Abstract
Central neurocytoma is a rare tumor of neuronal differentiation which is typically seen in young adults. Here, we report a case of a 25 years old female patient who presented with central neurocytoma of the third ventricle. Sub-total resection of the tumor was carried out via left parieto-occipital craniotomy. Afterwards, the patient received conventional radiotherapy (i.e., 54 Gy/27 fractions). We observed marked improvement in terms of tumor size reduction (i.e., from 5.2 × 4.8 cm2 to 3.4 × 2.1 cm2; ∼71%) and patient performance status.
Introduction
Central neurocytomas (CN) are rare tumors of neuronal differentiation which are typically seen in young adults. Such tumors when located within the ventricles of the brain are called intraventricular while those arising/present in the cerebral hemispheres and spinal cord are called extraventricular neurocytomas. Having a relatively good prognosis, early recognition of these tumors is crucial towards more favorable treatment outcomes. Radiological studies, in particular magnetic resonance imaging (MRI), provides the first step in diagnosis of these tumors [Citation1]. However, histopathology ascertains the definite diagnosis. The prominent features of these tumors have been elucidated [Citation2,Citation3] , which, among others, include: morphology comprising cells with uniform round contours, round nuclei with fine speckled chromatin, cell clusters with nuclear free fibrillary areas mimicking neurophil and delicate arborizing capillaries and foci of calcification. At the therapeutic end, total surgical resection is considered as the treatment of choice [Citation3Citation[4]–Citation5] ; nevertheless, radiotherapy [Citation3Citation[4]Citation[5]Citation[6]–Citation7] and chemotherapy are sometimes used in adjuvant settings [Citation3,Citation8,Citation9] , particularly when total resection is not possible.
Herein, we present a case of intraventricular neurocytoma (IVN), assess the response of our treatment protocol (i.e., sub-total tumor resection followed by conventional radiotherapy) and review the treatment options from the available literature. Specifically, we report a case of 25 years old female diagnosed with IVN. The patient showed marked improvement to sub-total tumor resection followed by radiotherapy.
Case report
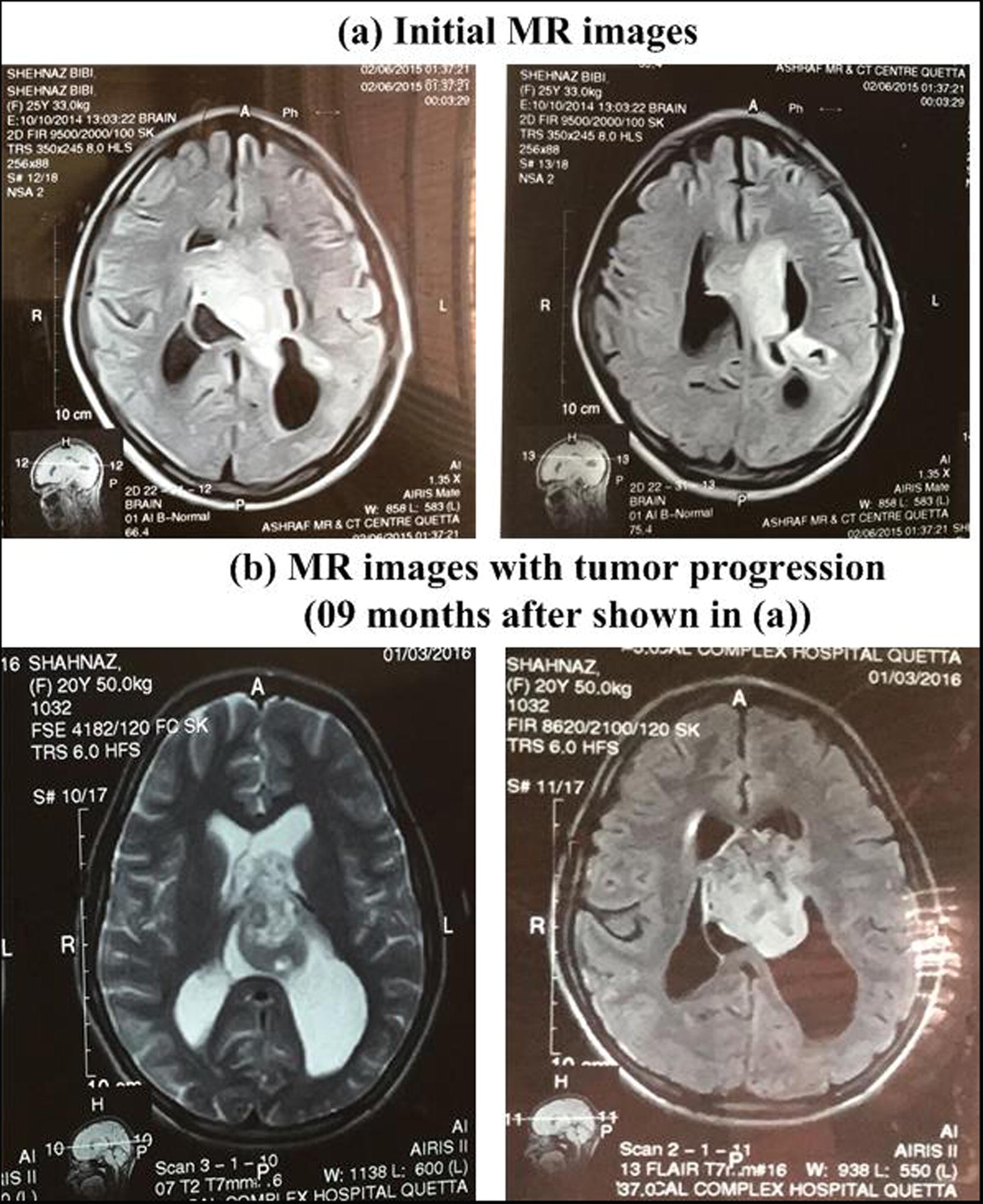
A 25-year-old female presented to the radiology department with the complaints of headache for three months duration. The patient was blind from both eyes. The Eastern Cooperative Oncology Group (ECOG) performance status of the patient was one at the time of presentation. Magnetic resonance (MR) images of the brain demonstrated tumor in the lateral ventricular region (). Specifically, MR images revealed moderately enhancing abnormal