Abstract
We evaluated the epidemiological and molecular features of community-associated methicillin-resistant Staphylococcus aureus (CA-MRSA) and methicillin-sensitive S. aureus (MSSA) from children and adult patients with skin and soft-tissue infections (SSTIs) in China. Prospective community-acquired S. aureus SSTI surveillance was conducted in 23 hospitals over a 24-month period. Susceptibility to 16 antimicrobials was evaluated using the agar dilution method. StatApriori was used to determine statistically significant association trends. The genotypic characteristics of CA-MRSA isolates were tested by staphylococcal cassette chromosome mec (SCCmec) typing, staphylococcal protein A (spa) typing, and multilocus sequence typing. The presence of Panton–Valentine leukocidin (pvl) genes was determined. Overall, 71.6% (1946/2716) of cases were community-associated S. aureus. CA-MRSA accounted for 2.6% (51). Out of 1895 methicillin-sensitive S. aureus strains, 97.3% were resistant to erythromycin, 96.6% to penicillin and 89.1% to clindamycin. No S. aureus strains were resistant to vancomycin. Thirteen sequence types (STs) and 17 spa types were detected among the CA-MRSA strains. The most prevalent sequence type was ST121 (19/51, 37.3%), followed by ST59 (13/51, 25.5%). In addition, t437 was predominant, accounting for 43.1% (22/51). Only five (9.8%) of the CA-MRSA strains harbored pvl genes. There were no significant differences in antibiotic sensitivity profiles between ST121 and non-ST121 MRSA isolates. However, ST121 strains tended to be more resistant to cefazolin, whereas non-ST121 strains were more resistant to chloramphenicol. In conclusion, CA-MRSA infections are rare among Chinese SSTI patients. MRSA strains in China have diverse genetic backgrounds, with ST121 being the predominant clone. Fusidic acid and mupirocin remain effective for topical treatment.
INTRODUCTION
Staphylococcus aureus (S. aureus) is a significant human pathogen worldwide, particularly in healthcare settings. It has long been recognized as an important causative agent of skin and soft-tissue infections (SSTIs), which range from folliculitis to life-threatening conditions such as necrotizing fasciitis. The increasing prevalence of methicillin-resistant S. aureus (MRSA) and its ability to resist multiple drugs has posed a serious challenge.Citation1 Hospital-associated MRSA has been extensively investigated, with a high prevalence of MRSA (52.3%–76.9%) in mainland China.Citation2 However, considering China's vast territory, the data on SSTIs caused by community-associated methicillin-resistant S. aureus (CA-MRSA) are limited. Despite the importance of MRSA, methicillin-sensitive S. aureus (MSSA) is among the most common causative agents of SSTIs.Citation3 The epidemiological surveillance of MRSA and MSSA is critical for the development and implementation of infection control programs.
This study focused on an expanded sample of SSTI cases to obtain accurate molecular characteristics of CA-MRSA in mainland China and to produce a more comprehensive national description of the molecular epidemiology and resistance profiles of CA-MRSA in children and adults in China. Although previous studies reported on S. aureus biogeography and virulence,Citation4 to our knowledge, this is the first study to compare contemporaneous CA-MRSA of SSTIs from adults and children and the first such study carried out in mainland China.
MATERIALS AND METHODS
Patient enrollment
This was a laboratory-based multicenter study involving the voluntary participation of 23 hospitals (including 13 children’s hospitals and ten adult hospitals) in six geographical regions (Northeast, North China, Northwest, East China, South Central China and Southwest) located throughout China. The inclusion criteria for these institutions were: (i) at least one children’s hospital and one adult hospital located in five regions, but only one children's hospital in the Northeast area; and (ii) certified as a rank A tertiary hospital by the Ministry of Health of China. Clinical data were collected from outpatients with SSTIs in the Department of Dermatology of each hospital during a 24-month period from October 2009 to September 2011.
