ABSTRACT
Background and objectives: Ideal analgesia following knee surgery is needed to encourage early rehabilitation, and to improve functional recovery. We studied the impacts of adductor canal block (ACB) versus fascia iliaca compartment block (FICB) using ultrasound guidance on postoperative analgesia, strength of quadriceps muscle and capability to mobilize following knee arthroscopy.
Methods: 100 patients scheduled for elective arthroscopic knee surgery were randomly allotted to receive either ACB or FICB using bupivacaine 0.25% with epinephrine (1:2,00,000) at the end of surgery. Visual analogue scale (VAS) was evaluated on admission to PACU, 2, 4, 6, 12, 18 and 24 h postoperative. The quadriceps muscle strength and mobilization ability were assessed at 6, 12, 18 and 24 h postoperative. The postoperative consumption of rescue analgesia and patient's satisfaction were documented.
Results: At 6, 12 and 18 h after block, the quadriceps muscle strength was significantly better in ACB group in comparison with FICB group (P < 0.05). The timed up and go test in ACB group was significantly faster than that of FICB at 6 h, 12 h and 18 h after block (P < 0.001, 95% CI; 25.30–38.22, 30.06–35.95 and 24.09–28.28 respectively). Visual Analogue Scale values, postoperative consumption of rescue analgesia and patient's satisfaction were insignificantly different between both groups.
Conclusions: ACB and FICB provided effective postoperative analgesia for patients experiencing arthroscopic anterior cruciate ligament reconstruction with patellar graft or medial meniscus surgery, with quadriceps muscle strength sparing and early ambulation in ACB patients.
Trial registration: Pan African Clinical Trial Registry identifier: PACTR201606001666108.
1 Introduction
Arthroscopic knee surgery alludes to a large diversity of surgical interventions of the knee, and various pain relieving regimens have been explored with a specific end goal to find the ideal analgesic modality for such procedures. Postoperative pain depends, among others, on the sort and degree of surgical intervention and it is thus challenging to foresee the reasonable regimen for every patient [Citation1].
The femoral nerve block (FNB) has been considered the backbone for post knee arthroscopy analgesia for a considerable length of time. Opposing to FNB, the adductor canal block (ACB) is mainly a sensory nerve block with possibility of preserving quadriceps muscle strength as well as mobilization ability [Citation2,Citation3].
Fascia iliaca compartment block (FICB) is an anterior thigh regional block through blockade of lumbar plexus [Citation4]. As confirmed by radiography, local anesthetics introduced posterior to the fascia iliaca diffuse into its internal layers to reach the following nerves; femoral, lateral femoral cutaneous, genitofemoral, and obturator [Citation5,Citation6].
The present study investigated the impacts of ultrasound-guided ACB versus ultrasound-guided FICB on postoperative analgesia, quadriceps muscle strength and ability to mobilize in patients scheduled for arthroscopic knee surgery.
2 Materials and methods
The present prospective double-blind randomized trial was performed; following approval of our Institutional Review Board (30912/05/16), registration in the Pan African Clinical Trial Registry (PACTR201606001666108) and patients’ informed consent, on adult patients (18–40 years old), with American Society of Anesthesiologists physical status (ASA) I-II scheduled for elective arthroscopic knee surgery for medial meniscus surgery or anterior cruciate ligament (ACL) reconstruction with patellar graft. The study convention, ACB, FICB and the Visual Analogue Scale (VAS) were elucidated to each patient preoperatively together with instructions on how to perform the timed up and go (TUG) test.
2.1 Exclusion criteria
Exclusion criteria included patient refusal, body mass index (BMI) >35 kg/m2, mental disorders, any local infection or unfavorable coagulation profile that may hinder regional anesthesia, known allergy to the study drug, pregnancy, drug or alcohol abuse, a daily intake of opioid analgesics, patients booked for ACL reconstruction by hamstring graft or pre-operative inability to perform the mobilization test (TUG test).
Patients were randomized through a PC produced randomization numbers into two groups using sealed opaque envelopes.
