Abstract
Canarium odontophyllum (CO) (Miq.) (Burseraceae) has been traditionally consumed for its antioxidant benefit in maintaining longetivity. However, there is no report concerning its pharmacological activity on blood vessels. This study was aimed to investigate the effects of CO aqueous leaf extract on isolated aortic rings.
Methods Isolated thoracic aortic rings were suspended in a tissue bath and placed between 2 tungsten wires and connected to an isometric force transducer. The tension changes were recorded to a data acquisition system.
Results The leaf aqueous extract (3–15mg/ml) induced relaxation in endothelium-intact and endothelium-denuded aortic rings precontracted with PE. Incubation with nitric oxide enzyme inhibitor L-NAME, however, did not alter the CO-induced vasorelaxant on endothelium-intact aortic ring. The vasorelaxant effect of CO was endothelium-independent as it reduced the contraction induced by extracellular Ca2+ in endothelium-denuded aortic ring precontracted by PE and KCl in Ca2+-free Krebs solution. However, CO did not inhibit the release of intracellular Ca2+ from sarcoplasmic reticulum.
Conclusion This study suggests that the vasorelaxant effect of aqueous extract from CO leaves was endothelium-independent and was possibly mediated through the blockade of voltage-dependent calcium channel and receptor-operated calcium channel.
1 Introduction
According to World Health Organization (WHO), cardiovascular diseases such as coronary heart disease and ischemic heart disease are the leading cause of death worldwide in 2015 [Citation1] One of the risk factors of cardiovascular disease is arterial hypertension, which is also associated with other conditions such as myocardial infarction and stroke [Citation2]. Besides that, arterial hypertension is also found in metabolic diseases such as diabetes mellitus and obesity and in addition, smoking also often lead to cardiovascular pathology complication that involves vascular remodeling [Citation3,Citation4] . The prevalence of hypertension in Malaysia aged 18 years and above was 32.7%, and for aged 30 years and above was 43.5% in 2011 [Citation5].
With the increased risk of hypertension, researchers opt to seek for natural remedies from plant sources as they are a major source of phytochemical compounds with medicinal values. In the last 20 years, around 200 vasodilator compounds derived from plants have been identified such as resveratrol and quercetin [Citation6,Citation7] , as well as alkaloids, terpenoids and flavonoids [Citation8].
Canarium odontophyllum Miq. (CO) is a type of fruit that belongs to Burseraceae family which consists of 100 species well distributed throughout tropical Africa, Asia and Pacific Island [Citation9]. This fruit is classified as an under-utilized fruit due to lack of promotion and its economic potential has not been fully explored yet. The tree is found in the tropical rainforest of Sarawak [Citation10] and is locally known as ‘dabai’ or ‘Sibu olive’ in Sarawak and ‘kembayau’ in Sabah [Citation11]. The leaves were found to contain appreciable amount of flavonoid and terpenoid [Citation12] however, the type of terpenoid in the aqueous extract from C. odontophyllum leaves is still being investigated. It was suggested that among the many constituents of Gingko biloba leaves, terpenoid compounds contribute to the vasodilatory effect of G. biloba extract [Citation13]. To date, the effect of CO leaves on the changes of the vascular tone has not been studied yet. Therefore, this study was aimed to investigate for the first time, the vascular mechanisms involved in the vasorelaxant effect of leaf aqueous extract of Canarium odontophyllum using rat thoracic aorta.
2 Materials and methods
2.1 Drugs and reagents
Phenylephrine hydrochloride, acetylcholine chloride, NG-nitro-L-arginine methyl ester hydrochloride (L-NAME), potassium chloride (KCl) and ethylene diamine tetraacetic acid (EDTA) were bought from Sigma-Aldrich Inc., St. Louis, USA, while diltiazem hydrochloride was purchased from EMD Millipore Corp., USA. All the drugs were dissolved in distilled water.