signal intensity area involving the septum pellucidum and affecting the anterior part of both lateral ventricles, as presented in . Moderate dilation of posterior parts of lateral ventricles was also noted. No further differential diagnostic or therapeutic work up was done for nine months, due to patient negligence. After nine months, the patient again presented to the radiology department; repeat MR study illustrated a large heterogeneously enhancing mass of size 5.1 × 3.8 cm2 in the midline region, with bulk of mass at the left. Specifically, the mass occupied the region of third ventricle. Further, mild communicating hydrocephalus was also noted. The mass also affected adjacent ventricles. However, posterior fossa of the brain stem was normal (). Sub-total resection of the tumor was implemented via left parieto-occipital craniotomy.
Fig. 1 Pre-treatment magnetic resonance (MR) images of the brain showing tumor in the lateral ventricular region. MR images with largest tumor size are shown only.
Histopathology revealed fragments of a neoplastic lesion (size = 2 × 1.5 cm2) composed of small to intermediate sized cells arranging in the form of sheets seen around arborizing blood vessels (). The individual neoplastic cells had scant cytoplasm and pleomorphic nuclei with open coarse chromatin showing few (approximately 1/10 HPF) mitoses. In foci, fibrillary nuclear free zones were seen. However, definite necrosis was not identified. Immunohistochemical stains showed following patterns; GFAP and EMA were negative, synaptophysin was diffuse positive and Ki 67 (Mib-1) was low. These features favored central neurocytoma, WHO grade II, according to WHO classification of central nervous system (CNS) neoplasms [Citation10]. The summary of clinical, radiological and histopathological features has been presented in .
Fig. 2 Illustrative histopathology and immunohistochemistry images; (a) Haematoxylin and Eosin (H&E) staining at 10× field showing prominent calcifications, (b) H&E staining at 40× field showing nuclear free fibrillary areas, and (c) Synaptophysin immunostain showing positive staining.

Table 1 Summary of clinical, radiological and histopathological features of 25-years old female patient having central neurocytoma of the third ventricle.
MR study after one month of craniotomy demonstrated evidence of mass (size = 5.2 × 4.8 cm2) in the septum pellucidum and frontal horn of third left lateral ventricle. It was isointense on T1 and intermediate signal on T2 and FLAIR images. Moreover, there was evidence of minimal dilatation of all the ventricles (). Re-surgery was refused by the surgeon at this stage.
Fig. 3 Post-treatment MR images of the brain showing reduced tumor in the lateral ventricular region. MR images with largest tumor size are shown only.
