO2) were continuously monitored.
Immediately after intubation, patients were connected to anesthesia machine and anesthesia gas delivery adjusted according to allocated group to keep BIS between 40–60. In MC group: FGF was set to 2 L/min, FiSev was set to 1.5–2% with FiO2 of 0.4. In EtC-2 group: FGF was set to 2 L/min, EtSev was set to 1–1.5% with FiO2 of 0.35. In EtC-0.5 group, FGF was set to min flow (0.5 L/min), EtSev was set to 1–1.5% with FiO2 of 0.35. Immediately after skin closure, Sevoflurane was stopped and a FGF of 6 L/min was used till extubation criteria are fulfilled.
In the case of increased HR or MAP by more than 20% of patient's baseline readings, sevoflurane concentration is increased by 0.2% to a maximum EtC of 2% or FiSev of 3% according to the study group. If no response, a bolus of fentanyl 1 mcg/kg is injected. Otherwise, incremental doses of propranolol 0.2 mg can be used. If MAP falls by more than 20%, patient volume status was assessed simultaneously with surgical field visual assessment and communication with the surgical team. otherwise, 5 mg of ephedrine can be injected intravenously. Atropine 0.5 mg was given intravenously in the case of bradycardia.
Patient’s age, weight, height, basal heart rate (HR), basal mean arterial pressure (MAP) were recorded. During surgery, HR, MAP, BIS, anesthesia gas analysis data (FiSev, EtSev, FiO2, EtO2) were recorded hourly. At the end of surgery, anesthesia duration, total gas consumption (sevoflurane [ml/min], Oxygen [L/min], and air consumption [L/min]) were obtained from machine log. Time from terminating sevoflurane delivery until extubation was calculated (extubation time). The number of interventions needed by anesthesiologist to modify target sevoflurane and/or FGF during anesthetic period was also recorded. The incidence of perioperative hypoxia (Spo2 ≤ 94%), hypercapnia (EtCO2 ≥ 40 mmHg), and accidental awareness during anesthesia (assessed by Brice interview [Citation14] on day 1 postoperatively) were recorded.
1.1 Statistical analysis
For Sample size assessment, authors used G∗power software version 3.1.10. Based on the results of a pilot study conducted on similar group of patients in our program, comparing sevoflurane consumption in 15 patients; 5 per group (7 ± 1 ml/h for EtC-0.5L group, 12 ± 3 ml/h for EtC-2L group, 13 ± 3 ml/h for MC group), a total sample size of 60 patients was found sufficient for a study power of 90% with alpha error of 0.05.
We used Statistical package for social sciences (SPSS) software version 20 to tabulate and analyze recorded data. Continuous data with a normal distribution as shown by Shapiro-Wilk test were represented as mean ± SD, otherwise, Median [IQR] was used. Nominal data and categorical data were presented as number (%). Statistical differences between the three studied groups were assessed using one-way ANOVA or Kruskal-Wallis H test as appropriate. Post hoc comparison was achieved by Tukey honestly significant difference test.
2 Results
In this study, 60 patients were randomly divided into three groups according to the technique of control of sevoflurane delivery. We did not found any statistically significant difference between the studied groups regarding patient’s demographics, basal hemodynamics (HR, MAP), anesthesia duration (). Similarly, no difference was detected between intraoperative HR, MAP, or BIS, .
Table 1 patient characteristics in the studied groups, data is presented as mean ± SD.
Table 2 Intraoperative monitoring (HR, MAP, BIS) among the two studied groups; MC group (n = 20), EtC-2L group (n = 20), EtC-0.5L group (n = 20). Data are presented as mean ± SD.
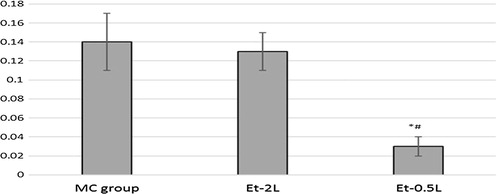
Sevoflurane consumption was significantly lower in EtC-0.5L group than in EtC-2L and MC groups (4.2 ± 1.3 ml/h, 12.6 ± 2.6 ml/h, and 15 ± 2.9 ml/h respectively, p. 0.001). Simultaneously, a significant decrease in overall numbers of user adjustments between the three groups (8 times for EtC-0.5L group, 7 times in EtC-2L group, 22 times for MC group, p. 0.008) was detected . Similarly, oxygen and air consumptions were significantly lower in both EtC-0.5L group and EtC-2L group than in MC group (p-value 0.00), . Consequently, anesthesia-related cost was significantly lower in EtC-0.5L group than both EtC-2L and MC groups (0.03 ± 0.01 $/min for EtC-0.5L group, 0.13 ± 0.2 $/min in EtC-2L group, 0.14 ± 0.3 $/min for MC group, p. 0.002) . As in , time needed to extubation was not statistically different in the 3 groups. No perioperative Hypoxia, hypercapnia, awareness episodes were recorded in the three groups.