2.2 Preparation of extract
The extraction method was based on previous study [Citation12]. In brief, fresh leaves of Canarium odontophyllum (CO) were collected from Miri, Sarawak, Malaysia and was identified by Mr. Sani Miran from the Herbarium of the Universiti Kebangsaan Malaysia (UKM), Bangi, Malaysia, Selangor with voucher specimen number of UKM 40052. CO leaves were washed and dried overnight then grinded using electrical blender. A total of 100 g of the leaves powder was then added with 500 ml of distilled and shaken at 100 rpm for 24 h by using an orbital shaker. The mixture was centrifuged at 3000 rpm for 5 min. The supernatant was collected and the process was repeated by adding 250 ml distilled water into the remaining residue. The supernatant was combined and freeze-dried at -50 °C under vacuum for 12 h to produce a fine crystal-like crude extract. The extract was kept in air-tight jar at 4 °C. Stock solution of the aqueous extract was prepared by dissolving 100 mg of extract in 1 ml of distilled water for experimental uses in this study. The dose selection ranging from 3.0 mg/ml to 15.0 mg/ml of CO extract were based on the observation of relaxation effect within the range.
2.3 Animals
In this study, 31 male Wistar rats weighing between 250 and 350 g were obtained from UKM Animal House. The rats were housed in plastic cages in controlled environment with 12 h light-dark cycle at 22 ± 5 °C and 40–60% humidity. The rats were fed with standard rat pellets and distilled water ad libitum. This study was approved by the Universiti Kebangsaan Malaysia Animal Ethical Committee (FSK/2015/DAYANG/11FEB-641-FEB-2015-JUNE-2017).
2.4 Preparation of isolated aortic rings
The rats were injected intraperitoneally with 1000 unit/ml/kg of heparin prior anaesthetised by using 1.5 g/kg urethane. Upon dissection, the descending thoracic aorta was isolated and placed in ice-cold Krebs-Henseleit solution with the following composition: NaCl (118 mM), NaHCO3 (25 mM), KCl (4.7 mM), KH2PO4 (1.2 mM), MgSO4·7H2O (1.2 mM), CaCl2·2H2O (2.5 mM) and glucose (11.7 mM) in a 1 L of dH2O. For Ca2+-free Krebs-Henseleit solution, the solution was prepared by excluding CaCl2·2H2O and adding EDTA (0.1 mM). The aorta was then cleared from any excess connective tissue and fat with extra care to avoid any damage to the luminal endothelium and then cut into small rings of 3–4 mm in length. For endothelium-independent experiment, the endothelium was removed mechanically by gently rubbing the luminal surface with a thin stainless steel wire before immersing it in the tissue bath chamber.
2.5 Vascular reactivity setup
The aortic rings were suspended between two stainless steel wires in the tissue bath chamber containing 10 ml of oxygenated Krebs solution (95% O2; 5% CO2) maintained at 37 °C. A passive tension of ∼1 g was applied to the rings and the change of tension in the aortic rings was measured isometrically by force transducer connected to PowerLab with Chart 5 software (ADInstrument, Australia). The aortic rings were allowed to equilibrate 45 min before addition of 120 mM of KCl to ensure the rings viability. Once the contraction stabilized and the tension reached a plateau, the aortic rings were precontracted with (0.1 μM) of phenylephrine (PE), an α1-adrenergic receptor agonist followed by (10 μM) acetylcholine (ACh), an endothelium-dependent vasorelaxant to assess the smooth muscle and endothelial integrity, respectively. Endothelium was considered to be intact when ACh caused >60% relaxation from the maximal contraction obtained in the aortic rings precontracted with PE [Citation14] while in endothelium-denuded rings, relaxation to acetylcholine was less than 10% [Citation15].
2.6 Effect of CO extract on endothelium-intact and endothelium-denuded aortic ring
An experiment was performed in both intact and denuded-endothelium aortic rings to investigate the dependence of CO vasorelaxation to the endothelium. The aortic rings were precontracted with (0.1 μM) PE and once PE-induced contraction had reached plateau, cumulative concentration of the extract ranging from 3 to 15 mg/ml were added to evaluate its relaxation effect on the aortic ring. The relaxant effect of the extract on the aortic rings was calculated as a percentage of the contraction in response to PE. The EC50 of CO obtained from the cumulative dose response curve would be used for further mechanistic investigation.
2.7 Involvement of nitric oxide synthesis pathway on CO vasorelaxation effect
Endothelium-intact aortic ring was preincubated with (100 μM) L-NAME for 20 min before contracted by PE (0.1 μM). Then the extract from 3 to 15 mg/ml was then added cumulatively. The relaxation effect of the extract on the aortic rings was compared with the control (without L-NAME incubation) to investigate the role of NO in the vasorelaxant effect of CO in the endothelium-intact aortic ring.
