Abstract
Coronavirus disease 2019 (COVID-19) pandemic has significantly impacted the availability of cardiology services and management of cardiac conditions. Elective surgeries, outpatient appointments and cardiac imaging have been largely cancelled across the world due to the risk of infection transmission and the need for reallocation of resources to deal with the increasing number of COVID-19 patients. The impact on patients with cardiac co-morbidities during these times may be drastic. However, cardiologists and hospitals across the world have implemented measures to ensure on-going monitoring and care of patients remotely. In this review, we discuss the impact of COVID-19 on cardiac services including interventional cardiology services, cardiac imaging and outpatient appointments. In addition, implications for future research and clinical practice are also discussed.
Keywords:
Introduction
Coronavirus disease 2019 (COVID-19) pandemic has caused a state of alarm across the world. As of 7th June 2020, there have been over 6 million cases reported with >300,000 deaths globally [Citation1]. Pre-existing cardiovascular disease (CVD) has been associated with severe COVID-19 infection. The exact prevalence of CVD in COVID-19 patients is unknown; however, the prevalence has been reported to be 16.4% of CVD and 17.1% of hypertension in COVID-19 patients in China. [Citation2,Citation3]. COVID-19 patients with pre-existing CVD were reported to more likely to require intensive care unit admission [Citation2,Citation3]. Therefore, it is paramount that patients with pre-existing cardiac disease are continued to be monitored despite the rising pressure and burden on the healthcare system.
COVID-19 has significantly impacted hospital cardiology services in a number of different ways. The number of cardiology interventions has decreased worldwide over the past few months [Citation2,Citation4–6]. All elective, non-urgent procedures are currently cancelled, and medically fit in-patients are being discharged. These measures have been taken to allow resources to be reallocated to deal with COVID-19 patients and to reduce the risk of infection transmission. In this review, we discuss the impact of the COVID-19 pandemic on cardiology services such as cardiac imaging, interventional cardiology services and outpatient appointments. Implications for future clinical practice and research are also discussed.
Cardiac imaging
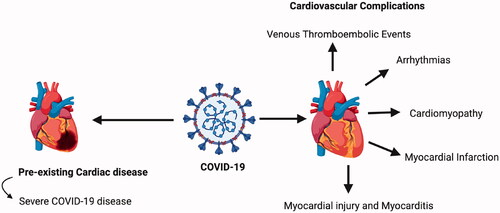
The potential cardiac complications of COVID-19 infection () in patients can increase the burden on cardiac imaging services [Citation3,Citation7]. The indication for cardiac imaging should be considered carefully to decrease the risk of infection from patient to patient, imager to patient and patient to imager [Citation7]. Imaging should only be performed if it is deemed necessary and is likely to change patient management or be lifesaving [Citation7,Citation8]. When requesting cardiac imaging, a number of factors should be considered. In patients with confirmed or suspected COVID-19, there is a potential risk of infection transmission to professionals and contamination of imaging equipment and facilities [Citation7]. Furthermore, there may be a risk of widespread contamination due to transportation of the critically ill or high-risk COVID-19 patients [Citation7]. It is also important to consider the consumption of personal protective equipment (PPE) by professionals carrying out the imaging and the time and resources needed to clean the equipment after use [Citation7]. In many countries, imaging for non-urgent or elective patients has been cancelled or postponed [Citation9]. However, cardiac imaging is still widely being requested in emergency departments and for in patients with acute cardiac decompensation [Citation7].
Due to the COVID-19 pandemic, there may be a change in the use of certain cardiac imaging modalities [Citation7]. COVID-19 patients can present with increased troponin levels associated with myocardial injury [Citation3,Citation10]. Compurterised Tomography (CT) angiography can possibly be used instead of invasive coronary angiography to confirm or exclude the diagnosis of acute coronary syndrome (ACS); this would help reduce exposure of COVID-19 to all members of the catheterisation lab [Citation7,Citation11].
Cardiac CT or magnetic resonance imaging (MRI) scans can also be used as alternatives to transesophageal echocardiography (TOE) due to increased risk of contamination of equipment and personnel with TOE [Citation7]. Furthermore, if TOE is indicated in a COVID-19 patient, it may be possible to perform a focussed cardiac ultrasound study (FoCUS) as an alternative [Citation7,Citation12]. FoCUS uses handheld or smaller lap-top-based scanners which are easier to cover, clean, and disinfect than larger machines [Citation12,Citation13]. Ideally, separate dedicated scanners exclusively for COVID-19 patients, that remain within designated COVID-19 areas should be considered [Citation7]. However, this is not possible in all centres. Therefore, it is paramount that cardiac imaging is performed if absolutely necessary and is likely to change patient management.
