Abstract
Study objectives
The present study investigated the effect of dexmedetomidine infusion on bispectral index and hemodynamic values for patients undergoing cesarean section under general anesthesia as well as the postoperative maternal and fetal outcomes.
Design and setting
This is randomized controlled study done in operating rooms and postoperative recovery area.
Patients
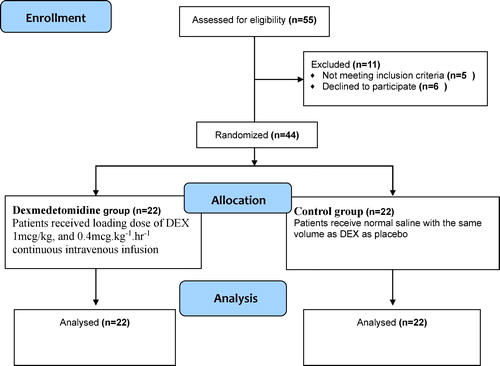
44 Adult healthy pregnant females scheduled for elective Caesarian section delivery under general anesthesia were divided randomly in to two equal groups. Dexmedetomidine group and control group.
Interventions
Unlike control group, Dexmedetomidine group: patients were given intravenous loading dose of DEX 1 mcg/kg before induction of anesthesia then intravenous infusion of DEX 0.4 mcg kg−1 hr−1 throughout surgery.
Measurements
The BIS values; heart rate, blood pressure and MAC were monitored at 15 designated points of sequential events during anesthesia. The maternal sedation in the first postoperative hour was reported every 15 min. Apgar score of the neonates was assessed by the pediatrician 1 min and 5 min interval. All patients were asked about awareness or recall at the time of discharge and 6 h after.
Results
BIS values, blood pressure, heart rate and MAC were significantly lower in DEX group at most different time intervals. Both groups of the study were matched as regard as Apgar score at 1 min. and 5 min. Alderete score was significantly lower in DEX group 15 min after extubation. However, both groups were matched 30 min after extubation. Sedation score was higher in Dex group at 5 and 15 min postoperatively. 10 patients in the control group needed extra dose of fentanyl.
Conclusions
Dexmedetomidine is useful adjuvant during general anesthesia for CS as it attenuates hemodynamic responses to surgical stress, reduces needs for analgesic and anesthetic drugs together with favorable maternal and neonatal outcome.
1 Introduction
Awareness is a serious complication during general anesthesia. It causes adverse psychological sequelae which may lead to postoperative behavior modification [Citation1]. Prevention of pain and awareness during general anesthesia is the major mission of the anesthesiologist. This can be achieved adequate balanced anesthesia using hypnotic, analgesic, and amnesic drugs [Citation2]. There is increased incidence of awareness during general anesthesia for Cesarean section due to rapid sequence induction, avoidance of opioid analgesics and amnesic drugs until the fetal delivery, and the limited concentration of volatile agents [Citation3,Citation4]. This can increase the incidence of post-traumatic stress disorder among these patients. Achievement of adequate depth of anesthesia is an important goal and as such merits more research work [Citation5]. The current approach for evaluating the depth of anesthesia is the assessment of hemodynamics and subjective signs like movement, sweating, and lacrimation, but these are not adequately sensitive or specific [Citation6]. The Bispectral Index (BIS) is an adequately sensitive FDA-approved method for the evaluation of the depth of anesthesia by processing the patient's electroencephalogram (EEG) [Citation7]. Accordingly, the BIS can be used to prevent intraoperative awareness in surgeries with increased risk of light anesthesia like C/S [Citation3]. Dexmedetomidine(DEX) is a highly selective alpha II receptor agonist with many actions like; sedation and analgesia [Citation8]. Dexmedetomidine provides hemodynamic stability, so it can be used as a sedative during surgical and other procedures in non-intubated patients [Citation9]. In 2009, dexmedetomidine has been used safely during normal labour as it provides stability of maternal hemodynamics, sedation, ecbolic effect and less incidence of fetal distress due to its high placental retention [Citation10]. Several Studies have recommended that DEX is safe and effective when used as an adjuvant for general anesthesia with a loading dose of 0.5–1 μg/kg and 0.5–1.0 μg kg−1 min−1 infusion during intravenous or volatile agents [Citation11]. The aim of this study is to evaluate the effect of intraoperative dexmedetomidine infusion on depth of anesthesia and hemodynamics during general anesthesia for Cesarean section. The primary outcome was the effect of dexmedetomidine infusion on Bispectral index values during general anesthesia for cesarean section. The Secondary outcomes were hemodynamic parameters and clinical signs of inadequate depth of anesthesia, Apgar score, sedation score, Alderete score and intraoperative need for excess analgesia.