2.8 Involvement of extracellular Ca2+ on CO vasorelaxation effect
In order to determine whether the inhibition of extracellular Ca2+ influx was involved in extract-induced relaxation, the endothelium-denuded aortic ring contracted by 60 mM KCl (0.1 μM) PE after being incubated with the EC50 of the extract. The aortic ring was incubated in Ca2+-free Krebs solution in the presence of 0.1 M EDTA for 30 min to remove excess Ca2+ from the tissues. The control study was devoid of preincubation with the extract for 30 min. CaCl2 solution was then added cumulatively to a concentration from 0.3–10.0 mM to obtain a concentration-response curve. The contraction induced by KCl indicated that the influx of extracellular Ca2+ was through the voltage-dependent calcium channel (VDCC), whereas contraction induced by PE showed that the extracellular influx Ca2+ was through the receptor-operated calcium channel (ROCC). Then the contractile responses induced by CaCl2 in the presence and absence of extract were compared.
2.9 Involvement of intracellular Ca2+ release from sarcoplasmic reticulum on CO vasorelaxation effect
The endothelium-denuded aortic ring was preincubated with Ca2+ channel blocker, diltiazem, (1 μM 30 min) in normal Krebs solution to determine whether the relaxation induced by the extract was related to the inhibition of intracellular Ca2+ release. Diltiazem was used in this study as it is known to exert a relaxant effect on the rat and human vessels without a negative inotropic action on rat atria. Diltiazem has the advantage over other vasoselective Ca2+ channel blocker such as amlodipine as it does not activate the sympathetic nervous system and does not stimulate NO release from endothelial cells [Citation16]. Subsequently, PE at (0.1 μM) was then added to the bath to induce a steady contraction followed by the EC50 of CO extract.
2.10 Statistical analysis
All values were expressed as mean ± S.E.M and analysed with Two-way analysis of variance (ANOVA) using GraphPad Prism software version 6. Relaxant responses were normalized and expressed as percentage relaxation to maximal contraction induced by (0.1 μM) PE. Values of p <.05 were considered statistically significant.
3 Results
3.1 Vasorelaxation effect of CO extract
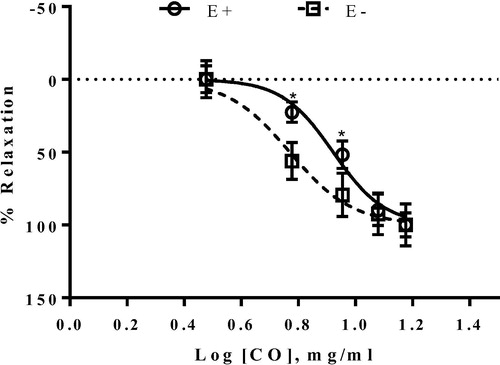
The result of Canarium odontophyllum (CO) leaf aqueous extract on PE-induced contraction in endothelium-intact and denuded aortic rings is presented in . The extract produced concentration-dependent relaxation in both aortic rings precontracted with (0.1 μM) PE. The maximal vasorelaxant effect for both treatment was normalized to 100%. The EC50 of the extract in the endothelium-denuded aortic ring was 5.89 mg/ml whereas for the endothelium intact aortic ring, the EC50 value was 8.36 mg/ml.
3.2 Vasorelaxant effect of CO extract was not mediated by nitric oxide synthesis pathway
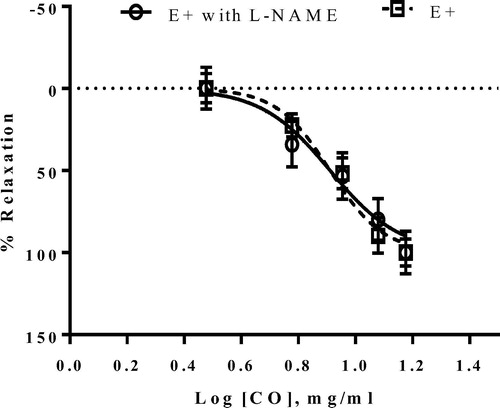
shows that the vasorelaxant activity of CO extract at the concentration above 9 mg/ml on the endothelium-intact aortic ring was not altered in the presence of L-NAME. This finding indicated that the relaxant response by the extract was not dependent on the nitric oxide released from the endothelium. There was no significant difference (p > 0.05) between the relaxation response of the extract with and without L-NAME-incubated aortic ring. The maximal relaxant effect in endothelium-intact aortic ring in L-NAME and control was normalized to 100%.