3 Discussion
Anesthesiologists have to choose most cost-effective anesthetic technique without compromising service quality or patient safety. A large part the anesthetic drug budget is related to the cost of consumed inhaled anesthetic [Citation3,Citation15,Citation16]. In our study, Mean Sevoflurane consumption per anesthesia hour was significantly lower when EtC was applied. Manufacturers of anesthesia machines have been trying to decrease the cost of modern inhalational agents like desflurane and sevoflurane. The use of low flow during sevoflurane anesthesia has been considered as a way to decrease the anesthesia related expenditure [Citation7,Citation8]. Although a small number of studies investigated EtSev as a target for maintenance of inhalational anesthesia, this mode is offered as a promoted economic delivery technique in which gas flow and vaporizer output are modified to reach the chosen end-tidal concentration [Citation4,Citation5,Citation9,Citation17]. Donor hepatectomy is an optimal surgery to investigate automate control of EtSev because inhalational anesthesia is the preferred method for anesthesia maintenance in most transplant centers. Also, the surgery is lengthy enough to clarify the postulated economic effect [Citation18].
Our study showed that sevoflurane consumption and required user interventions were significantly lower when EtC mode is applied. Likewise, advantages of EtC mode have been shown in several trials. The randomized trial of Potdar and his co-workers compared sevoflurane consumption in two groups, 100 patients each, using EtC and MC. Sevoflurane consumption was significantly lower in EtC group [Citation19]. In the same study, Potdar reported a lower number of adjustments in automated mode group rather than the MC group. Similarly, Tay and his colleagues demonstrated 27% reduction in costs of inhalational anesthetics when Et-control mode was introduced to a teaching hospital in Australia [Citation20]. The impact of adding EtC software was investigated by Singaravelu and his colleagues [Citation12]. They found lower gas consumption when EtC was applied in comparison to FGF control without reaching statistical significance, which may be explained by the shorter duration of anesthetic procedure than in our study.
However, Lucangelo and his colleagues did not show any significant decrease in sevoflurane consumption when EtC is applied in comparison to MC [Citation6]. In their protocol, both manual and automated control groups targeted a fixed Et-Sev level with a FGF at 1 L/min in both study groups. This might explain why sevoflurane uptake was nearly equal especially. The same study [Citation6] demonstrated benefits of EtC mode like similar efficiency, hemodynamic stability, and lower interventions.
An important concern during EtC of sevoflurane application is the safety issues. In our study, we did not record any perioperative complications in any of the study groups. When using EtC, the anesthesiologist sets the EtO2, minimum flow rate and target EtSev concentration [Citation21]. The system monitors these concentrations and automatically adjusts FGF and anesthetic concentrations to ensure maintained patient's uptake. Multiple protective safety mechanisms are integrated into Et-control including minimal flow rate, system checks, fresh gas sampling checks every 3 min, and leak checks. Indirectly, minimizing the need for user intervention can decrease the workload on the attending anesthesiologists, thus decrease complications related to fatigue [Citation22].
Anesthetic agent consumption is related to FGF [Citation15,Citation3,Citation23]. In our study, the effect of different was eliminated through comparison between EtC-2L group in which FGF was set to 2 L/min like in MC, while in EtC-0.5L group the machine fully controlled the FGF and Fisev to reach target EtSev and EtO2. Results are shown in illustrated that targeting EtSev lowers gas consumption even at the same FGF; a privilege that is maximized by allowing the machine to control both FGF and inhaled anesthetic concentration in fully automated mode (EtC-0.5L). This finding is similar to results of two studies that investigated anesthetic gas consumption between EtC and MC mode at the same FGF [Citation9,Citation19].
The economic value of EtC mode must be weighed against the costs of acquiring an anesthesia machine with the mentioned mode or adding the new module to an old machine. As mentioned earlier, new anesthesia machines mostly have the automated mode as a built-in feature that offers no extra burden during purchasing the machine.
Applying our results, the use of EtC mode can save around 11 ml of sevoflurane/hour (5.28 $/anesthesia hour according to 2015 prices) supposing that a FGF of no more than 2 L/h is applied. By a simple equation, yearly savings for a machine that works 6 h daily, 5 days a week, will be over 8000 $.
The inevitably single blinded study design is a considered a limitation in this study, as authors could not figure a practical way to blind responsible anaesthetist to the used mode of inhalational anesthesia control. The economic effect of EtC mode cannot be extrapolated to its use with isoflurane because of its significantly lower price. However, EtC of isoflurane can be used even if with lower savings.
4 Conclusion
Automated EtC of sevoflurane-based anesthesia has a potential clinical and economic benefits. We could not detect additional hazard over patient safety. The use of EtC mode shall be encouraged if available. Further studies may be required to establish its safety and economic benefits.
