Abstract
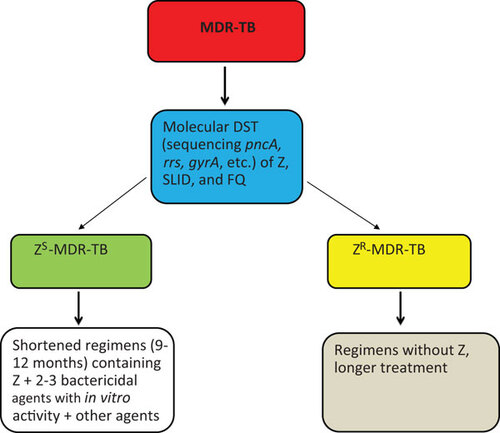
Indispensable for shortening treatment of drug-susceptible tuberculosis (TB), pyrazinamide (PZA, Z) is also essential in the treatment of multidrug-resistant (MDR)-TB. While resistance to PZA in MDR-TB is associated with poor treatment outcome, bacillary susceptibility to PZA along with the use of fluoroquinolone (FQ) and second-line injectable drugs (SLIDs) may predict improved treatment success in MDR-TB. Despite a high prevalence of PZA resistance among MDR-TB patients (10%–85%), PZA susceptibility testing is seldom performed because of technical challenges. To improve treatment of MDR-TB, we propose to: (i) classify MDR-TB into PZA-susceptible MDR-TB (ZS-MDR-TB) and PZA-resistant MDR-TB (ZR-MDR-TB); (ii) use molecular tests such as DNA sequencing (pncA, gyrA, rrs, etc.) to rapidly identify ZS-MDR-TB versus ZR-MDR-TB and susceptibility profile for FQ and SLID; (iii) refrain from using PZA in ZR-MDR-TB; and (iv) explore the feasibility of shortening the treatment duration of ZS-MDR-TB with a regimen comprising PZA plus at least two bactericidal agents especially new agents like TMC207 or PA-824 or delamanid which the bacilli are susceptible to, with one or two other agents. These measures may potentially shorten therapy, save costs, and reduce side effects of MDR-TB treatment.
Drug-resistant tuberculosis (TB), especially multidrug-resistant TB (MDR-TB), defined by bacillary resistance to at least isoniazid (INH) and rifampin (RIF), and extensively drug-resistant TB (XDR-TB), poses an increasing challenge for TB control.Citation1 XDR-TB refers to MDR-TB with additional bacillary resistance to fluoroquinolones (FQs) and one or more of the three second-line injectable drugs (SLIDs)—kanamycin, amikacin and capreomycin. WHO estimates that 500 000 MDR-TB cases occur every year.Citation1 Treatment of MDR-TB is difficult with an average cure rate of only around 62% in the best clinics.Citation2 In addition, the recommended treatment duration of MDR-TB, which is at least 18–24 months, is expensive and toxic in a substantial proportion of patients.