Clinical data collection
Eligible patients were those with at least one sample from any site that was culture positive for S. aureus who met the following criteria for community-associated S. aureus: (i) a culture sample was obtained during an outpatient visit or within 48 h of hospitalization; (ii) the patient had not been admitted to a hospital, nursing home or any other long-term care facility within the past year; and (iii) the patient had no history within the past year of known risk factors for MRSA, including current intravenous drug use, surgery, dialysis, an indwelling catheter or a percutaneous medical device. A case report form was completed for each patient who included demographic information, clinical symptoms, laboratory findings, type of infection diagnosed, all antibiotic use and clinical outcome.
Bacterial strains
Specimens were collected from infection sites of every patient enrolled and cultured on blood agar. Preliminary identification was performed based on bacterial morphology, Gram staining, hemolysis, and catalase tests at the central laboratory. Then, Slidex Staph Plus (bioMérieux, Marcy I'Etoile, France) latex agglutination was performed for the rapid detection of S. aureus. To avoid overrepresentation, we included only the first isolate from each patient. MRSA isolates were initially identified using the oxacillin minimum inhibitory concentration method and confirmed for the presence of the mecA gene by PCR as previously described.Citation5
Antimicrobial susceptibility testing
The minimum inhibitory concentrations of penicillin, oxacillin, cefazolin, cefuroxime, ceftriaxone, erythromycin, clindamycin, ciprofloxacin, chloramphenicol, gentamicin, rifampicin, tetracycline, trimethoprim-sulfamethoxazole, vancomycin, fusidic acid and mupirocin were determined by agar dilution method in accordance with the 2010 guidelines of the Clinical and Laboratory Standards Institutes.Citation6 All antibiotics were from Sigma Chemical Co., St Louis, MO, USA except mupirocin from GlaxoSmithKline, Brentford, London. Fusidic acid minimum inhibitory concentrations were determined according to the European Committee on Susceptibility Testing guidelines (EUCAST, version 1.3, 2010, Basel, Switzerland). The S. aureus strain ATCC 29213 was used as a control.
Molecular typing methods
Staphylococcal cassette chromosome mec (SCCmec) typing, staphylococcal protein A (spa) typing, and multilocus sequence typing were performed using PCR as previously described for all CA-MRSA isolates.Citation5, Citation7, Citation8 The presence of Panton–Valentine leukocidin (pvl) genes, such as lukS-PV and lukF-PV, was also determined by PCR as previously described.Citation9
Statistical analysis
A χ2-test or Fisher’s exact test was used to analyze quantitative variables. Statistical analyses were performed using SPSS, version 13.0 software (SPSS, Chicago, IL, USA). A P-value of ≤0.05 was considered statistically significant. All susceptibility data and molecular test results were analyzed using WHONET software, version 5.6. StatApriori (WHO, Geneva, Switzerland) was used for searching statistically significant association rules.
RESULTS
Patient demographics
A total of 2716 patients were identified during the study period. Out of these patients, 71.6% (1946) fulfilled the criteria for inclusion in the study, 2.6% (51) met the definition of CA-MRSA infection and the rest were classified as having MSSA infection. The incidence of S. aureus from children’s hospitals (82.6%, 1705/2046) was much higher than from adult hospitals (36.96%, 241/652). Common lesions in children included impetigo (81.9%, 1397/1705), staphylococcal scald skin syndrome (4.8%, 82/1705), and secondary infection of eczema (4.3%, 74/1705), whereas in adults, common lesions included secondary infection of eczema (24%, 58/241), impetigo (20%, 48/241) and folliculitis (11%, 27/241). Demographic and clinical features of all patients are shown in .