Informed written consent was done for all patients participating in the study.
2 Materials and methods
Our study was conducted on 44 adult healthy pregnant females scheduled for elective Caesarian section (CS) delivery under general anesthesia in the operating theater at Suez Canal University hospital. Randomization was done using simple random tables and patients were allocated to two equal groups with allocation ratio of 1:1. Allocation sequence was concealed in opaque numbered envelops. Participant patients and anesthesia provider were blinded to the study group. Another anesthesiologist who was blind to the study group was responsible for recording BIS values without interfering with any anesthetic decisions.
Inclusion criteria included Pregnant, full term women (completed 37 weeks), Single or multiple pregnancies, Patients ASA physical status I and II, Patient refusal of regional anesthesia and Infection at the site of injection of spinal anesthesia.
Exclusion criteria included patient Refusal of general anesthesia, previous history of mental disease, signs of active labour, pregnancy related-diseases or antepartum hemorrhage, and presence of Fetal distress.
2.1 Preoperative assessment
Medical history was taken including medical disorders as hypertensive disorders of pregnancy, chest, cardiovascular, liver or kidney diseases, past history of operations or hospitalization, past anesthetic history, allergies to anesthetic drugs, and any previous intraoperative or postoperative complications. General examination, Heart and chest examination, and Airway assessment were done for all patients. Complete blood count, ABO group, RH, and coagulation study were requested for all patients to be done before surgery.
2.2 Intra-operative technique
Airway devices(laryngoscope blade 3 and 4, endotracheal tube size 6.5, bougie, stylet, laryngeal mask and Guedel oro-pharyngeal airway), syringe pump. Anesthetic machine (Avance c/s2™) with capnogragh and gas analyzer, flowmeter and monitor were checked promptly. Monitoring equipment included hemodynamic monitor (Datex-OhmedaTM) with 3leads ECG, non-invasive blood pressure and pulse oximetry and depth of anesthesia monitor (BISTM covidien). Patients were fasting for 6–8 h. Intravenous access was gained using an 18-G cannula. Monitoring equipment was attached to the patients including the BIS.
2.3 Patients were divided into two groups
2.3.1 The first group (DEX group)
Intravenous loading dose of DEX 1 mcg/kg was given over 10 min before induction of anesthesia. Pre-oxygenation with 100% oxygen was done for at least 3–5 min in 10–15 degree left uterine tilted position. Rapid sequence induction was performed using propofol 2 mg/kg and suxamethonium 1.5 mg/kg. Anesthesia was maintained using isoflurane (1–1.5% before delivery and 0.5–1% subsequently according to hemodynamic parameters), DEX 0.4 mcg kg−1 hr−1 continuous intravenous infusion after induction of anesthesia till peritoneal closure. Atracurium 0.4 mg/kg was given after the return of spontaneous respiration. After neonatal delivery, Fentanyl 1 micg/kg was given intravenously, and an infusion of 10 IU oxytocin in 500 ml ringer lactate solution was started.
2.3.2 The second group (control group)
The same as first group but without use of DEX.
Patients in both groups were received additional dose of IV fentanyl 1 mcg/kg if there is increased heart rate and/or arterial blood pressure by more than 20% of the pre-anesthetic values despite reaching the maximum determined isoflurane concentration. Isoflurane was stopped after the start of skin closure. The BIS values, heart rate, blood pressure and MAC were continuously monitored and recorded at 15 designated points of sequential events during anesthesia: Base line, after induction of anesthesia and intubation, skin incision, retraction of abdominal rectus muscles, uterine incision, fetal delivery, uterine curettage, uterine closure, abdominal lavage, closure of peritoneum, closure of subcutaneous tissue, shutoff of Isoflurane, Skin closure, reversal administration and recovery.