Unique role of PZA in the treatment of TB and MDR-TB
Pyrazinamide (PZA) plays a unique role in modern TB chemotherapy.Citation3 Inclusion of PZA enables considerable shortening of the treatment period from the previously 9–12 months to 6 months, thus the drug plays a pivotal role in the current short-course chemotherapy for drug susceptible TB.Citation4 The powerful sterilizing activity of PZA is due to its ability to kill a population of persister tubercle bacilli that are not killed by other TB drugs.Citation4 Studies in the mouse model of TB showed that substitution of PZA, but not INH and RIF, invariably led to poorer treatment outcomes.Citation5,Citation6,Citation7 Furthermore, the synergistic activity of PZA with newly developed agents such as the diarylquinoline bedaquiline suggests that the use of PZA in regimens including novel agents could improve efficacy substantially, if the organism retains susceptibility to PZA.Citation8,Citation9
Feasibility of establishing a simple and shortened treatment regimen for PZA-susceptible MDR-TB
There is fairly good evidence from animal and human studies that the treatment duration of ZS-MDR-TB can be shortened to a minimum of 9 months with a regimen comprising PZA accompanied by two bactericidal drugs. McCune et al.Citation10,Citation11 demonstrated in the mouse model that murine TB could be better sterilized with PZA plus a companion drug, especially a bactericidal one. In the treatment of drug-susceptible TB, the 2-year relapse rates of 9-month regimens comprising streptomycin, INH and PZA given daily or intermittently were only 5%–6%.Citation12,Citation13 A small retrospective study suggested that inclusion of PZA in the treatment regimen was associated with a favorable outcome.Citation14 A recent observational study among second-line treatment-naive MDR-TB patients suggested that the treatment duration of MDR-TB could be shortened to a minimum of 9 months with a gatifloxacin-based regimen that contained PZA and clofazimine throughout with kanamycin, high-dose INH and prothionamide given for at least 4 months in the initial phase.Citation15 Although the impressive treatment outcome was partially attributed to clofazimine by conjecture,Citation15 interpretation of findings could have been confounded by PZA susceptibility, which was not checked and might be present in at least 31% of the study sample according to a systematic review.Citation16 The feasibility of shortening TB treatment for selected MDR-TB patients was further corroborated by a recent report.Citation17 Subsequent retrospective analysis with the same updated dataset suggests that PZA use with in vitro activity alongside later-generation FQs and SLID may considerably increase the proportion with three-month sputum culture conversion, and marginally increase that with two-year treatment success. (Chang KC et al., unpublished). However, the above results are preliminary and future prospective studies are required to assess the possibility that PZA, alongside two or three bactericidal agents might improve the treatment of ZS-MDR-TB.
Problem with PZA susceptibility testing: phenotypic tests versus molecular tests
Despite the potential importance of PZA resistance in MDR-TB treatment outcome,Citation14,Citation18 standard phenotypic PZA susceptibility testing is seldom performed owing to technical challenges.Citation3 This also explains why PZA resistance data are generally unavailable in TB drug resistance surveys. However, a number of studies have demonstrated a high prevalence of PZA resistance among MDR-TB patients in different localities, ranging from 10% in Papua New GuineaCitation19 and 25% in Turkey,Citation20 to 49% in Thailand,Citation21 50% in Central Africa,Citation22 52% in South Africa,Citation23 53% in Japan,Citation24 55% in Taiwan,Citation25 77% in PakistanCitation26 and 85% in South KoreaCitation27 and in India.Citation28 Bacillary resistance to PZA is generally higher in XDR-TB than MDR-TB cases, ranging from 72% in Chongqing, China (Zhang WH, unpublished), 86% in South Korea,Citation27 to 93% in FQ-resistant pre-XDR-TB in Cambodia.Citation29 The reason for the high PZA resistance rates in many high-burden areas may be partly related to widespread use of PZA in retreatment regimens without drug susceptibility guidance or maybe false resistance. It is also possible that some of the above studies that reported very high PZA resistance among MDR-TB overestimated the PZA resistance frequency due to false resistance. However, the XDR-TB studies that reported very high PZA resistance were all based on molecular test of pncA sequencing rather than conventional PZA susceptibility testing.