3.3 Vasorelaxant effect of CO extract was not mediated by the extracellular Ca2+-induced contraction
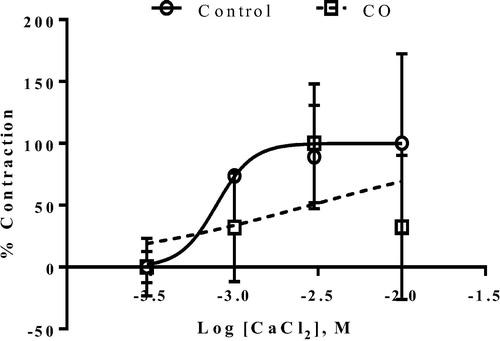
The concentration of the extract used to determine its inhibitory effect on the contraction induced by extracellular Ca2+ in endothelium-denuded ring precontracted with KCl and PE in Ca2+ free Krebs solution was based on the preliminary study on EC50 CO-induced relaxation in denuded preparation (5 mg/ml). As seen from Figs. 3(a) and 3(b) respectively, the vasocontraction responses to the cumulative concentration of Ca2+ showed no significant difference by the presence of CO in both KCl ((a)) and PE-precontracted ((b)) aortic rings compared to the control. The absence of attenuation of the contraction induced by the Ca2+ in the presence of CO incubation indicated that the extract mediated its vasorelaxation effect by mechanism not involving either VDCC (KCl-induced) and ROCC (PE-induced).
Fig. 3a Inhibitory effect of EC50 of CO on the extracellular Ca2+-induced contraction ranging from 0.3 mM to 10.0 mM in endothelium-denuded aortic ring precontracted by 60 mM KCl in Ca2+-free Krebs solution. Control group was not pre-incubated with CO. Values are expressed as mean ± S.E.M. where n = 4.
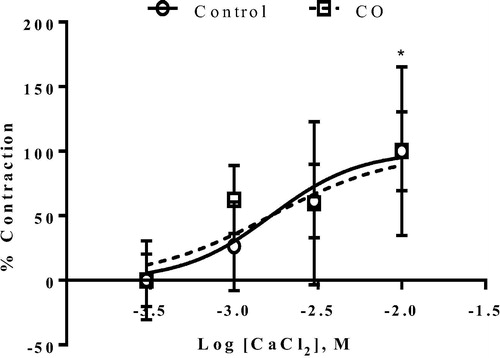
Fig. 3b Inhibitory effect of EC50 of CO at on the extracellular Ca2+-induced contraction at concentration from 0.3 mM to 10.0 mM in endothelium-denuded aortic ring precontracted by (0.1 μM) PE in Ca2+-free Krebs solution. Control group was not pre-incubated with CO. Values are expressed as mean ± S.E.M. where n = 4.
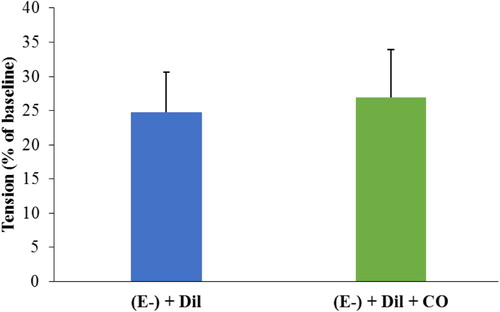
3.4 Vasorelaxant effect of CO extract was not mediated by intracellular Ca2+ release from sarcoplasmic reticulum
The result of CO extract on endothelium-denuded aortic rings incubated with diltiazem precontracted with PE shows that there was no significant difference (p > 0.05) in the contraction induced by PE before and after adding the extract (). This finding shows that the extract did not inhibit or decrease the release of the intracellular Ca2+ from the sarcoplasmic reticulum as PE was still able to produce vasoconstriction effect on the aortic ring despite adding the CO extract. However, since PE-induced contraction is not affected by the presence of Ca2+in the normal Krebs solution, the result with diltiazem which showed no changes in the vasospasm level indicates that this phenomenon has been eliminated prior to considering addition of CO extract.