Reversal of muscle relaxation was performed by neostigmine 0.04 mg/kg and atropine 0.01 mg/kg. The maternal sedation in the first postoperative hour was reported at 5, 15, 30,45 and 60 min. Sedation score was recorded using five-point scale (1 = completely awake, 2 = awake but drowsy, 3 = asleep but responsive to verbal commands, 4 = asleep but responsive to tactile stimulus, 5 = asleep and not responsive to any stimulus) [Citation12]. Apgar score of the neonates was assessed by the pediatrician 1 min and 5 min interval. All neonates were observed for respiratory depression and bradycardia during the first hour after delivery. All patients were interviewed at the time of discharge from post-anesthetic care unit and 6 h after that for determination of awareness or recall.
2.4 Statistical analysis
A sample size of 20 patients per group was required to detect 8.8 difference between the means of Bispectral Index 10 min after intubation in dexmedetomidine group and control group at a standard deviation of 8.4 [Citation13] with 90% power and a 5% level of significance. Considering a dropout rate of 20%, the sample size required was 44 patients (22 patients per group).
Values were expressed as mean ± standard deviation (continuous variables) or as a percentage of the group from which they were derived (categorical variables). Data with variables completed were analyzed in the study. The data from the groups were compared using the paired Student's t-test, with P value < 0.05 indicating significance.
3 Results
This study includes 44 patients. They were randomly assigned for two equal groups (22 patients/group): Dexmedetomidine group (DEX group) where loading DEX was given before induction of anesthesia and infusion till the end of surgery. Control group: where normal saline with the same volume as Dex was given as a placebo ().
Both groups were matched regarding age, weight, presence of chronic illness and the duration of surgery (p value > 0.05). 4.5% of patients in DEX group have hypertension while hypertension was not present in control group. Diabetes mellitus was noted to be present in 4.5% in both DEX and control group. Duration of surgery was 51.59 min and 52.04 min in DEX and control group respectively ().
Table 1 Demographic data in both groups of the study.
3.1 BIS and heamodynamics
There was no significant difference between the two groups of the study regarding BIS values at the base line, while BIS was significantly lower in DEX group at other time intervals till the end of surgery (p value < 0.05) ().
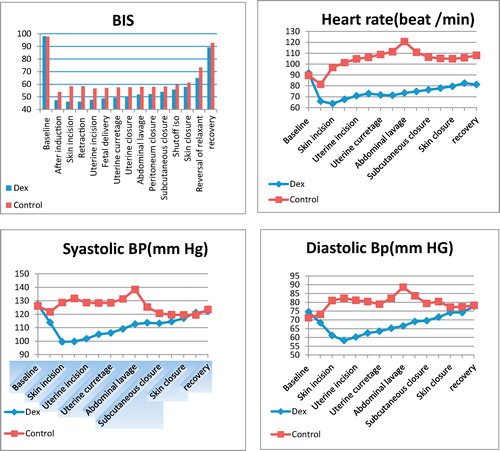
There was no significant difference between the two groups of the study regarding systolic blood pressure at the base line, shutoff Isoflurane, skin closure, reversal of muscle relaxant and at the recovery from anesthesia (p value > 0.05) while systolic blood pressure was significantly lower in DEX group at other time intervals (p value < 0.05). Also diastolic blood pressure values in the two groups were comparable at the base line, skin closure, reversal of muscle relaxant and at the recovery while being significantly lower in DEX group at other time intervals (p value < 0.05). There was no significant difference between the two groups of the study regarding heart rate at the base line, while it was significantly lower in DEX group at other time intervals till the end of surgery (p value < 0.05). Systolic blood pressure, Diastolic blood pressure and Heart rate were noted to be more elevated at the abdominal lavage time point more than 20% of the baseline values ().