Group I: Ultrasound-guided ACB
Group II: Ultrasound-guided FICB
15 min before surgery, Intravenous (IV) midazolam 0.05 mg/kg was administered for patients’ premedication. Following the application of routine monitoring; 5 leads ECG, pulse oximetry, non-invasive blood pressure and capnography; IV propofol 2 mg/kg, fentanyl 1 μg/kg and cisatracurium 0.15 mg/kg were used for induction of general anesthesia and endotracheal tube insertion. Anesthesia was maintained with O2: air, isoflurane (1–1.2%), and mechanical ventilation was initiated and adjusted so that endtidal carbon dioxide is kept at 35–40 mmHg. At the end of the surgical procedure and under entire aseptic safety measures, the regional nerve block technique was done in all patients under ultrasound guidance utilizing high-frequency linear 13–6 MHz transducer (SonoScape SSI 6600- China) and 100 mm 20 gauge insulated needle (Visioplex, Vygon, France).
ACB group: Patients received ultrasound-guided ACB utilizing bupivacaine 0.25% (30 ml) with epinephrine (1: 2,00,000) and sham ultrasound guided FICB.
FICB group: Patients received ultrasound-guided FICB utilizing bupivacaine 0.25% (40 ml) with epinephrine (1: 2,00,000) and sham ultrasound guided ACB.
The studied local anesthetic solutions were prepared and regional nerve blocks were performed by an anesthesiologist who had no ensuing part in the study.
Neostigmine (0.05 mg/kg) and atropine (0.02 mg/kg) IV were used for neuromuscular block reversal and patients were extubated. All patients were admitted to Post Anesthesia Care Unit (PACU) where IV paracetamol (1 g) was administered every 6 h. Postoperative pain was surveyed over 24 h utilizing VAS, where zero score corresponds to no pain and 100 mm to the worst pain. A rescue analgesic of IV pethidine 20 mg was given to patients in both groups when VAS ≥ 40 mm at rest and the total consumption of postoperative rescue analgesia was recorded. Any adverse events such as nausea, vomiting, respiratory complications, shivering, pruritus or any block-related postoperative neurologic symptoms (persistent numbness or paresthesia, weakness, or nonsurgical pain in the operative extremity) were recorded. All measurements and study outcomes were assessed by another research anesthesiologist who was blinded to group assignment.
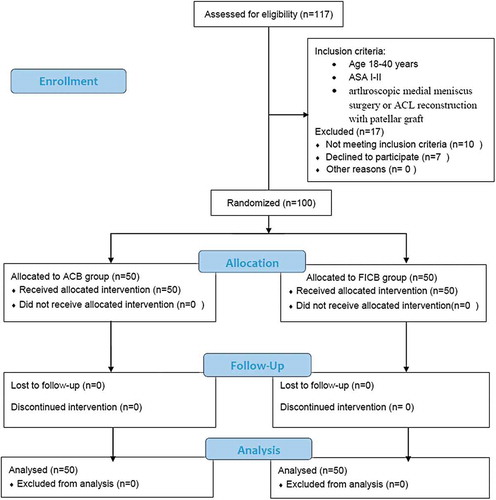
ACB [Citation1] : At the level of mid-thigh, halfway between the superior anterior iliac spine and the base of the patella, the ultrasound probe was positioned transversely, where the adductor canal is recognized through the representation of the sartorius muscle, the femoral artery, and vein. Recognizing the saphenous nerve, a hyperechoic structure situated lateral to the femoral artery, a 100 mm, 20 G needle was inserted using the in-plane technique through the sartorius muscle till the tip of the needle was in a position close to the saphenous nerve. Local anesthetic solution was incrementally injected in the adductor canal after initial aspiration followed by intermittent aspiration every 5 ml (.).
Fig. 1 Ultrasound guided demonstration of the adductor canal block: A and B: ultrasonographic anatomy of the adductor canal: FA (Femoral artery), FV (Femoral Vein), SN (Saphenous nerve), SM (Sartorius muscle), VM (Vastus Medialis). C and D: ACB: needle location indicated by arrows with local anesthetic (LA) deposited in the adductor canal.