Table 1 Demographic and clinical features of patients from children and adults with skin and soft-tissue infections
Comparison of resistance profiles of S. aureus isolates
Overall, CA-MRSA accounted for 2.6% (51) of 1946 S. aureus strains. Of 1895 MSSA strains isolated, 97.3% strains were resistant to erythromycin, followed by 96.6% to penicillin, 89.1% to clindamycin, 42.0% to tetracycline and 14.4% to chloramphenicol. None of the S. aureus strains were resistant to vancomycin. The antimicrobial susceptibilities of MRSA isolates were compared with MSSA isolates (). CA-MRSA isolates demonstrated a higher rate of resistance to chloramphenicol, ciprofloxacin, ceftriaxone and cefixime (31.4% vs. 14.4%, 13.7% vs. 6.3%, 23.5% vs. 0.9% and 19.6% vs. 2.5%, respectively). The susceptibility profiles of MRSA to other antimicrobial agents were similar to those of MSSA. All CA-MRSA and MSSA isolates tested were sensitive to vancomycin. Significant differences in antimicrobial susceptibility profiles of isolates from children and adults were also observed (P<0.05) (). S. aureus isolates obtained from children were more likely to be susceptible to chloramphenicol, gentamicin, ciprofloxacin, trimethoprim-sulfamethoxazole, fusidic acid, mupirocin and cephalosporin than those from adults.
Table 2 Results of the susceptibility testing of the strains
Molecular characteristics of CA-MRSA isolates
High genetic diversity was observed among the 51 CA-MRSA isolates: 13 STs and 17 spa types harbored two SCCmec types (). Surprisingly, the most prevalent ST was ST121 (19/51, 37.3%), followed by ST59 (13/51, 25.5%). Among them, t437 was predominant, which accounted for 43.1% (22/51) of all CA-MRSA isolates, followed by t2086, t1425 and t127. Only SCCmec type IV was found in North China. Interestingly, strains ST121, ST59 and t437 were uncommon in East China. Some spatial variations were observed in the distribution of spa types (e.g., t437 occurred in 66.7% and 55.6% isolates from Children’s Hospital of Chongqing Medical University and Beijing Children’s Hospital, respectively). However, such differences were not significant. No other clinical or spatial associations were observed in the distribution of spa types or STs with regard to infection type, sex, region or hospital of origin.
Table 3 Clinical and molecular features of 51 cases with CA-MRSA infections
Of the isolates tested, only five (9.8%) of the CA-MRSA isolates harbored pvl genes. Four of the strains were isolated from children. Three patients suffered from abscesses, one from a furuncle and one from cellulitis. Four of the strains were t437. The clinical and molecular characteristics of the five CA-MRSA isolates are shown in .
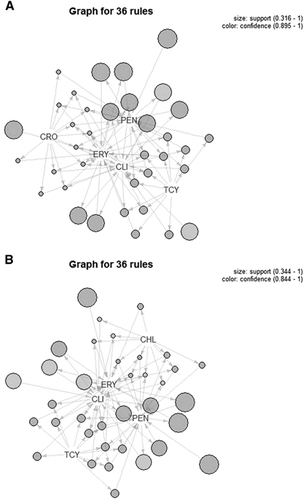
Characteristics of ST121 CA-MRSA strains
The 19 ST121 strains were isolated from patients with impetigo (13/19), cellulitis (1/19), secondary infection of eczema (3/19) and abscess (2/19). These 19 strains comprised nine spa types; however, only t437 was found in ST59 strains. There was no significant difference in antibiotic sensitivities between ST121 and non-ST121 MRSA isolates. Thirty-six separate associations between the five antimicrobials (erythromycin, penicillin, tetracycline, clindamycin and cefazolin/chloramphenicol) were found. Moreover, ST121 CA-MRSA strains tended to be more resistant to cefazolin, whereas non-ST121 CA-MRSA strains tended to be more resistant to chloramphenicol (). Two mupirocin-resistant strains were observed among non-ST121 CA-MRSA strains.
DISCUSSION
This study was conducted at 23 large, inner city, comprehensive medical teaching and research hospitals selected by the Chinese Ministry of Health to fill an important gap in the knowledge of community-associated S. aureus SSTIs in China. To our knowledge, this is the first large-scale comparison of CA-MRSA clinical characteristics between children and adults with S. aureus SSTIs in mainland China. We present three major findings: (i) the prevalence of CA-MRSA was low among children and adults with SSTIs; (ii) CA-MRSA strains in China have diverse genetic backgrounds and there is no trend of an outbreak thus far; and (iii) ST121 is currently the predominant clone.