3.2 MAC of isoflurane
MAC values in Dex group were significantly lower than the control group at most different time intervals (p value < 0.05) but there were no significant difference between them after induction, shutoff Isoflurane and at skin closure time points ().
Table 2 MAC of Isoflurane at different time intervals.
3.3 Neonatal outcome
Both groups of the study were matched as regard as Apgar score at 1 min and 5 min (p value > 0.05). Apgar score was 5.6 and 5.2 in DEX and control group respectively at 1 min as well as it was 9 and 8.8 in DEX and control group respectively at 5 min ().
Table 3 Apgar score in both groups of the study at 1 min and 5 min.
3.4 Post-recovery maternal monitoring
Alderete score values in DEX group were significantly lower than the control group 15 min after extubation (p value < 0.05). However, both groups were matched regarding Alderete score 30 min after extubation (p value > 0.05). Alderete score was 7.8 and 9.5 in Dex and control group respectively at 15 min after extubation but it was 10 in both groups of the study at 30 min after extubation ().
Table 4 Alderete score, sedation score and postoperative analgesic needs of the two study groups at post anesthetic care unit (PACU).
Sedation score values in Dex group were significantly higher than the control group at 5 and 15 min postoperatively (p value < 0.05). However, both groups were matched at 30 and 45 min (p value > 0.05). At 5 mints after extubation, 12 patients in DEX group were awake but drowsy and 10 patients were asleep but responsive to verbal commands while in the control group 17 patients were completely awake and 5 patients were awake but drowsy at 15 min post-extubation 22 patient in DEX group were awake but drowsy, on the other hand all patients in the control group were completely awake. All patients in both groups were completely awake at 30 and 45 min post-extubation ().
10 patients in the control group needed extra dose of fentanyl which were taken once at the abdominal lavage time point, but no one in the DEX group needed extra doses of fentanyl with statistically significant difference between both groups (p value < 0.05) ().
After 6 h from delivery, patients were asked for any recall or awareness but none of them were aware.
Surgeons were not satisfied about the degree of uterine contraction in 4 patients in the control group and requested additional dose of ecbolics.10 IU of oxytocin were given with marked improvement. On the other hand, other patients in both groups of the study did not need extradoses of ecbolic drugs.
4 Discussion
Successful anesthesia is a balance between the amounts of anesthetics given for the patients and their arousal state. Critical imbalances between anesthetic requirement and actually administered anesthetics may result in either light plane of anesthesia or marked depth of anesthesia leading to poor outcome [Citation14]. Awareness ranges from 0.13 to 17% among patients undergoing CS under general anesthesia [Citation15,Citation16]. Several studies reported that DEX is a useful adjuvant during general anesthesia as it has various advantages like hemodynamic stability, cerebral, cardiac, and renal protection [Citation17,Citation18].
Our primary outcome was evaluation of the effect of intraoperative dexmedetomidine infusion on BIS values during general anesthesia for CS. We found no significant difference between the two groups of the study regarding BIS values at the base line, while BIS was significantly lower in DEX group at other time intervals till the end of surgery. Similarly, Andreas et al. [Citation19] showed that DEX reduced propofol requirements and ensures hemodynamic stability during ICU sedation with BIS guidance. In addition, Simmons et al. [Citation20] showed that the revised Sedation-Agitation Scale and BIS work well to describe the depth of sedation for ventilated ICU patients. Also, Ghodki et al. [Citation21] showed that DEX is an effective anesthetic adjuvant which can be used in laparoscopy without fear of awareness. Other outcomes were evaluation of the effect of DEX infusion on hemodynamics, MAC of isoflurane, apgar score, sedation score and alderete score.
DEX was found to improve hemodynamic responses to surgical stimulation.
Blood pressure and heart rate were significantly controlled in DEX group at most of time intervals during surgery. In contrast to DEX group, 10 patients in the control group received single extra fentanyl dose at abdominal lavage time interval as there was increased heart rate and blood pressure more than 20% of the baseline.