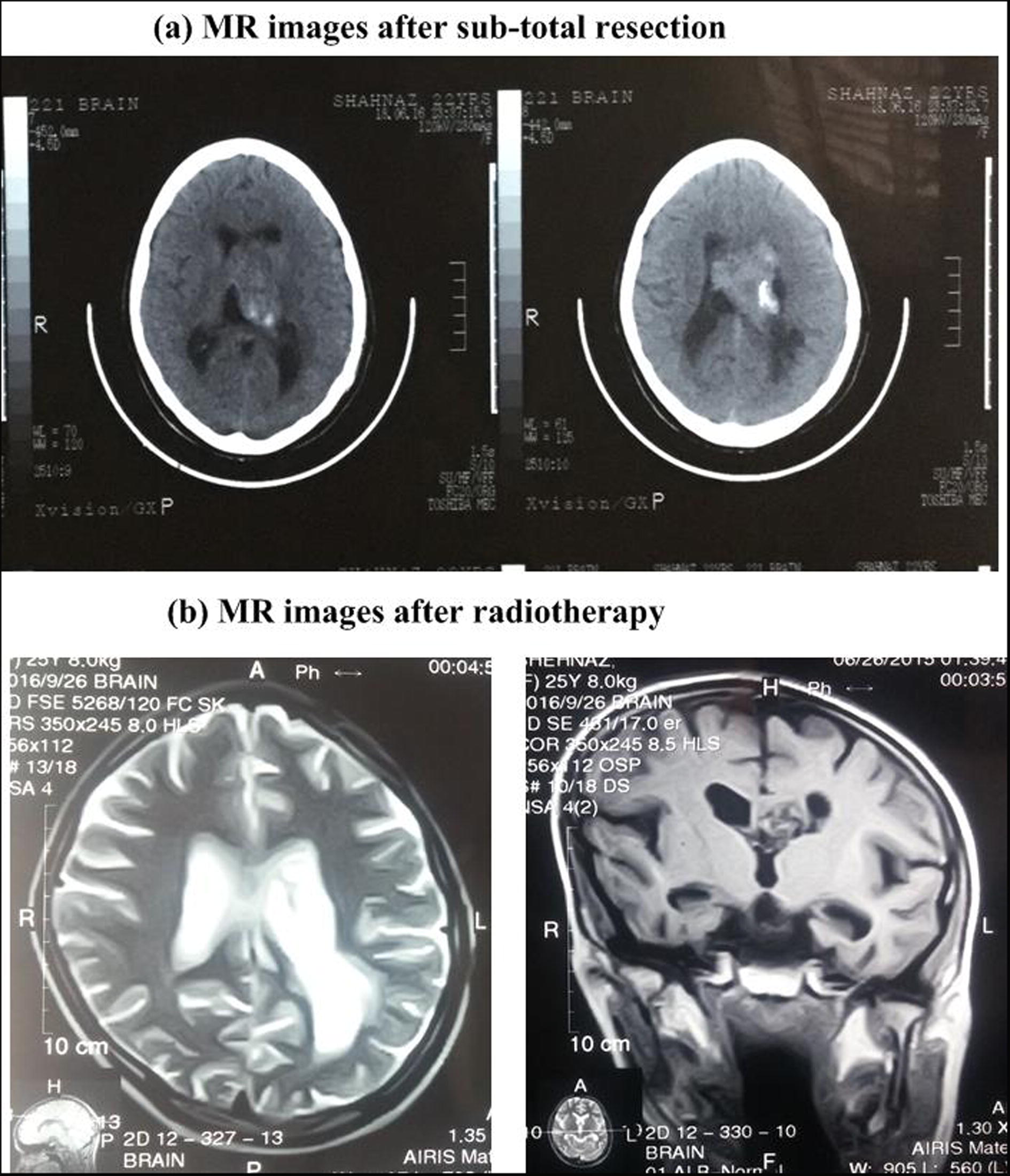
Conventional radiotherapy alone was decided at the therapeutic end. Specifically, 54 Gy in 27 fractions was delivered via two lateral opposing portals. Chemotherapy was not included in the treatment protocol. The tumor was re-assessed radiologically after three months of radiotherapy completion. Post-radiotherapy MR images illustrated mass in the frontal horn of left lateral ventricle with reduction in the size of tumor (size = 3.4 × 2.1 cm2; ∼71%). The patients have no complaints, including headache, and being kept on follow up. It may be of interest that the patient, after radiotherapy, was being pregnant and normally delivered a healthy twin recently.