There are different methods for PZA susceptibility testing such as Lowenstein–Jensen medium and 7H10/11 agar at pH 5.5, BACTEC 460 and MGIT 960 or BacT/ALERT systems at pH 6.0.Citation30 However, PZA susceptibility testing is prone to errors,Citation3,Citation31,Citation32 which arise from: (i) acidity of the medium required for PZA activity inhibits the growth of Mycobacterium tuberculosis—about 20%–25% of clinical isolates do not grow on acidic 7H10 plates (pH 5.5), and even with pH 6.0 in BACTEC 460 liquid medium, 3.5% of the strains did not grow;Citation33 and (ii) use of too large an inoculum (over 107 bacilli/ml) leads to increase in medium pH, which then inactivates PZA.Citation34 In a recent study, the MGIT 960 PZA susceptibility testing method was found to be even less reliable than the radioactive BACTEC 460 method giving rise to more false resistant results, presumably due to the larger inoculum used in the MGIT method. The authors suggested retesting of PZA-resistant strains by the ‘gold standard’ BACTEC 460 method and pncA sequencing of PZA-resistant strains identified by the MGIT method.Citation32 Automated PZA susceptibility testing methods, including the BACTEC 460 method, are not exempt from false resistance owing to the use of either a lower resistance breakpoint (100 µg/ml) or an inadvertently large inoculum. According to the Henderson–Hasselbalch equation, the minimum inhibitory concentration (MIC) cutoff for PZA resistance should be at least 156 µg/ml,Citation34 rather than 100 µg/ml, which is the currently used breakpoint for PZA resistance in MGIT 960 or BACTEC 460.
To circumvent the above problems, use of nicotinamide at high concentrations (0.5–2 mg/ml) at neutral pH has been proposed as a surrogate method for PZA susceptibility testing in acidic Lowenstein–Jensen medium,Citation3,Citation35,Citation36 with promising results.Citation36,Citation37,Citation38 The nicotinamide test can be used potentially as an inexpensive alternative for PZA susceptibility testing in clinical microbiology laboratories, but it has a long (several weeks) turnaround time. The PZase enzyme test (the Wayne test), using PZase as a surrogate of PZA susceptibilityCitation39 may also give rise to false resistance, due to the need for a sufficiently large inoculum that inevitably increases its turnaround time.
Mutation in the pncA gene encoding PZaseCitation40 is the major mechanism for PZA resistance in M. tuberculosis.Citation40,Citation41,Citation42 Although a lower percentage of pncA mutations in PZA-resistant strains, i.e. 64%Citation43 and 72%,Citation44 has been reported, these studies did not retest PZA-resistant strains without pncA mutations to rule out false resistance. Because of the problem of PZA susceptibility testing discussed above, the lower percentage of PZA-resistant strains, i.e., 64%Citation43 and 72%,Citation44 with pncA mutations is most likely due to false resistance, lack of vigorous retesting to rule out false resistance, the low resistance breakpoint (100 µg/ml PZA in BACTEC or MGIT) used, or the small number of strains analyzed in the study.Citation43 A recent systematic review with meta-analysis showed no significant difference between pncA sequencing and the Wayne PZase test by sensitivity and specificity in detecting PZA resistance,Citation16 indicating good correlation between pncA mutations and lack of PZase activity and PZA resistance. In analysis of PZA-resistant strains, pncA mutations were found in an average of 87% of PZA-resistant strainsCitation16 and sometimes in as high as 99% of PZA-resistant strains.Citation45 However, some studies suggest that a few PZA susceptible strains have pncA mutations that do not appear to alter the PZase enzyme activity,Citation46,Citation47,Citation48 indicating that false resistance can potentially occur by the sequencing approach. In addition, a few PZ-resistant strains with no PZase activity did not have pncA mutations,Citation42 indicating a potential regulatory gene of pncA that may have acquired a mutation. A few genuine low level PZA-resistant strains do not have pncA or rpsA mutations.Citation3,Citation41,Citation49 However, the above three situations are rareCitation24,Citation41,Citation50 and do not pose a significant problem for use of pncA sequencing for rapid detection of PZA susceptibility or resistance. Nevertheless, it would be of interest to develop a database of rare mutations that are not associated with PZA resistance to guide clinical treatment. In view of the good correlation of pncA mutations and PZA resistance.Citation41,Citation42,Citation45 the extremely diverse pncA mutations that are impossible to be included in current molecular tests such as MTBDRplus (Hain Lifescience) and GeneXpert (Cepheid) and new advances in sequencing technology and increasing affordability of DNA sequencing, we propose pncA sequencing as the best available molecular test for rapid PZA susceptibility testing. Although various molecular tests such as PCR single stranded conformation polymorphism (PCR-SSCP),Citation41 microarray,Citation51 expression of PncA protein followed by PZase activity testing,Citation52 and line-probe assayCitation53 have been used to detect pncA mutations in PZA-resistant strains, these tests are generally more onerous and expensive than pncA sequencing. As phenotypic PZA susceptibility testing is prone to false resistance, pncA sequencing can be more sensitive and specific than the BACTEC 460 or MGIT 960 method. Indeed, a recent study showed a disturbingly low sensitivity of MGIT 960 PZA susceptibility testing in comparison with the molecular test owing to a high false resistance rate of 68%.Citation54 Clinical studies comparing these two tests and the molecular test with treatment outcome are needed.