Mahrous [Citation22] compared the effect of using DEX in a dose of 0.4 μg/kg/h intravenous infusion started from induction till peritoneum closure to the effect of fentanyl bolus on hemodynamic responses in pre-eclamptic patients undergoing elective CS under general anesthesia and showed a significant hemodynamic stability.
In addition, Abu-Halaweh et al. [Citation10] used intravenous DEX infusion for analgesia during normal labour in pre-eclamptic patients and found that DEX has asignificant blood pressure control.
El Tahan et al. [Citation23] compared different concentrations of DEX and placebo in CS and they found that its pre-operative administration in a dose of 0.4 and 0.6 μg/kg attenuates maternal hemodynamic and hormonal responses to surgery.
Moreover, Hall et al. [Citation24] reported a reduction in heart rate without change in mean arterial pressure when he used DEX intravenous infusion in his study about “sedative, Amnestic and Analgesic properties of small dose DEX infusion”.
Similarly, Talkeel et al. [Citation25] showed that patients given intravenous infusion of dexmedetomidine at adose of 0.8 μg /kg showed less increase in heart rate and noradrenaline levels during vascular surgery. While Yildiz et al. [Citation26] reported that a single preoperative dose of DEX resulted in increased sedation, blunted haemodynamic responses to laryngoscopy, and decreased opioid needs.
In addition, Ozkose et al. [Citation27] demonstrated that a single dose of 1 μg kg−1 h−1 DEX decreased hemodynamic response to intubation, reduced anesthetic and analgesic requirements, shortened recovery times, and decreased postoperative pain scores.
Kianpour et al. [Citation18] reported that intraoperative Dex infusion during bariatric surgery leads to decreased need for fentanyl use, and shortens the length of stay in the recovery room.
In the current study, DEX has been found to decrease the required MAC of isoflurane. This is consistent to what was found by Fragen, and Fitzgerald [Citation28]. They reported that Dexmedetomidine 0.7 ng/ml blood concentration decreased the required MAC of sevoflurane by about 17% in adults undergoing elective surgery. Similarly, Aantaa et al. [Citation29] found that use of DEX reduced the MAC of isoflurane in female patients undergoing abdominal hysterectomies.
As regard the neonatal parameters, our study showed no difference between Dex and control groups in Apgar score at 1 and 5 min. It was also recorded in the entire previous studies that dexmedetomidine can be used safely in parturients with no effect on neonatal Apgar score [Citation30,Citation31].
Similar studies done by, Mahrous [Citation22] and Abu-Halaweh et al. [Citation10] using DEX as an adjuvant during CS delivery and normal labour for pre-eclamptic mothers respectively showed maternal blood pressure control without any maternal or neonatal hazard.
As regards sedation and recovery scores, the current study showed that alderete score values in Dex group were significantly lower than the control group 15 min after extubation. Also, DEX has a good sedative effect for the 1st post-recovery 15 min.
Zaynelogulo at al. [Citation12] showed that DEX causes longer recovery time than a combination of midazolam and fentanyl when used for outpatient extracorporeal shock wave lithotripsy.
Similarly, Ohtani at al. [Citation32] stated that DEX infusion in a dose of 0.4 μg/kg/h may cause delayed recovery when given as an additive to propofol during TIVA in patients undergoing lower abdominal surgery, while Kim et al. [Citation33] showed that intraoperative DEX infusion at a dose 0.4 μg kg−1 h−1 till extubation reduced incidence of emergence agitation phenomenon in patients undergoing nasal surgery without delaying extubation.
In addition, Sarada et al. [Citation34] found that single dose of DEX 0.5 μg/kg given 5 min before extubation reduces the hemodynamic responses and airway reflexes during emergence from anaesthesia without causing excessive sedation.
The limitation of this study is that different doses of DEX should be studied rather than a fixed dose as it is known that the effect of DEX on blood pressure and heart rate is dose dependent.
Surgeons were satisfied about the uterine contraction in all DEX group patients. We think this can be explained by the fact that DEX has ecbolic effect and also due to decreased MAC requirement in the study group.