Discussion
Neurocytoma is a group of rare brain tumors with characteristic indolent growth [Citation11], usually seen in adolescents and young adults. The typical clinical symptoms of neurocytomas include hydrocephalus, headache, vision problems, weakness, memory loss, nausea/vomiting, paresthesias, balance problems, decreased consciousness and occasional intraventricular hemorrhage [Citation3]; the first six symptoms were also presented by our patient.
The primary therapeutic option for neurocytoma tumors is the complete surgical resection (with minimal neurologic impairment) that markedly diminishes the chance of recurrence [Citation3]. Such resection essentially relives the intracranial pressure developed by the tumor and also restores cerebrospinal fluid (CSF) channels [Citation12]. However, the extent of surgical resection is typically defined by multiple parameters such as tumor size and location, invasion to surrounding critical structures, tumor vascularity, and expertize of the surgeon [Citation4]. In addition, typical IVN do not invade surrounding parenchyma, facilitating total tumor resection (TTR) particularly with microsurgical resection techniques such as transcortical- and transcallosal- transventricular approaches [Citation12,Citation13] . Indeed, TTR has been reported in one-third to one-half of patients [Citation14], which markedly increase the chance for local control of the tumor, as compared to sub-total resection (STR). For instance, three and five year local control for TTR was 95% and 85% against 55% and 46% for STR, respectively [Citation15]. Similar results have been found in other meta-analysis studies [Citation16]. Moreover, STR has been demonstrated as the only parameter associated with poor treatment outcomes. In our patient, STR of the tumor was performed, which might have delayed the improvement of patient status. Furthermore, minimally invasive approach based on endoscopic assisted total resection of central neurocytoma tumor has been successfully demonstrated. It is claimed that no further treatment was required; no residual or recurrent tumor was seen at 36-month follow-up [Citation17]. In summary, TTR remains the treatment of choice for neurocytomas and offers significantly (p < 0.001) superior outcomes compared to STR [Citation16].
Although the role of radiotherapy (RT) to the tumor bed after surgical resection has been debatable; nevertheless it has been implemented in many cases with the aim of preventing tumor progression and recurrence, particularly in patients with incomplete resection. Specifically, RT after STR improved local control (i.e., from 39% to 94%) and 10 years survival (i.e., from 82% to 100%) [Citation16]. Reduction in Mib-1 index from 5.6% to 0.2% has also been reported with RT (i.e., 58 Gy) [Citation18]. Moreover, various RT dose regimes for central neurocytoma after STR have been estimated [Citation19]. Specifically, the 5 years local control for equivalent dose in 2-Gy fractions was significantly (p = 0.0066) improved (98% vs. 69%) for higher doses (i.e., 54.0–62.2) as compared to lower doses (i.e., 40.0–53.6 Gy); at 10 years, the local control was 89% vs. 65%.
Most neurocytomas do not infiltrate the surrounding tissues; thereby necessitating RT to the tumor bed only, while the surrounding parenchyma should be spared. This would minimize the chance for radiations induced toxicities including necrosis (a factor suspected to correlated with radiation mortality) in the sensitive brain tissue [Citation20]. Previously, development of radiation induced anaplastic astrocytoma has been reported after 8 years of implementing STR followed RT for neurocytoma treatment [Citation21]. However, it has been suggested that radiation induced adverse effects can be minimized by limiting the dose below 60 Gy [Citation22]. Moreover, RT alone (i.e., without surgery and chemotherapy) has not been comprehensively assessed for treatment of neurocytomas; nevertheless, it may be offered to patients not fit for surgical resection or in case of non-availability of other treatment modalities [Citation23].
Stereotactic radiosurgery (SRS) has emerged as a potential treatment tool in the management of neurocytomas, due to its favorable features such as rapid dose fall-off and shorter treatment time, as compared to conventional RT [Citation24,Citation25] . SRS appear to offer superior results in terms of diminishing tumor recurrences and radiation-associated complications. Post-operative (i.e., STR) 5 years local tumor control was 100% with SRS as compared to 87% with conventional RT [Citation26]. Further, executing gamma knife radiosurgery in adjuvant setting, mean tumor volume reduction in 14 patients after mean follow up of 70 months was 69% (ranging from 47 to 87%) with no tumor progression [Citation7]. Moreover, linear accelerator based radiosurgery has revealed promising results. Specifically, residual lesion treated with this modality showed no evidence of recurrence for follow up of 51 months [Citation27]. Furthermore, it is noteworthy that the IVN’s offer an ideal location for SRS, presumably due to absorption of excess radiation by the CSF, minimizing radiation dose delivered to normal surrounding tissues [Citation28]. However, further studies with long term follow up are required as recurrences typically occur later in life [Citation29].