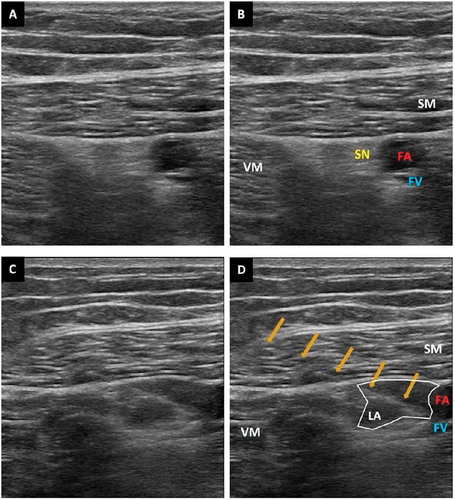
FICB [Citation7] : At the intersection of the lateral 1/3 and medial 2/3 of a line from the pubic tubercle to the anterior superior iliac spine, around 0.5–2 cm inferior to the inguinal ligament, the ultrasound probe was put in a transverse position where two fascial planes, the fascia lata and the fascia iliaca, were visualized as two hyperechoic lines. A 100 mm, 20G needle was inserted in a lateral-to-medial orientation aiming to puncture the fascia iliaca, where local anesthetic solution was injected in increments with intermittent aspiration every 5 ml ().
Fig. 2 Ultrasound guided demonstration of the fascia iliaca compartment block: A and B: ultrasonographic anatomy of the fascia iliaca compartment: FI (Fascia iliaca), FL (Fascia lata), FN (Femoral nerve), IPM (Iliopsoas muscle), FA (Femoral artery). C and D: ACB: needle location indicated by an arrow with local anesthetic (LA) deposited below the fascia iliaca.
Sham block: Using ultrasound guidance, a sham subcutaneous 0.5 ml sterile normal saline was injected at the FICB site and at the ACB site for the patients in ACB group and the patients in FICB group respectively.
2.2 Measurements
Primary outcome was the postoperative VAS score. The VAS was recorded immediately after transport to PACU, 2 h, 4 h, 6 h, 12 h, 18 h and 24 h postoperative.
Secondary outcomes included:
| • | The quadriceps muscle power was assessed with the patients in the supine position. They were requested to play out a straight leg raise. The quadriceps muscle power was assessed at 6, 12, 18 and 24 h after performing the block. The quadriceps motor power was assessed using the Medical Research Council (MRC) scale [Citation8] and was graded as follows: grade 0 = no voluntary contraction possible; grade 1 = muscle flicker, or trace of contraction but no movement of limb; grade 2 = active movement only with elimination of the gravity, grade 3 = active movement against gravity but without resistance; grade 4 = active movement against gravity with some resistance; and 5 = normal motor power against resistance. | ||||
| • | Mobilization ability was assessed with TUG test [Citation9] by measuring the time taken by the patient to get up from a chair, walk 3 m, turn, walk back to the chair, and sit down. All patients used an assisted aid in the form of a high walker with arm support while performing the test. Mobilization ability was assessed at 6, 12, 18 and 24 h after performing the block. This test was only done if the patient feels that he is capable of rising and walking without the risk of falling. | ||||
| • | Patient satisfaction was evaluated using a 3-point scale with 1 = satisfied, 2 = fair and 3 = unsatisfied. | ||||
2.3 Statistical analysis
Computation of the sample size relied upon the degree of the postoperative pain score. In light of the aftereffects of a past study [Citation10,Citation11]; assuming a 20 mm difference in the VAS score to be clinically significant and using SD of 24 mm; at least 40 patients were needed in each group at α error of 5% and study power of 95%. We recruited 50 patients in each group to avoid the dropout cases. We utilized SPSS 16 software (SPSS Inc., Chicago, IL, USA) for statistical analysis. Kolmogorov–Smirnov test was utilized to verify the assumption of normality. Quantitative data were portrayed as mean ± SD and independent sample t-test was utilized for comparison between both groups. The nonparametric data were presented as median and interquartile range. The grade of the quadriceps muscle power was analyzed using the Mann-Whitney test. Comparison of the continuous data within each group was carried out using repeated measures analysis of variance the Friedman test as appropriate. Categorical data were depicted as number or frequencies (%) and Chi-square or Fisher’s exact test were utilized as appropriate for comparison between both groups. P-value < 0.05 was considered significant.