Cardiac imaging cancellation for non-COVID-19 patients can delay their diagnosis and treatment. Therefore, it is important that other ways to image patients remotely are put into place. For example, pocket-size ultrasound devices (PUDs) can be provided to patients with cardiac dysfunction, and their use can be directed off-site by cardiologists [Citation14]. These devices can be used to screen for left ventricular systolic dysfunction, left atrial enlargement, and elevated central venous pressure [Citation14]. Furthermore, to monitor and support the ongoing care of patients with congenital heart disease, software-based remote cardiac MRI services have been reported to be both feasible and successful in allowing ongoing management of these patients [Citation15]. Using devices and specific software that allow remote imaging will minimise disruption for patients. Furthermore, it will allow doctors to provide a real-time interpretation of images, diagnosis, guidance and treatment options to patients remotely.
Further investment of research, time and finances is necessary to establish remote cardiac imaging services that can allow ongoing care and management of patients with cardiac disease during this outbreak.
Interventional cardiology services
The COVID-19 pandemic has put an enormous strain on healthcare services and has significantly affected interventional cardiology facilities. Interestingly, there has been a reduction in hospital presentations of cardiovascular conditions such as ischaemic heart disease, decompensated heart failure and endocarditis [Citation16,Citation17,Citation18]. Although the exact impact on emergency cardiology services is unknown, reports highlight that there has been a reduction in emergency procedures during this pandemic [Citation18].
The diagnosis and treatment of ACS has been affected due to the shift in focus of healthcare systems towards caring for COVID-19 patients [Citation19]. A Consensus Statement from the American College of Emergency Physicians has highlighted that due to increasing bed pressures and increasing volume of COVID-19 patients, there may be delays in diagnosis and management of patients with ACS [Citation20].
The time taken for STEMI patients to present to hospital and the time taken to treat them has significantly increased. In Hong Kong, Tam et al. [Citation5] found that patients are presenting to hospital ∼319 min after symptom onset compared to ∼88 min prior to the pandemic; this is a significant increase of almost four times. [Citation5] Time of arrival in the catheterisation laboratory to successful wire crossing was also increased from ∼22 min pre-pandemic to 33 min post-pandemic [Citation5]. These delays may be attributed to limited staff availability due to illness with the COVID-19 infection and the need to don PPE which can be time-consuming.
The delay in patient presentation to hospital with conditions such as MI could be detrimental, possibly leading to out of hospital cardiac arrest. Analysis carried out in France highlighted that there was a 13% increase in out of hospital cardiac arrests [Citation21]. A proportion of these cases can be attributed directly to infection with COVID-19, however, in patients who tested negative for COVID-19 the indirect effect of the virus such as heightened public anxiety, perceptions that hospitals are areas of high infection transmission and reorganisation of the healthcare system may have contributed to the increase in out of hospital cardiac arrests. A study conducted to evaluate the use of the handheld ECG in India found it to be valuable in monitoring heart disease remotely [Citation22]. Such technology could be valuable for use with high-risk patients as it can allow for immediate examination and can help prevent patients going into cardiac arrest both in-hospital and out of hospital [Citation23]. Currently, the literature on the long-term impact of delaying interventional cardiology procedures due to the pandemic is limited. Future studies could evaluate the long-term effects of delaying interventional cardiology procedures and could help identify strategies to decrease their impact on cardiovascular morbidity and mortality.
Despite COVID-19's potential cardiac manifestations () and the association of viral infections with an increased rate of MI, current literature reports the number of PPCI’s has reduced internationally [Citation4,Citation3,Citation5,Citation24,Citation25,Citation26]. Rodríguez-Leor et al. reported that in Spain, there was a 48% reduction in PPCI during the pandemic compared to before the pandemic. The observed decrease in PPCI could be attributed to a reduction in available interventional cardiologists as 5% were reported to be infected with COVID-19 [Citation18]. Furthermore, reports from Austria showed a decline of 39.4% in admissions for PPCI due to ACS [Citation17]. Similarly, analysis in the United States (US) has estimated a 38% decrease in PPCI for STEMI treatment [Citation4]. Additionally, these findings were further highlighted by primary data collected from the cardiology department at Liverpool Heart and Chest Hospital. In order to maximise efforts to support COVID-19 patients, all elective coronary angiograms have been cancelled due to the risk of infection transmission and to prioritise emergency and urgent cases with severe coronary disease. It was found that the number of PPCI performed reduced from an average of 2.1 PPCI per day to 1.1 PPCI procedures during COVID-19 lockdown (between 23.03.2020 to 20.04.2020). There is no clear explanation for the reduction in PPCI. However, especially with the centralisation of services and anxiety surrounding the transmission of infection in hospital; it could be possible that patients are reluctant to call emergency services on symptom onset. It could be possible that elderly patients with atypical presentations of MI, ignore their symptoms thus fail to present to hospital.