In addition to RT, chemotherapy has been used in a limited number of studies as adjunctive therapy to surgery [Citation8,Citation30,Citation31] . Chemotherapy is particularly advantageous in patients having large tumor bed where it can avoid the long-term radiation toxicity of large radiation fields [Citation31]. Although, the agreement on the optimal combination of chemotherapy agents seems scarce, reported studies have used various chemotherapy agents such as topotecan, carmustine, ifosfamide, prednisone, etoposide, carboplatin, lomustine, cyclophosphamide, vincristine, cisplatin, etc., [Citation13]. For instance, neurocytoma treated with (STR followed by) chemotherapy regime of PCV (i.e., procarbazine, CCNU, vincristine) remained stable for 16 months [Citation31]. Further, a patient with spinal cord drop metastasis from recurrent neurocytoma was treated with three cycles of chemotherapy (i.e., topotecan (0.5 mg/m2) and carboplatin (250 mg/m2) days 1–3; and ifosfamide (1,800 mg/m2) days 1–5, every 21 days); the patient showed complete response without severe complications [Citation9]. Nevertheless, further studies with large sample cohort are needed to compare various regimes of chemotherapy towards establishing any chemotherapy-specific recommendations in management of neurocytoma.
Conclusion
Neurocytoma is a rare tumor of neuronal differentiation which is typically seen in young adults. Herein, we presented a case of third ventricle neurocytoma. The patient showed marked improvement in terms of tumor size reduction (i.e., from 5.2 × 4.8 cm2 to 3.4 × 2.1 cm2; ∼71%) and patient performance status to the treatment protocol pertaining to sub-total resection of the tumor followed by conventional radiotherapy (i.e., 54 Gy/27 fractions). The available literature shows that total resection of the tumor remains the treatment of choice, offering the most favorable treatment outcomes. Radiotherapy, particularly radiosurgery, to the tumor bed has been used in tandem with sub-total resection (i.e., adjuvant setting). Chemotherapy seems to have limiting role in the management of neurocytomas.
Notes
✩ Source(s) of support in the form of grants, equipment, drugs, or all of these: None.
References
- C.-L.ChenC.ShenJ.WangC.LuH.LeeCentral neurocytoma: a clinical, radiological and pathological study of nine casesClin Neurol Neurosurg1102008129136
- Y.LiX.YeG.QianY.YinQ.PanPathologic features and clinical outcome of central neurocytoma: analysis of 15 casesChinese J Cancer Res2442012284290
- D.M.PatelR.F.SchmidtJ.K.LiuUpdate on the diagnosis, pathogenesis, and treatment strategies for central neurocytomaJ Clin Neurosci209201311931199
- K.A.ChoudhariC.KaliaperumalA.JainC.SarkarM.Y.S.SooD.Radeset al.Central neurocytoma: a multi-disciplinary reviewBr J Neurosurg2362009585595
- J.l..LeenstraF.J.RodriguezC.M.FrechetteC.GianniniS.l.StaffordB.E.PollockCentral neurocytoma: management recommendations based on a 35-year experienceInt J Radiat Oncol Biol Phys674200711451154
- H.ParkS.D.ChangStereotactic radiosurgery for central neurocytoma: a quantitative systematic reviewJ Neurooncol1082012115121
- M.ChenD.H.PanW.ChungK.LiuY.-S.YenM.-T.Chenet al.Gamma knife radiosurgery for central neurocytoma: retrospective analysis of fourteen cases with a median follow-up period of sixty-five monthsStereotact Funct Neurosurg892011185193
- D.BuchbinderM.DanielpourW.H.YongN.SalamonJ.LaskyTreatment of atypical central neurocytoma in a child with high dose chemotherapy and autologous stem cell rescueJ Neurooncol972010429437