Proposition
In the area of drug-resistant TB, emphasis has previously been focused on INH and RIF resistance as in MDR-TB. In addition, in the management of MDR-TB, attention has been focused on the use of FQs and SLID. However, in view of the potentially important role of PZA in treatment outcome of MDR-TB, its unique sterilizing activity, and a considerable proportion of MDR-TB strains that are susceptible to PZA (about 50% resistance on average), we propose to classify MDR-TB based on PZA susceptibility into ZS-MDR-TB and PZA-resistant MDR-TB (ZR-MDR-TB) (). This classification may allow ZS-MDR-TB treatment to be shortened without compromising cure rates and also will improve evaluation of treatment outcomes of novel regimens in observational studies. Because of the good correlation between pncA mutations and PZA resistance, we further propose to use molecular tests such as sequencing of pncA (and FQ and SLID mutations, e.g., gyrA, rrs) to rapidly identify ZS-MDR-TB and ZR-MDR-TB with backup phenotypic tests to guide therapy. Moreover, we propose to sequence the pncA gene for all drug-resistant TB, including MDR/XDR-TB, even INH- or RIF-resistant TB. As PZA may cause hepatotoxicity,Citation55 it may be prudent to omit PZA in the treatment of ZR-MDR-TB. Finally, with the implication of PZA susceptibility on treatment outcome of MDR-TB in human studies and its superior sterilizing activity, we suggest actively exploring a simple and shortened treatment regimen for ZS-MDR-TB (possibly 9–15 months) comprising PZA plus at least two bactericidal agents including new agents like TMC207Citation9 or PA-824Citation56 or delamanidCitation57 as companion drugs, with one or two other agents. The above measures may potentially help to shorten therapy, protect against development of resistance to PZA, reduce costs and ameliorate side effects in MDR-TB treatment. Future clinical studies are needed to validate these propositions for better MDR-TB treatment.
- WHO. WHO report 2010: Global Tuberculosis Control;2010.
- Anti-tuberculosis Drug Resistance in the World, Report No, 4. 2008. Available at http://www.who.int/tb/publications/2008/en/index.html (accessed 13 March 2012).
- Zhang Y, Mitchison D.The curious characteristics of pyrazinamide: a review. Int J Tuberc Lung Dis2003;7: 6–21.
- Mitchison DA.The action of antituberculosis drugs in short course chemotherapy. Tubercle1985;66: 219–225.
- Nuermberger E, Tyagi S, Tasneen R et al.Powerful bactericidal and sterilizing activity of a regimen containing PA-824, moxifloxacin, and pyrazinamide in a murine model of tuberculosis. Antimicrob Agents Chemother2008;52: 1522–1524.
- Rosenthal IM, Zhang M, Williams KN et al.Daily dosing of rifapentine cures tuberculosis in three months or less in the murine model. PLoS Med2007;4: e344.
- Andries K, Verhasselt P, Guillemont J et al.A diarylquinoline drug active on the ATP synthase of Mycobacterium tuberculosis. Science2005;307: 223–227.
- Ibrahim M, Andries K, Lounis N et al.Synergistic activity of R207910 combined with pyrazinamide against murine tuberculosis. Antimicrob Agents Chemother2007;51: 1011–1015.