Although the reasons underlying the decrease in PPCI are likely to be multifactorial, The primary cause of a reduction in PPCI appears to be due to delay in patients presenting to hospitals. Patients may perceive hospitals to be areas at high risk of COVID‐19 transmission and, therefore, delay presenting. However, it is also important to note that there could have been staff deployment or illness, which may have also contributed to the reduction in PPCI [Citation18,Citation27]. Furthermore, it can be proposed that the number of PPCI performed may be indirectly affected by behavioural changes in the general public. For example, a change in smoking habits with people smoking less due to fear that smoking could increase their risk of infection [Citation28]. During this period, in which health is even more important than usual, people may try to adopt healthier lifestyles which would decrease the risk of MI and hence PPCI.
During the COVID-19 pandemic PPCI has remained the standard treatment for STEMI patients at hospitals which are capable of performing PPCI in a time-efficient manner with the appropriate PPE. The American College of Emergency Physicians has suggested that thrombolysis could be administered prior to PPCI for STEMI patients in hospitals where there are limited PPCI facilities or if PPCI is not feasible. During this pandemic, administration of thrombolysis prior to PPCI has been shown to be valuable in STEMI patients as indicated by reports from the Sichuan hospital in China [Citation20]. Thrombolysis may be useful in patients presenting with ACS in regions with limited or over-whelmed cardiac facilities, or where PPCI cannot be performed within 120 min. Updating thrombolysis protocols, ensuring hospitals are fully stocked with thrombolytics as well as staff training will promote efficient management of patients with STEMI [Citation29]. Optimising medical management of cardiac emergencies is paramount during this pandemic as it would help discharge patients quickly, reduce bed pressures and the risk of transmission of infections.
Surgical procedures for patients with structural heart disease (SHD) have also been affected. The guidance issued by the Centre for Medicare and Medicaid Services(CMS) in the United States has recommended limiting cardiac surgical procedures to 'highly symptomatic patients' [Citation30]. As a result, a number of [Citation31]aortic valve replacement surgeries for low-risk patients have been delayed. Tanguturi et al. have suggested that patients with aortic stenosis should be monitored via virtual assessments every 1–3 months to assess disease progression and treatment should be delayed until the pandemic subsides [Citation32]. However, the risk of delaying treatment should be balanced against the risk of patient exposure to infection and current resource limitations[Citation33].
Outpatient appointments
Many patients frequently visit the hospital for treatment and monitoring of disease progression. Due to the increased risk of severe infection in patients with cardiac co-morbidities, all outpatient procedures and appointments have been cancelled to reduce face-face contact [Citation31,Citation34].
The role of telemedicine and remote consultations is of considerable importance during the current pandemic [Citation35]. The European Society of Cardiology strongly encourages the use of telemedicine, especially in vulnerable groups such as older patients [Citation8]. Telemedicine encompasses virtual video and telephone visits, as well as home monitoring tools [Citation36,Citation37]. There are several telemedicine platforms available to healthcare providers, each of which can be tailored to the patient's needs [Citation35,Citation37,Citation38]. Telemedicine can allow adequate monitoring and management of patients remotely while reducing the risk of transmission of infection. Telemedicine platforms can also be used to provide training to medical staff.
Patients with chronic conditions such as heart failure (HF), if not closely monitored, are at risk of acute cardiac decompensation [Citation39]. HF patients can be monitored by use of telehealth programmes and equipping patients with monitors that can communicate information directly to care providers. The use of telemedicine has shown similar health outcomes compared to face-to-face appointments for HF patients [Citation37]. The Heart Failure Society of America suggests that Virtual Visits (VV) can be potentially offered to patients with HF [Citation40]. Virtual visits (VV) allow real-time interaction between patient and clinician and have the potential to save time and cost; they have also been reported to improve patient satisfaction which was related to the convenience of avoiding travel to health care centres [Citation41–43]. Gorodeski et al. reported that VV's had decreased no-show rate compared to in-person appointments with no significant difference in hospital readmissions, emergency department visits or deaths between the two study arms [Citation40].