- E.AminiT.RoffidalA.LeeG.N.FullerA.MahajanL.Ketonenet al.Central neurocytoma responsive to topotecan, ifosfamide, carboplatinPediatr Blood Cancer512008137140
- D.N.LouisA.PerryG.ReifenbergerDeimling A.VonD.Figarella-BrangerW.K.Caveneeet al.The 2016 World Health Organization classification of tumors of the central nervous system: a summaryActa Neuropathol13162016803820
- A.HallockB.HamiltonL.C.AngK.Y.TayJ.F.MeygesiB.J.Fisheret al.Neurocytomas: long-term experience of a single institutionJ Neurooncol1392011943949
- M.H.SchmidtO.N.GottfriedKoch.S.VonS.M.ChangM.W.McdermottCentral neurocytoma: a reviewJ Neurooncol662004377384
- M.C.SharmaP.DebS.SharmaC.SarkarNeurocytoma: a comprehensive reviewNeurosurg Rev292006270285
- A.BertalanffyK.RoesslerO.KoperekE.GelpiD.PrayerE.KnospRecurrent central neurocytomasCancer10412005135142
- D.RadesF.FehlauerTreatment options for central neurocytomaNeurology59200212681270
- D.RadesS.E.SchildTreatment recommendations for the various subgroups of neurocytomasJ Neurooncol772006305309
- A.RomanoS.ChibbaroO.MakieseM.MarsellaP.MaininiE.BenericettiEndoscopic removal of a central neurocytoma from the posterior third ventricleJ Clin Neurosci1622009312316
- T.FujimakiA.MatsunoT.SasakiT.ToyodaR.MatsuuraM.Ogaiet al.Proliferative activity of central neurocytoma: measurement of tumor volume doubling time, MIB-1 staining index and bromodeoxyuridine labeling indexJ Neurooncol321997103109
- D.RadesS.E.SchildK.IkezakiF.FehlauerDefining the optimal dose of radiation after incomplete resection of central neurocytomasInt J Radiat Oncol Biol Phys5522003373377
- S.E.SchildB.W.ScheithauerM.G.HaddockD.SchiffP.C.BurgerW.W.Wonget al.Central neurocytomasCancer7941997790795
- A.UtsunomiyaH.UenoharaS.SuzukiS.NishimuraA.NishinoH.Araiet al.Suzuki A case of anaplastic astrocytoma arising 8 years after initial treatment by partial resection and irradiation for central neurocytomaNo To Shinkei5382001747751
- D.RadesF.FehlauerK.LamszusS.E.SchildC.HagelM.Westphalet al.Well-differentiated neurocytoma: what is the best available treatment?J Neurooncol720057783
- V.KulkarniV.RajshekharR.P.HaranS.M.ChandiLong-term outcome in patients with central neurocytoma following stereotactic biopsy and radiation therapyBr J Neurosurg1622002126132
- E.Tyler-KabaraD.KondziolkaJ.C.FlickingerL.D.LunsfordStereotactic radiosurgery for residual neurocytomaJ Neurosurg952001879882
- C.-Y.KiS.H.PaekS.S.JeongH.-T.ChungJ.H.HanC.-K.Parket al.Gamma knife radiosurgery for central neurocytomaCancer11010200722762284
- D.RadesS.E.SchildValue of postoperative stereotactic radiosurgery and conventional radiotherapy for incompletely resected typical neurocytomasCancer1065200611401143
- D.G.KimS.H.PaekI.H.KimJ.G.ChiH.JungD.H.Hanet al.Central neurocytoma; the role of radiation therapy and long term outcomeCancer7910199719952002
- A.BertalanffyK.RoesslerW.DietrichM.AichholzerD.PrayerA.Ertlet al.Gamma knife radiosurgery of recurrent central neurocytomas : a preliminary reportJ Neurol Neurosurg Psychiatry702001489493
- D.J.CookS.D.ChristieR.J.B.MacaulayD.E.RheaumeR.O.HolnessFourth ventricular neurocytoma: case report and review of the literatureCan J Neurol Sci3142004558564
- A.A.BrandesP.AmistaM.GardimanL.VolpinD.DanieliB.Guglielmiet al.Chemotherapy in patients with recurrent and progressive central neurocytomaCancer8812000169174
- C.S.von KochM.H.SchmidtJ.H.Uyehara-lockM.S.BergerS.M.ChangThe role of PCV chemotherapy in the treatment of central neurocytoma: illustration of a case and review of the literatureSurg Neurol602003560565