3 Results
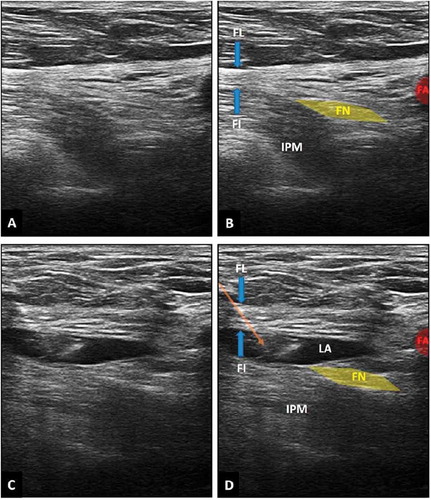
One hundred and seventeen patients were assessed for enrollment in this study. Ten patients didn’t match the inclusion criteria and 7 patients refused to participate in the research. In each group 50 patients were enrolled ().
Demographic data and type of surgery were comparable in both groups ().
Table 1. Demographic data and perioperative criteria of both groups.
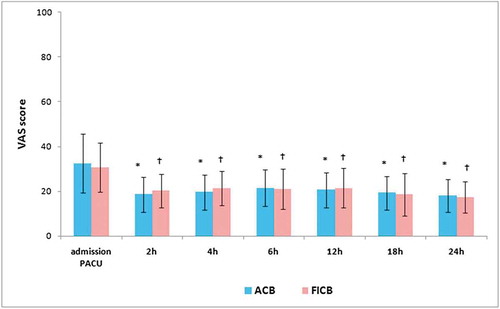
On admission to PACU, there was a statistically non-significant difference in the VAS score between ACB group (32.4 ± 13.2) and FICB group (30.6 ± 11.0) (P = 0.460, 95% confidence interval (CI); 03.01–06.61). All over the study time, VAS values showed statistically insignificant difference between ACB group and FICB group (P > 0.05). At 2 h postoperative and ongoing remaining times, the VAS values in both groups decreased significantly as compared to the VAS value on admission to PACU ().
Fig. 4 VAS changes in studied groups: * significant values in ACB group compared to the value on PACU admission. † significant values in FICB group compared to the value on PACU admission. Data presented as mean ± SD.
At 6, 12 and 18 h after performing the peripheral nerve blocks, the grade of quadriceps muscle strength was significantly better in ACB as compared to that in FICB (P < 0.001, 0.001, 0.037 respectively). However, that difference became statistically non-significant at 24 h (P = 0.608) ().
Table 2. The grade of the quadriceps muscle power in ACB and FICB.
The pre-operative values of the TUG test in both groups were comparable (8.55 ± 0.55 sec and 8.62 ± 0.48 sec) in ACB group and FICB respectively (P = 0.535). At 6 h after block, 41 patients in ACB group were able to perform the TUG test compared to only 15 patients in FICB (P < 0.001) (). The TUG test was faster in ACB group as compared to FICB at 6 h, 12 h and 18 h after block (P < 0.001, CI 25.3–38.22, 30.06–35.95, 24.09–28.28 respectively), while it became non significantly different at 24 h after block (P = 0.068) ().
Fig. 5 TUG test (sec) changes in both groups. * significant values between ACB and FICB groups. Data presented as mean ± SD.
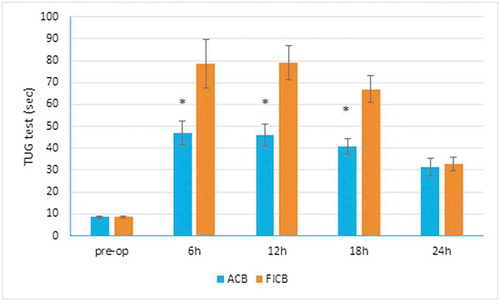
Table 3. Postoperative criteria in both groups.
5 patients in ACB group required rescue analgesia compared to 3 patients in FICB group (P = 0.715) ().
Patient's satisfaction was non significantly different between both groups (P = 0.202) ().
4 Discussion
Adequate analgesia following knee surgery is essential for prompt rehabilitation, refining functional recovery and diminishing postoperative morbidity [Citation12]. Postoperative nerve blocks provide tremendous analgesia for orthopedic surgery [Citation13].