Fig. 4 The effect of CO extract on the intracellular Ca2+ released by the sarcoplasmic reticulum. Endothelium-denuded aortic ring was incubated with diltiazem (1 μM) before addition of (0.1 μM) PE. The rings were then exposed to 4.95 mg/ml of CO extract. The tension produced by the ring was compared before and after the addition of the extract. Values are expressed as mean ± S.E.M. where n = 4.
4 Discussion
The present study reports the vasorelaxant action of the C. odontophyllum (CO) leaves extract on the aortic rings at the concentration ranging from 3 mg/ml to 15 mg/ml. The extract was able to induce concentration-dependent relaxation. The vasodilatory effect of CO was still the same even in the absence of endothelium suggesting that its mechanism does not involve the presence of endothelium-derived relaxing factor (EDRF) in vascular endothelium.
Vascular endothelium which is located between the circulating blood and vascular smooth muscle plays an important role in regulating the vascular tone. Modulation of vascular tone by endothelium is mediated by the release of vasodilators (NO and prostacyclin) and vasoconstrictors such as endothelin and angiotensin II [Citation17]. Relaxation in vascular smooth muscle can occur through the NO/cGMP pathway. In endothelial cell, the calcium-calmodulin complex stimulates NO synthase (NOS), which later activates NO formation from L-Arginine. NO then enters the smooth muscle cells and stimulates guanylate cyclase, which increases intracellular cyclic guanosine monophosphate (cGMP). The increased of the intracellular cGMP then stimulate cGMP dependent protein kinases leading to a decrease in the calcium concentrations in the smooth muscle cells, which causes its relaxation [Citation18].
The impairment of NO release may be held to account for abolishing the relaxant effect by CO as this extract also exhibited relaxation in endothelium-intact aortic ring. NG-nitro-L-arginine methyl ester (L-NAME), a non-selective nitric oxide inhibitor was used to confirm the involvement of endothelium-derived relaxing factor in the CO-induced vasorelaxation. However, pretreatment with L-NAME did not alter the vasorelaxant effect of CO leaves extract in endothelium-intact aortic ring suggesting that NO may not contribute to the CO-induced relaxation. This is in disagreement with report on Myrciaria cauliflora fruit [Citation19] Andrade and Tridax procumbens Lin. leaf [Citation20] which produced endothelium-dependent vasorelaxant activity through NO formation. The latter further confirmed that the vasorelaxant effect of Tridax procumbens involved mainly activation of NO-cGMP-cAMP pathways [Citation21].
Since the current study showed that endothelium denudation did not alter the vasorelaxant action of CO, the extract could have acted directly through the vascular smooth muscle activity. As Ca2+ is directly involved in the smooth muscle contraction, the effect of CO towards the Ca2+-induced contraction was evaluated. The mechanism involving the extract-induced relaxation in endothelium-denuded ring could be due to the inhibition of the Ca2+ channel. The Ca2+ influx through cell membrane occurs by voltage-dependent L-type calcium channel (VDCC) and receptor-operated calcium channel (ROCC) [Citation22,Citation23] . Calcium ions caused vasoconstriction dependently in Ca2+-free Krebs solution after addition of high KCl. High KCl depolarizes the smooth muscle cell membrane and opens voltage-gated Ca2+ channel, resulting in an influx of extracellular Ca2+, leading to vascular smooth muscle contraction [Citation24,Citation25] . Meanwhile, PE, an α1-adrenergic receptor agonist causes vascular smooth muscle contraction by Ca2+ influx through ROCC and also by the release of Ca2+ from the sarcoplasmic reticulum [Citation24]. Apparently, CO did not significantly reduced Ca2+- induced contraction activated by both PE and KCl suggesting that the vasorelaxant effect of the extract did not involved blockade of both VDCC and ROCC. This is in disagreement with the vasorelaxant activity of root and rhizoma from extract Ligusticum jeholense was reported to be mediated by blockade of extracellular Ca2+ influx through the receptor-operated Ca2+ channel and voltage-dependent calcium channel pathways [Citation26].