In addition to the reduced exposure to COVID-19, there are several advantages of VV. Some patients find it easier to have discussions about their healthcare in the presence of their family members which may not be available for in-hospital appointments [Citation40]. From a healthcare system perspective, VV can allow reallocation of resources and increased focus on in patient services which are at risk of becoming overwhelmed due to the rapidly increasing number of COVID-19 patients [Citation40]. Despite the advantages of VV, there are several challenges in providing virtual care. Patients may feel uncomfortable with using technology or may have limited access to internet or smart devices/laptop. In addition, patients may also feel concerned about patient confidentiality in virtual appointments. From a clinician's perspective, VV's present a barrier to full physical examination and therefore, clinicians may feel as though the examination is not adequate compared to in patient visits. Providing education and reassurance to patients about telemedicine is important, as it would help reduce technical difficulties and ensure that patients are still receiving adequate ongoing care.
Some conditions cannot be appropriately diagnosed via VV's such as structural or valvular heart disease and would require an in-person assessment. In the UK, home care and mobile clinics are also currently proposed to prevent unnecessary movement of patients between hospitals; this would help prevent clinical deterioration of patients with cardiac disease and assure patient adherence to treatment [Citation8]. Nurses and physicians would need to wear appropriate PPE if delivering home care or mobile clinic services.
Telemedicine also has a significant role in cardiac rehabilitation. Over 30 trials investigating the role of telemedicine in a cardiac rehabilitation setting have been published [Citation44]. Results from a systematic review of these trials showed that there was a reduction in hospitalisation and cardiac events (risk ratio 0.56) with telemedicine compared with 'normal' cardiac rehabilitation; highlighting the efficacy of delivering cardiac rehabilitation remotely [Citation44]. In addition, the ubiquitous use of the internet and smartphones in telemedicine makes it more accessible to track patients progress; this will ensure that patients are adequately monitored.
There have been several advancements in cardiac telemedicine due to the rising demand for healthcare professionals to provide remote care. For example, patients with atrial fibrillation (AF) can be monitored using a programme called TeleCheck-AF [Citation45]. Telecheck-AF contains a smartphone application (FibriCheck) that uses the patient's index finger and the phone's camera to detect the patient's pulse. FibriCheck uses an algorithm to identify AF and abnormalities in the patient's heart rate; this data can then be used by the doctor to guide teleconsultations and to monitor treatment remotely [Citation45].
Despite telemedicine being easily accessible, it is currently not widely used, and therefore institutions should be encouraged to utilise these technologies to optimise patient care. Telephone consultations are an alternative to VV's. The method of remote care needs to be discussed between the patient and clinician and should be tailored individually to the patient to meet their medical needs [Citation40]. There are several limitations of telemedicine, however, it is important to optimise the current methods to allow quality management of patients remotely.
Implications for future clinical practice and further research
Due to the suspension of routine cardiovascular care, there may be an increase in cardiac hospital admissions, morbidity and mortality associated with chronic cardiac conditions post-outbreak. In particular, vulnerable groups such as diabetics, elderly and those with previous cardiac surgeries and renal failure may face additional complications that will need to be addressed. It is estimated that more than 50% of elective surgical cases could result in progressive cardiac deterioration due to postponement or cancellation of elective surgery [Citation46]. The postponement or cancellation of surgery can lead to lower quality of life, exacerbation of symptoms and increase in emergency hospital admissions after the pandemic. Therefore it is important to develop strategies to accommodate this expected rise in demand post-pandemic. The novel strategies developed during the pandemic, such as VVs might be more commonly employed post-pandemic to deal with the significantly higher demand for cardiovascular care. Further investment of research and finances is needed to develop software or devices to optimise remote care of patients with cardiovascular disease.
Due to the anticipated rise in demand for cardiovascular services post-pandemic, it becomes increasingly important to risk-stratify patients in order to identify high-risk patients in need of urgent intervention in the post pandemic era. Stahel et al. proposed a scoring system for elective surgeries after a blanket cancellation order was submitted by the American College of Surgeons [Citation46]. Adapting and implementing such a system to elective cardiac surgeries could assist in determining the urgency of cases and ensuring patient safety[Citation47,Citation48]. Risk scoring systems and algorithms may also be beneficial to risk-stratify patients with chronic conditions as well as emergency admissions. These measures will help to alleviate the pressure on an overwhelmed healthcare system.