In conclusion, Dexmedetomidine is useful adjuvant during general anesthesia for CS as it attenuates hemodynamic responses to surgical stress, reduces needs for analgesic and anesthetic drugs together with favorable maternal and neonatal outcome.
5 Contributions
| 1. | Emad Eldeen A. Ibrahim, MD: This author helped in the conception and design of the study, revising the article critically for important intellectual content, and final approval of the version to be submitted. | ||||
| 2. | Mokhtar M. Amer, MD: This author helped in analysis and interpretation of data and Manuscript editing. | ||||
| 3. | Mohamed E. Abuelnaga, MD: This author helped in acquisition of data analysis, interpretation of data and drafting the article. | ||||
| 4. | Wafaa I. Abd -Elaal, MBBch: This author helped in Literature search, Clinical studies and acquisition of data. | ||||
6 Declarations of interest
None.
Acknowledgements
We would like to thank every participant patient in our work. Deep thanks for our colleagues and nursing staff in Suez Canal university hospital.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
This study was approved by Suez Canal University's Institutional full Board committee (research #2859) on 28 June 2016 and written informed consent was obtained from all subjects participating in the trial. The trial was registered at Pan African Clinical Trial Registry (http://www.pactr.org) database (PACTR201802003114191, Date of registration: 26 February 2018). This manuscript adheres to the applicable CONSORT guidelines. This randomized blind clinical trial was registered on Pan African Clinical Trial Registry (www.pactr.org) database, with a trial ID (PACTR201802003114191).
References
- S.E.RampersadM.F.MulroyA case of awareness despite an adequate depth of anesthesia as indicated by a Bispectral Index® monitorAnesth Analg1005200513631364
- Grover V, Bharti N. Measuring depth of anaesthesia-an overview on the currently available monitoring systems. In: The Indian Anaesthetists' Forum; 2008.
- S.M.R.HadaviE.AllahyaryS.AsadiEvaluation of the adequacy of general anesthesia in cesarean section by bispectral indexIran J Med Sci3832013240
- K.ChinS.YeoA BIS-guided study of sevoflurane requirements for adequate depth of anaesthesia in Caesarean sectionAnaesthesia5911200410641068
- C.J.KalkmanJ.C.DrummondMonitors of depth of anesthesia, quo vadis?Anesthesiology9642002784787
- K.RobinsG.LyonsIntraoperative awareness during general anesthesia for cesarean deliveryAnesth Analg10932009886890
- A.L.ChungD.Y.KimH.S.LeeThe effect of using sevoflurane for cesarean section on the bispectral index (BIS) and on neonatesKor J Anesthesiol4722004188191
- A.GrewalDexmedetomidine: new avenuesJ Anaesthesiol Clin Pharmacol2732011297
- M.ShukryJ.A.MillerUpdate on dexmedetomidine: use in nonintubated patients requiring sedation for surgical proceduresTher Clin Risk Manage62010111
- S.A.Abu-HalawehA.-K.S.Al OweidiH.Abu-MaloohIntravenous dexmedetomidine infusion for labour analgesia in patient with preeclampsiaEur J Anaesthesiol26120098687
- W.-S.KangS.-Y.KimJ.-C.SonThe effect of dexmedetomidine on the adjuvant propofol requirement and intraoperative hemodynamics during remifentanil-based anesthesiaKorean J Anesthesiol6222012113118
- P.ZeynelogluA.PiratS.CandanS.KuyumcuI.TekinG.ArslanDexmedetomidine causes prolonged recovery when compared with midazolam/fentanyl combination in outpatient shock wave lithotripsyEur J Anaesthesiol25122008961967
- H.W.ShinH.N.YooD.H.KimH.LeeH.J.ShinH.W.LeePreanesthetic dexmedetomidine 1 µg/kg single infusion is a simple, easy, and economic adjuvant for general anesthesiaKorean J Anesthesiol6522013114120