In order to evaluate the involvement of intracellular Ca2+ released from sarcoplasmic reticulum (SR) in the vasodilating effect of CO, endothelium-denuded aortic ring was incubated with diltiazem, an L-type Ca2+ channel blocker to prevent the influx of extracellular Ca2+. The extract did not appear to abolish the vasoconstriction effect of PE, indicating that CO did not inhibit or attenuate the intracellular Ca2+ released from the inositol triphosphate (IP3)-sensitive stores of SR in aortic rings. PE activates the α1-receptor leading to the production of dialcylglycerol and IP3. Inositol triphosphate then stimulates the release of Ca2+ from SR after activation of IP3 receptor [Citation27] leading to vascular smooth muscle contraction. This result contradicts with the study on the seed extract of Nigella sativa that its hypotensive effect occurred via inhibitory action on the release of intracellular Ca2+ stores from SR [Citation28].
As far as the role of calcium is concerned, inhibition of extracellular Ca2+ does not contribute to the mechanism of vasodilating action of aqueous extract from Canarium odontophyllum leaves by acting on both the VDCC and ROCC. Additionally, it also does not involve the inhibition of intracellular Ca2+ from the sarcoplasmic reticulum. It could be postulated that the terpenoid constituents in a mixture of CO leaves played a role in exerting the vasorelaxant effects. Recently, a considerable amount of natural compound high in flavanoid and terpenoid [Citation12] have been shown to exert vasodilating effect, at least in part, by activating K+ channel [Citation29,Citation30] . Therefore, it can be suggested that these compounds that are contained in CO extract may contribute to vasorelaxant effect via modulation of K+ channel. Given the diversity of the bioactive compound derived from CO extract and various mechanism of action responsible for vasodilation activity this warrant further investigation in searching for the mechanism involved in vasorelaxant by CO extract.
5 Conclusion
This data demonstrated for the first time that C. odontophyllum Miq. aqueous leaf extract is a vasorelaxant and its effect is not dependent on the nitric oxide released by the endothelium. The action was also not mediated via voltage-dependent Ca2+ channel (VDCC) and receptor-operated Ca2+ channel (ROCC), as the influx of extracellular Ca2+ through these channels into the smooth muscle cells was not inhibited. These findings may provide insight that involved other mechanism into the efficacy of the leaf extracts from Canarium odontophyllum as phytoalternative treatment for hypertension and other cardiovascular diseases.
Acknowledgement
This project was funded by Universiti Kebangsaan Malaysia under the Research University Grant Code Grant GUP-2014-059.
References
- World Health Organization (WHO). Geneva: Cardiovascular diseases (CVDs). Fact Sheet N°317. :c2017 [cited 2016 Apr 28]. Available from: http://www.who.int/mediacentre/factsheets/fs317/en/.
- Nguelefack TB, Dongmo AB, Dimo T, Kamanyi A. Phytopharmacology of some medicinal plants used in Cameroonian traditional medicine to handle cardiovascular diseases. In: Recent Developments in Medicinal Plants Research. Kerala: Research Signpost Publisher; 2007. p. 147–167.
- S.ZainalabidinS.B.BudinA.RamalingamY.C.LimAortic remodelling in chronic nicotine-administered ratKorean J Physiol Pharmacol82014411418
- A.MisraL.KhuranaObesity and the metabolic syndrome in developing countriesJ Clin Endocrinol Metab932008930
- Naing C, Yeoh PN, Wai VN, Win NN, Kuan LP, Aung K. Hypertension in Malaysia. An Analysis of trends from the National Surveys 1996 to 2011. Medicine (Baltimore), 95: Article ID e2417.