- Diacon AH, Pym A, Grobusch M et al.The diarylquinoline TMC207 for multidrug-resistant tuberculosis. N Engl J Med2009;360: 2397–2405.
- McCune RM Jr, McDermott W, Tompsett R.The fate of Mycobacterium tuberculosis in mouse tissues as determined by the microbial enumeration technique. II. The conversion of tuberculous infection to the latent state by the administration of pyrazinamide and a companion drug. J Exp Med1956;104: 763–802.
- McCune RM, Feldmann FM, Lambert HP, McDermott W.Microbial persistence. I. The capacity of tubercle bacilli to survive sterilization in mouse tissues. J Exp Med1966;123: 445–468.
- Hong Kong TB Treatment Service/British Medical Research Council.Controlled trial of 8-month and 9-month regimens of daily and intermittent streptomycin plus isoniazid plus pyrazinamide for pulmonary tuberculosis in Hong Kong. Tubercle1975;56: 81–96.
- Hong Kong TB Treatment Service/British Medical Research Council.Controlled trial of 6-month and 9-month regimens of daily and intermittent streptomycin plus isoniazid plus pyrazinamide for pulmonary tuberculosis in Hong Kong. The results up to 30 months. Am Rev Respir Dis1977;115: 727–735.
- Mitnick C, Bayona J, Palacios E et al.Community-based therapy for multidrug-resistant tuberculosis in Lima, Peru. N Engl J Med2003;348: 119–128.
- van Deun A, Maug AK, Salim MA et al.Short, highly effective and inexpensive standardized treatment of multidrug-resistant tuberculosis. Am J Respir Crit Care Med2010;182: 684–692.
- Chang KC, Yew WW, Zhang Y.Pyrazinamide susceptibility testing in Mycobacterium tuberculosis: a systematic review with meta-analyses. Antimicrob Agents Chemother2011;55: 4499–4505.
- Leung E, Yew W, Leung C, Leung W, Tam C.Shorter treatment duration for selected patients with multidrug-resistant tuberculosis. Eur Respir J2011;38: 227–230.
- Migliori GB, Besozzi G, Girardi E et al.Clinical and operational value of the extensively drug-resistant tuberculosis definition. Eur Respir J2007;30: 623–626.
- Simpson G, Coulter C, Weston J et al.Resistance patterns of multidrug-resistant tuberculosis in Western Province, Papua New Guinea. Int J Tuberc Lung Dis2011;15: 551–552.
- Senol G, Coskun M, Gunduz AT, Bicmen C, Gayaf M, Ozsoz A.[Investigation of pyrazinamide resistance in multidrug-resistant tuberculosis cases in Hospital of Pulmonary Diseases, Izmir, Turkey]. Mikrobiyoloji Bulteni2008;42: 591–597. Turkish.
- Jonmalung J, Prammananan T, Leechawengwongs M, Chaiprasert A.Surveillance of pyrazinamide susceptibility among multidrug-resistant Mycobacterium tuberculosis isolates from Siriraj Hospital, Thailand. BMC Microbiol2010;10: 223.
- Minime-Lingoupou F, Pierre-Audigier C, Kassa-Kelembho E et al.Rapid identification of multidrug-resistant tuberculosis isolates in treatment failure or relapse patients in Bangui, Central African Republic. Int J Tuberc Lung Dis2010;14: 782–785.
- Louw GE, Warren RM, Donald PR et al.Frequency and implications of pyrazinamide resistance in managing previously treated tuberculosis patients. Int J Tuberc Lung Dis2006;10: 802–807.
- Ando H, Mitarai S, Kondo Y et al.Pyrazinamide resistance in multidrug-resistant Mycobacterium tuberculosis isolates in Japan. Clin Microbiol Infect2010;16: 1164–1168.