Conflict of Interest statement
None.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- P.G.KotzeI.F.JuniorC.D.FreitasF.DinizAnalysis of direct costs of anesthesia-related materials between spinal and venous anesthesia with propofol associated with local perianal block in hemorrhoidectomyJ Coloproctol312011268275
- A.TyagiV.VenkateswaranA.K.JainU.C.VermaCost analysis of three techniques of administering sevofluraneAnesthesiol Res Pract2014201416
- I.OdinP.FeissLow flow and economics of inhalational anaesthesiaBest Pract Res Clin Anaesthesiol19200539941310.1016/j.bpa.2005.01.006
- B.G.NairG.N.PetersonM.B.NeradilekS.F.NewmanE.Y.HuangH.A.SchwidReducing wastage of inhalation anesthetics using real-time decision support to notify of excessive fresh gas flowAnesthesiology118201387488410.1097/ALN.0b013e3182829de0
- S.SingaraveluP.BarclayAutomated control of end-tidal inhalation anaesthetic concentration using the GE Aisys Carestation™Br J Anaesth110201356156610.1093/bja/aes464
- U.LucangeloG.GarufiE.MarrasM.FerlugaF.TurchetF.BernabEnd-tidal versus manually-controlled low-flow anaesthesiaJ Clin Monit Comput28201411712110.1007/s10877-013-9516-8
- Wood H, Jones R, Cole H, Willits I. End-tidal Control software for use with Aisys closed circuit anaesthesia systems for automated gas control during general anaesthesia; 2014. http://https://www.nice.org.uk/advice/mib10/chapter/About-this-briefing.
- S.PonsonnardA.GalyJ.CrosA.M.DaragonN.NathanTarget controlled inhalation anaesthesia: a cost-benefit analysis based on the cost per minute of anaesthesia by inhalationAnaesth Crit Care Pain Med201610.1016/j.accpm.2016.02.005
- B.Lortat-JacobV.BillardW.BuschkeF.ServinAssessing the clinical or pharmaco-economical benefit of target controlled desflurane delivery in surgical patients using the Zeus® anaesthesia machineAnaesthesia6420091229123510.1111/j.1365-2044.2009.06081.x
- D.GuptaE.EgerIIInhaled anesthesia: the original closed-loop drug administration paradigmClin Pharmacol Ther842008151810.1038/clpt.2008.85
- G.A.DumontJ.M.AnserminoClosed-loop control of anesthesia: a primer for anesthesiologistsAnesth Analg11720131130113810.1213/ANE.0b013e3182973687
- U.LucangeloG.GarufiE.MarrasM.FerlugaF.TurchetF.BernabèEnd-tidal versus manually-controlled low-flow anaesthesiaJ Clin Monit Comput28201411712110.1007/s10877-013-9516-8
- W.ElsarrafT.SalahA.SultanM.El ShobariM.WahabImpact of sevoflurane versus isoflurane on the coagulation profile in living donor liver transplantation. A comparative studyAin-Shams J Anesthesiol7201426326810.4103/1687-7934.139539
- G.KotsovolisG.KomninosAwareness during anesthesia: how sure can we be that the patient is sleeping indeed?Hippokratia1320098389
- S.A.MillerC.A.AschenbrennerJ.R.TrauneroL.A.BaumanS.S.LobellJ.S.Kelly$1.8 Million and counting: how volatile agent education has decreased our spending $1000 per dayJ Clin Anesth35201625325810.1016/j.jclinane.2016.07.003
- G.NunnLow-flow anaesthesiaContin Educ Anaesthesia Crit Care Pain820081410.1093/bjaceaccp/mkm052
- T.StanleyW.LaurenceP.PhilipS.DavidB.JurisAutomated control of volatile agents consistently reduces its consumption costsBJA4120132013
- A.M.YassenG.ElSayedLow dose ketorolac infusion improves postoperative analgesia combined with patient controlled fentanyl analgesia after living donor hepatectomy – randomized controlled trialEgypt J Anaesth28201219920410.1016/j.egja.2012.02.010
- M.P.PotdarL.L.KamatM.P.SaveCost efficiency of target-controlled inhalational anesthesiaJ Anaesthesiol Clin Pharmacol30201422222710.4103/0970-9185.130026
- S.TayL.WeinbergP.PeytonD.StoryJ.BriedisFinancial and environmental costs of manual versus automated control of end-tidal gas concentrationsAnaesth Intensive Care41201395101
- S.TayL.WeinbergP.PeytonJ.BriedisFinancial and environmental costs of manual versus automated control of end-tidal gas concentrationAnaesth Intensive Care41201395101
- R.MooreP.GuptaNeto GFDOccupational Fatigue: impact on Anesthesiologist’s Health and the Safety of Surgical Patients. As Anesthesiologists We Are Frequently Working in a Stressful Environment. Do You Disagree With This?Braz J Anesthesiol.63201316716910.1016/S0034-7094(13)70209-5
- S.SuttnerJ.BoldtLow-flow anaesthesiaPharmacoeconomics17200058559010.2165/00019053-200017060-00004