The prevalence of CA-MRSA varies geographically, with a detection rate in patients with skin infections of 1–3% in France and up to 50% in the United States.Citation10 The incidence of CA-MRSA SSTIs in China is unclear because of the lack of systematic epidemiological studies. A few small studies demonstrated that the incidence of CA-MRSA with SSTIs was 1.1–4% in Beijing and other regions of China.Citation11, Citation12 In this study, we found the prevalence of CA-MRSA SSTIs to be surprisingly low, from 1.3% in North China to 6.1% in Southwest China. Furthermore, no MRSA infections were observed at two children’s hospitals and four adult hospitals. A potential explanation for the differences in the prevalence of MRSA infections in distinct regions of China is most likely the vast size of the territories, along with disparities in economic development. Another explanation may be a data bias of fewer cases in these regions. The current absence of CA-MRSA outbreaks or reports on serious outcomes of CA-MRSA infections suggests that the low prevalence observed in this study may truly reflect the current situation in China.
Antibiogram testing is a crucial step in MRSA screening and selection of the appropriate antibiotic for proper treatment of skin infections. Our study showed that most patients had MSSA (1 964/2 716 patients). On comparing the antibiotic susceptibility patterns of bacterial isolates from children and adults, significant differences were found. Antibiotic susceptibility patterns therefore appear to depend mainly on bacterial strains, rather than type of skin infections. The majority of patients with SSTIs can be cured only using topical antibiotics; however, a small number of patients require systematic treatment. According to the results of antibiotic susceptibility tests in this study, penicillin and erythromycin are no longer appropriate agents, and cephalosporin may be the wiser choice. Although MRSA are generally resistant to all previously available beta-lactams, it was interesting that cephalosporin demonstrated potent activity against CA-MRSA. Indeed, traditional antistaphylococcal antibiotics (cephalosporin) have been associated with good clinical outcomes for CA-MRSA SSTIs. Recently, ceftaroline, which is a novel parenteral broad-spectrum cephalosporin, demonstrated bactericidal activity against Gram-positive organisms (including MRSA) and represented a bactericidal option for the treatment of MRSA infections, including those caused by isolates with reduced susceptibilities to vancomycin and daptomycin.Citation13
Fusidic acid and mupirocin are effective topical antibacterial agents for the management of skin infections and S. aureus colonization in both patients and healthcare workers. In the past decade, there has been an increase in fusidic acid resistance in a number of countries. However, the fusidic acid resistance rates between MSSA and MRSA may differ. From 1998 to 2001, data from the United Kingdom showed that the resistance rates for fusidic acid in MSSA increased from 6.0% to 11.5%, whereas the resistance rates in MRSA were much lower and remained constant at ~2%.Citation14 In this study, we also found it interesting that only MSSA was resistant to fusidic acid (1.4%). In 1999, fusidic acid was first introduced in China and has been available as a topical cream since 2003. However, resistance to fusidic acid in China was reported after 2007.Citation15, Citation16 Therefore, selective pressure from antibiotic use likely led to increased resistance to fusidic acid. Similarly, initial reports on mupirocin-resistant S. aureus emerged shortly after the introduction of mupirocin into clinical practice.Citation17 However, the prevalence of mupirocin resistance has increased in settings where this agent is used extensively. It has been reported that more than 50% of community-associated S. aureus strains displayed high-level resistance to mupirocin in Canada.Citation18 In Beijing Children’s Hospital, mupirocin ointment has been prescribed since 1993. However, only one strain was found to be resistant to mupirocin in 2005.Citation15 In this study, the number of mupirocin-resistant S. aureus isolates clearly increased, but remained low compared with rates observed in other countries. Mupirocin therefore remains an effective therapy for the elimination of staphylococci in China.