- Chiu YC, Huang SF, Yu KW, Lee YC, Feng JY, Su WJ.Characteristics of pncA mutations in multidrug-resistant tuberculosis in Taiwan. BMC Infect Dis2011;11: 240.
- Rao NA, Irfan M, Soomro MM, Mehfooz Z.Drug resistance pattern in multidrug resistance pulmonary tuberculosis patients. J Coll Physicians Surg Pak2010;20: 262–265.
- Kim HJ, Kwak HK, Lee J et al.Patterns of pncA mutations in drug-resistant Mycobacterium tuberculosis isolated from patients in South Korea. Int J Tuberc Lung Dis2012;16: 98–103.
- Shenai S, Rodrigues C, Sadani M, Sukhadia N, Mehta A.Comparison of phenotypic and genotypic methods for pyrazinamide susceptibility testing. Indian J Tuberc2009;56: 82–90.
- Pierre-Audigier C, Surcouf C, Cadet-Daniel V et al.Fluoroquinolone and pyrazinamide resistance in multidrug-resistant tuberculosis. Int J Tuberc Lung Dis2012;16: 221–223, i–ii.
- Aragon LM, Garrigo M, Moreno C, Espanol M, Coll P.Evaluation of the BacT/ALERT PZA kit in comparison with the BACTEC 460TB PZA for testing Mycobacterium tuberculosis susceptibility to pyrazinamide. J Antimicrob Chemother2007;60: 655–657.
- Hewlett D Jr, Horn DL, Alfalla C.Drug-resistant tuberculosis: inconsistent results of pyrazinamide susceptibility testing. JAMA1995;273: 916–917.
- Chedore P, Bertucci L, Wolfe J, Sharma M, Jamieson F.Potential for erroneous results indicating resistance when using the Bactec MGIT 960 system for testing susceptibility of Mycobacterium tuberculosis to pyrazinamide. J Clin Microbiol2010;48: 300–301.
- Miller MA, Thibert L, Desjardins F, Siddiqi SH, Dascal A.Testing of susceptibility of Mycobacterium tuberculosis to pyrazinamide: comparison of Bactec method with pyrazinamidase assay. J Clin Microbiol1995;33: 2468–2470.
- Zhang Y, Permar S, Sun Z.Conditions that may affect the results of susceptibility testing of Mycobacterium tuberculosis to pyrazinamide. J Med Microbiol2002;51: 42–49.
- Brander E.A simple way of detecting pyrazinamide resistance. Tubercle1972;53: 128–131.
- Martin A, Takiff H, Vandamme P, Swings J, Palomino JC, Portaels F.A new rapid and simple colorimetric method to detect pyrazinamide resistance in Mycobacterium tuberculosis using nicotinamide. J Antimicrob Chemother2006;58: 327–331.
- Mirabal NC, Yzquierdo SL, Lemus D et al.Evaluation of colorimetric methods using nicotinamide for rapid detection of pyrazinamide resistance in Mycobacterium tuberculosis. J Clin Microbiol2010;48: 2729–2733.
- Martin A, Cubillos-Ruiz A, von Groll A, del Portillo P, Portaels F, Palomino JC.Nitrate reductase assay for the rapid detection of pyrazinamide resistance in Mycobacterium tuberculosis using nicotinamide. J Antimicrob Chemother2008;61: 123–127.
- McClatchy JK, Tsang AY, Cernich MS.Use of pyrazinamidase activity on Mycobacterium tuberculosis as a rapid method for determination of pyrazinamide susceptibility. Antimicrob Agents Chemother1981;20: 556–557.
- Scorpio A, Zhang Y.Mutations in pncA, a gene encoding pyrazinamidase/nicotinamidase, cause resistance to the antituberculous drug pyrazinamide in tubercle bacillus. Nat Med1996;2: 662–667.
- Scorpio A, Lindholm-Levy P, Heifets L et al.Characterization of pncA mutations in pyrazinamide-resistant Mycobacterium tuberculosis. Antimicrob Agents Chemother1997;41: 540–543.