The results of our research showed that, VAS and consumption of postoperative rescue analgesia throughout the 1st 24 postoperative were comparable between ACB and FICB groups. Along these lines, both ACB and FICB are effective in diminishing postoperative pain after arthroscopic knee surgeries. As respects the quadriceps muscle strength and the ambulation ability, both were better preserved in ACB as compared to FICB at 6 h, 12 h and 18 h postoperative. Notwithstanding the benefits of better conservation of quadriceps muscle strength and early ambulation, the utilization of small volume and dose of local anesthetic is another preferred standpoint of the ACB as compared to FICB. To our best of knowledge, our prospective double blinded study is the first study to compare the impacts of ACB and FICB on the postoperative pain relief, power of quadriceps muscle and mobilization capability in patients undergoing arthroscopic knee surgeries.
The adductor canal is situated between the adductor longus, vastus medialis and sartorius muscles in the mid-thigh [Citation14] navigated by different nerves; the saphenous nerve, nerve to the vastus medialis, posterior branch of the obturator nerve; and in some instances, the medial cutaneous nerve and anterior branch of the obturator nerve [Citation15]. All; apart from the nerve to the vastus medialis; participate in sensory innervation of the knee [Citation16]. In this way, ACB is more or less a sensory nerve block but may only affect the vastus medialisthus reducing the quadriceps muscle power in some patients, but with a restricted degree as contrasted to the FNB patients [Citation14]. Other conceivable reasons of reduced quadriceps muscle power in some patients included retrograde spread of local anesthetic solution prompting affection of the motor fibres of the femoral nerve [Citation13,Citation17], nerve compression or compartment syndrome, surgical trauma, or muscle injury [Citation17]. ACB has been archived to lessen quadriceps muscle power by about 8% as compared with placebo, however such decrease was not considered practically essential [Citation2].
In accordance with our outcomes as respects the effectiveness of ACB on reducing postoperative pain and preservation of the quadriceps muscle strength that permit early ambulation after knee surgery, Abdallah et al. [Citation18] in their study on 100 patients experienced ACL reconstruction, they presumed that ACB gave noninferior postoperative analgesia and in the meantime safeguarded quadriceps muscle strength as contrasted to FNB for outpatients experiencing ACL reconstruction. Kim et al. [Citation11] inferred that at 6–8 h postoperative, ACB patients had significant quadriceps strength saving impact when contrasted to FNB with as effective postoperative analgesia as FNB. While at 24 h and 48 h postoperative, the dynamometer results, pain scores, or opioid utilization were non significantly different between the both groups. El Ahl [Citation14] analyzed the impacts of ACB and FNB on postoperative pain and the quadriceps muscle strength in 120 patients experienced ACL reconstructions. He demonstrated that VAS in ACB group was insignificant different during the 1st 12 h postoperative but was significantly higher at 18 and 24 h as compared to FNB and with better preservation of quadriceps strength. The helpful effects of ACB on reducing postoperative pain and preserving the quadriceps muscle strength were demonstrated in other studies [Citation2,Citation3,Citation16,Citation18–Citation20].
Espelund et al. [Citation21] in their study on 50 adult patients underwent arthroscopic ACL reconstruction utilizing autologous tendon graft harvested from the semitendinosus muscle with or without semimembranosus or gracilis muscle accessory tendon graft. They inferred that no analgesic benefits were gotten when ACB was compared to placebo.
The FICB is a regional anesthetic technique where the local anesthetic solution is injected in a triangular-shaped space bounded anteriorly by the inner aspect of fascia iliaca, posteriorly by the iliacus muscle, medially by the vertebral column and upper part of the sacrum, and laterally by the inner lip of the iliac crest [Citation5,Citation6,Citation22,Citation23]. At the point when the local anesthetic is situated into this space, it distributes over the femoral, lateral femoral cutaneous, and obturator nerves, thereby making this block useful in patients experienced surgical procedures to the hip, femur and knee [Citation5,Citation6,Citation7,Citation22–Citation26].