- P.K.SinhaT.KoshyMonitoring devices for measuring the depth of anaesthesia-an overviewIndian J Anaesth5152007365
- P.S.SebelT.A.BowdleM.M.GhoneimThe incidence of awareness during anesthesia: a multicenter United States studyAnesth Analg9932004833839
- T.Al ZahraniO.IbraheimA.TurkistaniK.MazenBispectral index profile during general anaesthesia using nitrous oxide for lower segment caesarean deliveryInternet J Anesthesiol1012005
- C.ChrysostomouC.G.SchmittDexmedetomidine: sedation, analgesia and beyondExpert Opin Drug Metab Toxicol452008619627
- B.TufanogullariP.F.WhiteM.P.PeixotoDexmedetomidine infusion during laparoscopic bariatric surgery: the effect on recovery outcome variablesAnesth Analg1066200817411748
- A.E.TriltschM.WelteP.Von HomeyerBispectral index-guided sedation with dexmedetomidine in intensive care: a prospective, randomized, double blind, placebo-controlled phase II studyCrit Care Med305200210071014
- L.E.SimmonsR.R.RikerB.S.PratoG.L.FraserAssessing sedation during intensive care unit mechanical ventilation with the Bispectral Index and the Sedation-Agitation ScaleCrit Care Med278199914991504
- P.S.GhodkiS.K.ThombreS.P.SardesaiK.D.HarnagleDexmedetomidine as an anesthetic adjuvant in laparoscopic surgery: an observational study using entropy monitoringJ Anaesthesiol Clin Pharmacol2832012334
- R.S.MahrousStudy on the effect of dexmedetomidine in reducing hemodynamic responses to general anesthesia for elective cesarean section in patients with pre-eclampsiaRes Opin Anesth Intensive Care31201625
- M.El-TahanH.MowafiI.Al SheikhA.KhidrR.Al-JuhaimanEfficacy of dexmedetomidine in suppressing cardiovascular and hormonal responses to general anaesthesia for caesarean delivery: a dose–response studyInt J Obstet Anesth2132012222229
- J.E.HallT.D.UhrichJ.A.BarneyS.R.ArainT.J.EbertSedative, amnestic, and analgesic properties of small-dose dexmedetomidine infusionsAnesth Analg9032000699705
- P.TalkeR.ChenB.ThomasThe hemodynamic and adrenergic effects of perioperative dexmedetomidine infusion after vascular surgeryAnesth Analg9042000834839
- M.YildizA.TavlanS.TuncerR.ReisliA.YosunkayaS.OtelciogluEffect of dexmedetomidine on haemodynamic responses to laryngoscopy and intubationDrugs R D7120064352
- Z.OzkoseF.S.DemirK.PampalS.YardimHemodynamic and anesthetic advantages of dexmedetomidine, an α2-agonist, for surgery in prone positionTohoku J Exp Med21022006153160
- R.J.FragenP.C.FitzgeraldEffect of dexmedetomidine on the minimum alveolar concentration (MAC) of sevoflurane in adults age 55 to 70 yearsJ Clin Anesth1161999466470
- R.AantaaM.L.JaakolaA.KallioJ.KantoReduction of the minimum alveolar concentration of isoflurane by dexmedetomidineAnesthesiology865199710551060
- A.S.NairK.SriprakashDexmedetomidine in pregnancy: review of literature and possible useJ Obstet Anaesth Crit Care3120133
- V.J.M.MendozaDexmedetomidine as adjunct for analgesia in labor: a report of two casesRev Colomb Anestesiol40120127981
- N.OhtaniK.KidaK.ShojiY.YasuiE.MasakiRecovery profiles from dexmedetomidine as a general anesthetic adjuvant in patients undergoing lower abdominal surgeryAnesth Analg1076200818711874
- S.KimJ.KimJ.LeeB.SongB.KooEfficacy of intraoperative dexmedetomidine infusion on emergence agitation and quality of recovery after nasal surgerySurvey Anesthesiol5832014137
- S.D.VankayalapatiM.V.RamsaliS.DumpalaS.PasupuletiEffect of dexmedetomidine on haemodynamic and recovery responses during tracheal extubation: a randomized comparative studyJEMDS546201629802983