- Cheng SJ, Thibert L, Sanchez T, Heifets L, Zhang Y.pncA mutations as a major mechanism of pyrazinamide resistance in Mycobacterium tuberculosis: spread of a monoresistant strain in Quebec, Canada. Antimicrob Agents Chemother2000;44: 528–532.
- Huang TS, Lee SS, Tu HZ et al.Correlation between pyrazinamide activity and pncA mutations in Mycobacterium tuberculosis isolates in Taiwan. Antimicrobial Agents and Chemotherapy2003;47: 3672–3673.
- Sreevatsan S, Pan X, Zhang Y, Kreiswirth BN, Musser JM.Mutations associated with pyrazinamide resistance in pncA of Mycobacterium tuberculosis complex organisms. Antimicrob Agents Chemother1997;41: 636–640.
- Somoskovi A, Dormandy J, Parsons LM et al.Sequencing of the pncA gene in members of the Mycobacterium tuberculosis complex has important diagnostic applications: identification of a species-specific pncA mutation in ‘Mycobacterium canettii’ and the reliable and rapid predictor of pyrazinamide resistance. J Clin Microbiol2007;45: 595–599.
- Zhang H, Deng JY, Bi LJ et al.Characterization of Mycobacterium tuberculosis nicotinamidase/pyrazinamidase. Febs J2008;275: 753–762.
- Sheen P, Ferrer P, Gilman RH et al.Effect of pyrazinamidase activity on pyrazinamide resistance in Mycobacterium tuberculosis. Tuberculosis (Edinb)2009;89: 109–113.
- Lemaitre N, Callebaut I, Frenois F, Jarlier V, Sougakoff W.Study of the structure-activity relationships for the pyrazinamidase (PncA) from Mycobacterium tuberculosis. Biochem J2001;353( Pt 3): 453–458.
- Shi W, Zhang X, Jiang X et al.Pyrazinamide inhibits trans-translation in Mycobacterium tuberculosis. Science2011;333: 1630–1632.
- Jureen P, Werngren J, Toro JC, Hoffner S.Pyrazinamide resistance and pncA gene mutations in Mycobacterium tuberculosis. Antimicrobial Agents and Chemotherapy2008;52: 1852–1854.
- Wade MM, Volokhov D, Peredelchuk M, Chizhikov V, Zhang Y.Accurate mapping of mutations of pyrazinamide-resistant Mycobacterium tuberculosis strains with a scanning-frame oligonucleotide microarray. Diagn Microbiol Infect Dis2004;49: 89–97.
- Zhou M, Geng X, Chen J et al.Rapid colorimetric testing for pyrazinamide susceptibility of M. tuberculosis by a PCR-based in-vitro synthesized pyrazinamidase method. PLoS One2011;6: e27654.
- Sekiguchi J, Nakamura T, Miyoshi-Akiyama T et al.Development and evaluation of a line probe assay for rapid identification of pncA mutations in pyrazinamide-resistant mycobacterium tuberculosis strains. J Clin Microbiol2007;45: 2802–2807.
- Simons SO, van Ingen J, van der Laan T et al.Validation of pncA gene sequencing in combination with the MGIT method to test susceptibility of Mycobacterium tuberculosis to pyrazinamide. J Clin Microbiol2012;50: 428–434.
- Chang KC, Leung CC, Yew WW, Lau TY, Tam CM.Hepatotoxicity of pyrazinamide: cohort and case–control analyses. Am J Respir Crit Care Med2008;177: 1391–1396.
- Stover CK, Warrener P, VanDevanter DR et al.A small-molecule nitroimidazopyran drug candidate for the treatment of tuberculosis. Nature2000;405: 962–966.
- Gler MT, Skripconoka V, Sanchez-Garavito E et al.Delamanid for multidrug-resistant pulmonary tuberculosis. N Engl J Med2012;366: 2151–2160.