It has been reported that five major CA-MRSA clones are disseminating worldwide. For example, the ST1 clone is observed in Asia, Europe, and the United States; the ST8 clone in Europe and the United States; the ST30 clone in Australia, Europe and South America; the ST59 clone in Asia and the United States; and the ST80 clone in Asia, Europe, and the Middle East.Citation19 In 2007, Schefold et al.Citation20 first reported a sepsis case of a 51-year-old male caused by S. aureus ST121. Thereafter, ST121 MSSA isolates were found to be distributed in 15 out of the 19 surveyed countries, namely Paraguay, New Caledonia, Togo, France, Czech Republic, Germany, Turkey, the United States, French West Indies, United Kingdom, Polynesia, Switzerland, Spain, Algeria and The Netherlands.Citation21 A small study performed in mainland China demonstrated that ~8.3% (1/12) of SSTIsCitation22 and 30.6% of asymptomatically colonized children in kindergartensCitation23 were associated with ST121 isolates. These findings suggest that most ST121 strains are MSSA. The ST121 clone is rarely dominant in MRSA clinical infections. It has been reported that 11.8% of MRSA strains belonged to ST121 in Cambodia,Citation24 7.1% in Japan,Citation25 5.4% in PortugalCitation26 and 0.3% in Spain.Citation27 The important finding from the present study is that ST121 (35.3%), which had been previously documented in only two isolates (3.5%) among MRSA causing SSTIs in 2015,Citation28 was more prevalent than ST59 (25.5%). Moreover, ST121 isolates have disseminated in seven hospitals located in five regions in mainland China. Interestingly, neither ST121 nor ST59 was observed in East China hospitals, an area of relatively rapid economic development. In addition, predominant spa type t437, which comprised 43.2% of all CA-MRSA, was also not observed in East China. There were also no significant differences in antibiotic sensitivities between MRSA and MSSA. MSSA has evolved as MRSA through the acquisition of SCCmec,Citation29, Citation30 and therefore, some MSSA genotypes are the same as some popular CA-MRSA genotypes. Baines et al.Citation31 found that ST5 MRSA clone has emerged from locally circulating ST5 MSSA strains in New Zealand. In addition, Stegger et al.Citation32 determined that a single descendant of a PVL-positive methicillin-sensitive ancestor circulating in sub-Saharan Africa rose to become the dominant CA-MRSA clone in Europe, the Middle East and North Africa. The findings in this study indicate that the genetic background of CA-MRSA found in mainland China is complex. We will next probe more deeply into the genotyping of MSSA and expect to find clues of MRSA 'conversion' from MSSA in China.
The role of PVL in the pathogenesis of staphylococcal infections remains controversial. However, PVL has been closely associated with CA-MRSA infections, and there is a strong epidemiological association between carriage of pvl genes and successful CA-MRSA lineages. PVL-positive S. aureus strains are more frequently associated with cellulitis and abscesses than with impetigo.Citation33 Although highly virulent CA-MRSA strains carrying pvl genes are known to prevail worldwide, the prevalence of PVL-positive MRSA strains from SSTIs in China was reported to range from 12.5% to 19.1%.Citation28, Citation34 Compared with a previous study, the overall positivity rates of pvl genes in the present study was lower (9.8%), indicating a decreased prevalence of pvl genes among S. aureus SSTI isolates in China. Five patients with PVL-positive CA-MRSA infections were able to perform daily activities and had no identifiable risk factors. All five patients were empirically treated with cephalosporin and good outcomes were achieved.
In summary, this study provided information on the epidemiological and molecular characteristics of community-acquired S. aureus SSTIs among Chinese populations. The low prevalence of CA-MRSA is positive news. Interestingly, ST121 was the predominant clone among CA-MRSA strains. Moreover, there were no clear regional variations. To fully understand the epidemiology of S. aureus clone ST121, the continued systematic surveillance of both hospital- and community-associated isolates is required.