Wallace et al. [Citation25] thought about the impacts of FICB and 3-in-1 block in 60 adult patients experienced knee Arthroscopy and meniscal repair and they found that the pain-relieving prerequisites and pain scores were not statistically significantly different between both groups and the onset of anesthesia was faster in the 3-in-1 block group but the duration of postoperative analgesia was longer with FICB. Farid et al. [Citation26] reasoned that FNB or FICB, followed by morphine patient-controlled analgesia (PCA), provided effective postoperative analgesia for ACL reconstruction. Morau et al. [Citation5] demonstrated insignificant difference in postoperative VAS score, opioid consumption between continuous 3-in-1 block group and continuous FICB group in patients scheduled for cruciate ligament repair or femur surgery however longer block performance time was recorded in the 3-in-1 block.
There are some limitations in our study; first, there was no control group as peripheral nerve blocks are used routinely in our institution as a part of multimodal analgesia for patients undergoing arthroscopic knee surgery. Secondly, we did not assess the sensory block as the peripheral nerve block was performed while the patient was anesthetized. Thirdly, we assessed postoperative pain during rest only. Fourth, we did not assess the time taken to perform each block.
5 Conclusions
ACB (30 ml bupivacaine 0.25% with 1: 2,00,000 epinephrine) and FICB (40 ml bupivacaine 0.25% with 1: 2,00,000 epinephrine) provided effective and satisfactory postoperative analgesia for patients undergoing arthroscopic ACL reconstruction with patellar graft or medial meniscus surgery without significant difference in side effects. ACB was associated with quadriceps muscle strength sparing and early ambulation compared to FICB.
Conflict of interest
The authors declare that there is no conflict of interest.
Meetings where the work has been presented
None.
Additional information
Funding
References
- Espelund M, Grevstad U, Jaeger P, Hölmich P, Kjeldsen L, Mathiesen O, et al. Adductor canal blockade for moderate to severe pain after arthroscopic knee surgery: a randomized controlled trial. Acta Anaesthesiol Scand 2014;85:1220–7.
- Jaeger P, Nielsen ZJ, Henningsen MH, Hilsted KL, Mathiesen O, Dahl JB. Adductor canal block versus femoral nerve block and quadriceps strength: a randomized, double blind, placebo-controlled, crossover study in healthy volunteers. Anesthesiology 2013;118:409–15.
- Kwofie MK, Shastri UD, Gadsden JC, Sinha SK, Abrams JH, Xu D, et al. The effects of ultrasound-guided adductor canal block versus femoral nerve block on quadriceps strength and fall risk: a blinded, randomized trial of volunteers. Reg Anesth Pain Med 2013;38:321–5.
- Mouzopoulos G, Vasiliadis G, Lasanianos N, Nikolaras G, Morakis E, Kaminaris M. Fascia iliaca block prophylaxis for hip fracture patients at risk for delirium: a randomized placebo-controlled study. J Orthop Traumatol 2009;10:127–33.
- Morau D, Lopez S, Biboulet P, Bernard N, Amar J, Capdevila X. Comparison of continuous 3-in-1 and fascia iliaca compartment blocks for postoperative analgesia: feasibility, catheter migration, distribution of sensory block, and analgesic efficacy. Reg Anesth Pain Med 2003;28:309–14.
- Capdevila X, Biboulet P, Bouregba M, Barthelet Y, Rubenovitch J, d‘Athis F. Comparison of the three-in-one and fascia iliaca compartment blocks in adults: clinical and radiographic analysis. Anesth Analg 1998;86:1039–44.
- Haines L, Dickman E, Ayvazyan S, Pearl M, Wu S, Rosenblum D, et al. Ultrasound guided fascia iliaca compartment block for hip fractures in the emergency department. J Emerg Med 2012;43:692–7.
- Compston A. Aids to the investigation of peripheral nerve injuries. Medical Research Council: Nerve Injuries Research Committee. His Majesty’s Stationery Office: 1942; pp. 48 (iii) and 74 figures and 7 diagrams; with aids to the examination of the peripheral nervous system. By Michael O’Brien for the Guarantors of Brain. Saunders Elsevier: 2010; pp. 64 and 94 Figures. Brain 2010;133:2838–44.
- Yeung TS, Wessel J, Stratford P, Macdermid J. Reliability, validity, and responsiveness of the lower extremity functional scale for inpatients of an orthopaedic rehabilitation ward. J Orthop Sports Phys Ther 2009;39:468–77.