- G.AldiniM.CariniA.PiccoliG.RossoniR.M.FacinoProcyanidins from grape seeds protect endothelial cells from peroxynitrite damage and enhance endothelium-dependent relaxation in human artery: new evidences for cardio-protectionLife Sci73200328832898
- A.NovakovicL.BukaricaM.GojkovicD.PericB.NezicJ.Djukanovicet al.The mechanism of endothelium-independent relaxation induced by the wine polyphenol resveratrol in human internal mammary arteryJ Pharmacol Sci10120068590
- F.J.Luna-VázquezC.Ibarra-AlvaradoA.Rojas-MolinaI.Rojas-MolinaM.A.Zavala-SánchezVasodilator compounds derived from plants and their mechanisms of actionMolecules18201358145857
- H.P.ChuaD.NicholasDabai - speciality fruit of SarawakAgromedia3020092830
- K.L.ChaiA.W.A.DayangC.Y.LauS.L.SimControl of in vitro contamination of explants from field-grown dabai (Canarium odontophyllum Miq.) treesAsia Pac J Mol Biol Biotechnol182010115118
- S.H.Ali HassanJ.R.FryM.F.Abu BakarAntioxidative phytochemicals and anti-cholinesterase activity of native kembayau (Canarium odontophyllum) fruit of Sabah, Malaysian BorneoJ Nutr Food Sci4201316
- DFBasriKYHengKMChanARGhazaliScreening of antioxidant phytoextracts of Canarium odontophyllum (Miq.) leaves in vitroIOSR J Pharm4201416
- S.NishidaH.SatohComparative vasodilating actions among terpenoids and flavonoids contained in Ginkgo biloba extractClin Chim Acta3392004129133
- R.F.FurchgottP.D.CherryJ.V.ZawadzkiD.JothianandanEndothelial cells as mediators of vasodilation of arteriesJ Cardiovasc Pharmacol61984336343
- M.AjayH.J.ChaiA.M.MustafaA.H.GilaniM.R.MustafaMechanisms of the anti-hypertensive effect of Hibiscus sabdariffa L. calycesJ Ethnopharmacol1092007388393
- M.MotroJ.ShemeshE.GrossmanCoronary benefits of calcium antagonist therapy for patients with hypertensionCurr Opin Cardiol162001349355
- G.M.RubanyiThe role of endothelium in cardiovascular homeostasis and diseaseJ Cardiovasc Pharmacol221993114
- E.StankeviciusE.KevelaitisE.VainoriusU.SimonsesRole of nitric oxide and other endothelium-derived factorsMedicina (Kaunas)392003333341
- Andrade DM, Fatima Reis C, Silva Castro PF, Borges LL, Amaral NO, Torres IMS, Rezende SG, Souza Gil E, Conceicao EC, Pedrino GR, Rocha Ml. Vasorelaxant and hypotensive effects of jaboticaba fruit (Myrciaria cauliflora) extract in rats. Evid Based Complement Alternat Med; 2015:696135.
- H.M.SalahdeenG.O.IdowuB.A.MurtalaEndothelium-dependent and independent vasorelaxant effects of aqueous extraxt of Tridax procumbens Lin. leaf in rat aortic ringsIndian J Exp Biol502012883888
- H.M.SalahdeenG.O.IdowuS.A.SalamiB.A.MurtalaA.A.AladaMechanism of vasorelaxation induced by Tridax procumbens extract in rat thoracic aortaJ Intercult Ethnopharmacol52016174179
- G.P.ChenY.YeL.LiY.YangA.B.QianS.J.HuEndothelium-independent vasorelaxant effect of sodium ferulate on rat thoracic aortaLife Sci8420098188
- H.KarakiH.OzakiM.HoriM.Mitsui-SaitoK.AmanoK.Haradaet al.Calcium movements, distribution, and functions in smooth musclePharmacol Rev491997157230
- H.KarakiN.UrakawaP.KutskyPotassium-induced contraction in smooth muscleJ Smooth Muscle Res201984427434
- P.M.HudginsG.B.WeissDifferential effects of calcium removal upon vascular smooth muscle contraction induced by norepinephrine, histamine and potassiumJ Pharm Exp Ther15919689197
- I.McFadzeanA.GibsonThe developing relationship between receptor operated and store operated calcium channels in smooth muscleBritish J Pharmacol135200213
- B.KimK.LeeK.S.ChinannaiI.HamY.BuH.Kimet al.Endothelium-independent vasorelaxant effect of Ligusticum jeholense root and rhizome on rat thoracic aortaMolecules2020151072110733
- Niazmand S, Fereidouni E, Mahmoudabady M, Mousavi SM. Endothelium-independent vasorelaxant effects of hydroalcoholic extract from Nigella sativa seed in rat aorta: the roles of Ca2+ and K+ channels. BioMed Res Int; 2014:247054.
- X.-M.ZhuL.-H.FangY.-J.LiG.-H.DuEndothelium-dependent and-independent relaxation induced by pinocembrin in rat aortic ringsVascul Pharmacol4632007160165
- C.R.TirapelliS.R.AmbrosioF.B.da CostaS.T.CoutinhoD.C.de OliveiraA.M.de OliveiraAnalysis of the mechanisms underlying the vasorelaxant action of kaurenoic acid in the isolated rat aortaEur J Pharmacol49222004233241