This study was supported by the National Natural Science Foundation of China (NO 81201237), the Beijing Municipal Administration of Hospitals Clinical Medicine Development of Special Funding Support (NO ZYLX201601), the Beijing Municipal Administration of Hospitals’ Youth Program (NO QML20151101) and Beijing Children’s Hospital Young Investigator Program (NO BCHYIPA-2016-11). We thank the China Dermatologist Association. We also thank the following hospitals and their staff members for participating in this study: Beijing Children’s Hospital, Harbin Children’s Hospital, Zhengzhou Children’s Hospital, Xuzhou Children’s Hospital, Guangzhou Women and Children’s Medical Center, Hunan Children’s Hospital, The First People's Hospital of Urumqi, Children’s Hospital of Chongqing Medical University, Peking University First Hospital, Xijing Hospital, West China Hospital, Children’s Hospital of Shanxi, Children’s Hospital of Changchun, Wuhan No. 1 Hospital, The Second Xiangya Hospital of Central South University, Peking University People's Hospital, Southwest Hospital, The First Teaching Hospital of Xinjiang Medical University, Children’s Hospital of Fudan University, Peking University Third Hospital, Huashan Hospital of Fudan University, Dalian Children’s Hospital of Dalian Medical University and Tianjin Children’s Hospital.
- DavidMZ,Boyle-VavraS,ZychowskiDL,DaumRS.Methicillin-susceptible Staphylococcus aureus as a predominantly healthcare-associated pathogen: a possible reversal of roles?PLoS One2011; 6:e18217.
- XiaoYH,GiskeCG,WeiZQet al.Epidemiology and characteristics of antimicrobial resistance in China.Drug Resist Updat2011; 14:236–250.
- CosgroveSE,SakoulasG,PerencevichENet al.Comparison of mortality associated with methicillin-resistant and methicillin-susceptible Staphylococcus aureus bacteremia: a meta-analysis.Clin Infect Dis2003; 36:53–59.
- JiangW,ZhouZ,ZhangK,YuY.Epidemiological investigation of community-acquired Staphylococcus aureus infection.Genet Mol Res12:6923–6930.
- ZhangK,McClureJA,ElsayedS,LouieT,ConlyJM.Novel multiplex PCR assay for characterization and concomitant subtyping of staphylococcal cassette chromosome mec types I to V in methicillin-resistant Staphylococcus aureus.J Clin Microbiol2005; 43:5026–5033.
- CLSI Performance Standards for Antimicrobial Susceptibility Testing; Twenty-second Informational SupplementClinical and Laboratory Standards Institute document: M100-S20.Clinical and Laboratory Standards Institute: Wayne, PA, USA.2012.
- EnrightMC,DayNP,DaviesCE,PeacockSJ,SprattBG.Multilocus sequence typing for characterization of methicillin-resistant and methicillin-susceptible clones of Staphylococcus aureus.J Clin Microbiol2000; 38:1008–1015.
- KoreenL,RamaswamySV,GravissEAet al.spa typing method for discriminating among Staphylococcus aureus isolates: implications for use of a single marker to detect genetic micro- and macrovariation.J Clin Microbiol2004; 42:792–799.
- BabaT,TakeuchiF,KurodaMet al.Genome and virulence determinants of high virulence community-acquired MRSA.Lancet2002; 359:1819–1827.
- DeLeoFR,OttoM,KreiswirthBN,ChambersHF.Community-associated meticillin-resistant Staphylococcus aureus.Lancet2010; 375:1557–1568.
- GengWJ,YangYH,WuDJet al.Molecular characteristics of community-acquired, methicillin-resistant Staphylococcus aureus isolated from Chinese children.Fems Immunol Med Microbiol2010; 58:356–362.
- WuDJ,GengWJ,YangYH,ShenXZ.Epidemiology and molecular characteristics of community-associated methicillin-resistant and methicillin-susceptible Staphylococcus aureus from skin/soft tissue infections in Beijing Children's Hospital, China.Diagn Microbiol Infect Dis2010; 67:1–8.
- SaravolatzL,PawlakJ,JohnsonL.In vitro activity of ceftaroline against community-associated methicillin-resistant, vancomycin-intermediate, vancomycin-resistant, and daptomycin-nonsusceptible Staphylococcus aureus isolates.Antimicrob Agents Chemother2010; 54:3027–3030.
- BrownEM,ThomasP.Fusidic acid resistance in Staphylococcus aureus isolates.Lancet2002; 359:803.
- LiuY,KongF,ZhangXet al.Antimicrobial susceptibility of Staphylococcus aureus isolated from children with impetigo in China from 2003 to 2007 shows community-associated methicillin-resistant Staphylococcus aureus to be uncommon and heterogeneous.Br J Dermatol2009; 161:1347–1350.