- Newman B, McCarthy L, Thomas PW, May P, Layzell M, Horn K. A comparison of pre-operative nerve stimulator-guided femoral nerve block and fascia iliaca compartment block in patients with a femoral neck fracture. Anaesthesia 2013;68:899–903.
- Kim DH, Lin Y, Goytizolo EA, Kahn RL, Maalouf DB, Manohar A, et al. Adductor canal block versus femoral nerve block for total knee arthroplasty: a prospective, randomized, controlled trial. Anesthesiology 2014;120:540–50.
- Strassels SA, Chen C, Carr DB. Postoperative analgesia: economics, resource use, and patient satisfaction in an urban teaching hospital. Anesth Analg 2002;94:130–7.
- Chen J, Lesser JB, Hadzic A, Reiss W, Resta-Flarer F. Adductor canal block can result in motor block of the quadriceps muscle. Reg Anesth Pain Med 2014;39:170–1.
- El Ahl MS. Femoral nerve block versus adductor canal block for postoperative pain control after anterior cruciate ligament reconstruction: a randomized controlled double blind study. Saudi J Anaesth 2015;9:279–82.
- Lund J, Jenstrup MT, Jaeger P, Sorensen AM, Dahl JB. Continuous adductor canal blockade for adjuvant postoperative analgesia after major knee surgery: preliminary results. Acta Anaesthesiol Scand 2011;55:14–9.
- Jenstrup MT, Jæger P, Lund J, Fomsgaard JS, Bache S, Mathiesen O, et al. Effects of adductor-canal-blockade on pain and ambulation after total knee arthroplasty: a randomized study. Acta Anaesthesiol Scand 2012;56:357–64.
- Veal C, Auyong DB, Hanson NA, Allen CJ, Strodtbeck W. Delayed quadriceps weakness after continuous adductor canal block for total knee arthroplasty: a case report. Acta Anaesthesiol Scand 2014;58:362–4.
- Abdallah FW, Whelan DB, Chan VW, Prasad GA, Endersby RV, Theodoropolous J, et al. Adductor canal block provides noninferior analgesia and superior quadriceps strength compared with femoral nerve block in anterior cruciate ligament reconstruction. Anesthesiology 2016;124:1053–64.
- Jæger P, Zaric D, Fomsgaard JS, Hilsted KL, Bjerregaard J, Gyrn J, et al. Adductor canal block versus femoral nerve block for analgesia after total knee arthroplasty: a randomized, double-blind study. Reg Anesth Pain Med 2013;38:526–32.
- Chisholm MF, Bang H, Maalouf DB, Marcello D, Lotano MA, Marx RG, et al. Postoperative analgesia with saphenous block appears equivalent to femoral nerve block in ACL reconstruction. HSS J 2014;10:245–51.
- Espelund M, Fomsgaard JS, Haraszuk J, Mathiesen O, Dahl JB. Analgesic efficacy of ultrasound-guided adductor canal blockade after arthroscopic anterior cruciate ligament reconstruction: a randomised controlled trial. Eur J Anaesthesiol 2013;30:422–8.
- Dalens B, Vanneuville G, Tanguy A. Comparison of the fascia iliaca compartment block with the 3-in-1 block in children. Anesth Analg 1989;69:705–13.
- Wambold D, Carter C, Rosenberg AD. The fascia iliaca block for postoperative pain relief after knee surgery. Pain Pract 2001;1:274–7.
- Wathen JE, Gao D, Merritt G, Georgopoulos G, Battan FK. A randomized controlled trial comparing a fascia iliaca compartment nerve block to a traditional systemic analgesic for femur fractures in a pediatric emergency department. Ann Emerg Med 2007;50:162–71.
- Wallace JB, Andrade JA, Christensen JP, Osborne LA, Pellegrini JE. Comparison of fascia iliaca compartment block and 3-in-1 block in adults undergoing knee arthroscopy and meniscal repair. AANA J 2012;80:S37–44.
- Farid IS, Heiner EJ, Fleissner PR. Comparison of femoral nerve block and fascia iliaca block for analgesia following reconstructive knee surgery in adolescents. J Clin Anesth 2010;22:256–9.