- LiuY,GengW,YangYet al.Susceptibility to and resistance determinants of fusidic acid in Staphylococcus aureus isolated from Chinese children with skin and soft tissue infections.FEMS Immunol Med Microbiol2012; 64:212–218.
- RahmanMNW,CooksonB.Mupirocin-resistant Staphylococcus aureus.Lancet1987; 2:387–388.
- MulveyMR,MacDougallL,CholinBet al.Community-associated methicillin-resistant Staphylococcus aureus, Canada.Emerg Infect Dis2005; 11:844–850.
- DeurenbergRH,StobberinghEE.The evolution of Staphylococcus aureus.Infect Genet Evol2008; 8:747–763.
- SchefoldJC,EspositoF,StormCet al.Therapy-refractory Panton Valentine Leukocidin-positive community-acquired methicillin-sensitive Staphylococcus aureus sepsis with progressive metastatic soft tissue infection: a case report.J Med Case Rep2007; 1:165.
- RaoQ,ShangW,HuX,RaoX.Staphylococcus aureus ST121: a globally disseminated hypervirulent clone.J Med Microbiol2015; 64:1462–1473.
- JiangW,ZhouZ,ZhangK,YuY.Epidemiological investigation of community-acquired Staphylococcus aureus infection.Genet Mol Res2013; 12:6923–6930.
- FanJ,ShuM,ZhangGet al.Biogeography and virulence of Staphylococcus aureus.PLoS One2009; 4:e6216.
- ChhengK,TarquinioS,WuthiekanunVet al.Emergence of community-associated methicillin-resistant Staphylococcus aureus associated with pediatric infection in Cambodia.PLoS One2009; 4:e6630.
- KikutaH,ShibataM,NakataSet al.Predominant dissemination of PVL-negative CC89 MRSA with SCCmec Type II in children with impetigo in Japan.Int J Pediatr2011; 2011:143872.
- Aires de SousaM,ConceicaoT,SimasC,de LencastreH.Comparison of genetic backgrounds of methicillin-resistant and -susceptible Staphylococcus aureus isolates from Portuguese hospitals and the community.J Clin Microbiol2005; 43:5150–5157.
- Gonzalez-DominguezM,SeralC,SaenzYet al.Epidemiological features, resistance genes, and clones among community-onset methicillin-resistant Staphylococcus aureus (CO-MRSA) isolates detected in northern Spain.Int J Med Microbiol2012; 302:320–326.
- YuF,LiuY,LvJet al.Antimicrobial susceptibility, virulence determinant carriage and molecular characteristics of Staphylococcus aureus isolates associated with skin and soft tissue infections.Braz J Infect Dis2015; 19:614–622.
- International Working Group on the Classification of Staphylococcal Cassette Chromosome E.Classification of staphylococcal cassette chromosome mec (SCCmec): guidelines for reporting novel SCCmec elements.Antimicrob Agents Chemother2009; 53:4961–4967.
- DavidMZ,DaumRS.Community-associated methicillin-resistant Staphylococcus aureus: epidemiology and clinical consequences of an emerging epidemic.Clin Microbiol Rev2010; 23:616–687.
- BainesSL,HowdenBP,HeffernanHet al.Rapid emergence and evolution of Staphylococcus aureus clones harboring fusC-containing staphylococcal cassette chromosome elements.Antimicrob Agents Chemother2016; 60:2359–2365.
- SteggerM,WirthT,AndersenPSet al.Origin and evolution of European community-acquired methicillin-resistant Staphylococcus aureus.MBio2014; 5:e01044–14.
- ZhaoC,LiuY,ZhaoMet al.Characterization of community acquired Staphylococcus aureus associated with skin and soft tissue infection in Beijing: high prevalence of PVL+ ST398.PLoS One2012; 7:e38577.
- YuF,ChenZ,LiuCet al.Prevalence of Staphylococcus aureus carrying Panton-Valentine leukocidin genes among isolates from hospitalised patients in China.Clin Microbiol Infect2008; 14:381–384.