COVID-19 pandemic has provided an excellent opportunity to reflect on our current healthcare system and clinical practice. The timely and efficient decision-making strategies utilised during the COVID-19 pandemic has highlighted the importance of well-organised protocols. As further research emerges, non-invasive treatment approaches may be used more frequently for cardiac conditions such as ACS, if supported by retrospective cohort studies. Furthermore, careful and meticulous analysis of epidemiological data will help exclude non-essential services, reducing financial pressure on the healthcare systems in addition to developing novel strategies for future pandemics. A summary of the impact of COVID-19, mitigating strategies, their consequences and long-term impacts is summarised in .
Figure 2. Summary of the impact of COVID-19 on cardiology services, mitigating strategies, their consequences and potential long-term effects.

To avoid huge impacts on cardiology services in future pandemics, optimisation of telemedicine services is paramount. In addition, training staff and patients to use telemedicine and remote healthcare facilities is also essential. In future pandemics, early communication and reassurance to patients that hospitals can provide adequate cardiac healthcare while ensuring infection control policies are met is vital; this will help to reduce anxiety and fear in patients. Home care and mobile clinics could also be offered to patients; this will help to reduce the delays in diagnosis and treatment. Furthremore, although it would require significant changes to healthcare infrastructure and organisation, recruiting more staff and increasing hospital capacity may be useful in relieving the increased pressure on healthcare services in future pandemics. Moreover, a change in healthcare bureaucracy and training junior cardiologists to make decisions which would otherwise be made by seniors would also beneficial. All these measures will help healthcare providers become better equipped and reduce the impact on cardiology services in future pandemics.
Conclusion
COVID-19 has caused an enormous impact on cardiac healthcare services worldwide. The pandemic has accelerated the movement towards telemedicine due to the rising demand for remote healthcare. Utilising emerging telemedicine facilities may help to alleviate stress on overstretched healthcare systems. However, further research and financial investment are required for the development of effective telemedicine services. Ultimately, it will be necessary to follow-up and risk stratify patients post-pandemic to evaluate the long-term impact of the delays in diagnosis and treatment on overall patient health. Further research is required to fully evaluate the effect of the COVID-19 pandemic on cardiology services and the benefit of current mitigating strategies.
Disclosure statement
The authors have no conflicts of interest to declare.
References
- Who.int. 2020 [Accessed 2020 Jun 8]. Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200606-covid-19-sitrep-138.pdf?sfvrsn=c8abfb17_4.
- Li B, Yang J, Zhao F, et al. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol. 2020;109(5):531–538.
- Long B, Brady W, Koyfman A, et al. Cardiovascular complications in COVID-19. Am J Emerg Med. 2020. [published online ahead of print]. DOI:https://doi.org/10.1016/j.ajem.2020.04.048
- Garcia S, Albaghdadi M, Meraj P, et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75(22):2871–2872.
- Tam C, Cheung K, Lam S, et al. Impact of Coronavirus Disease 2019 (COVID-19) outbreak on ST-segment–elevation myocardial infarction care in Hong Kong. Circ Cardiovasc Qual Outcomes. 2020;13(4):1–3.
- Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. The Lancet. 2020;395(10229):1054–1062.
- Skulstad H, Cosyns B, Popescu B, et al. COVID-19 pandemic and cardiac imaging: EACVI recommendations on precautions, indications, prioritization, and protection for patients and healthcare personnel. Eur Heart J Cardiovasc Imaging. 2020;21(6):592–598.
- Escardio.org. ESC Guidance For The Diagnosis And Management Of CV Disease During The COVID-19 Pandemic; 2020 [Accessed 2020 Jun 8]. Available from https://www.escardio.org/Education/COVID-19-and-Cardiology/ESC-COVID-19-Guidance#p06.
- DAIC. Cardiac imaging best practices during the COVID-19 pandemic; 2020[Accessed 2020 Jun 8]. Available from: https://www.dicardiology.com/article/cardiac-imaging-best-practices-during-covid-19-pandemic.
- Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet. 2020;395(10223):497–506.
- European Heart Journal. Corrigendum; 2019.
- Neskovic A, Skinner H, Price S, et al. Focus cardiac ultrasound core curriculum and core syllabus of the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2018;19(5):475–481.
- Cardim N, Dalen H, Voigt J, et al. The use of handheld ultrasound devices: a position statement of the European Association of Cardiovascular Imaging (2018 update). Eur Heart J Cardiovasc Imaging. 2019;20(3):245–252.
- Mai T, Ahn D, Phillips C, et al. Feasibility of remote real-time guidance of a cardiac examination performed by novices using a pocket-sized ultrasound device. Emerg Med Int. 2013;2013:1–5.
- Garg R, Sevilla A, Garberich R, et al. Remote delivery of congenital cardiac magnetic resonance imaging services, a unique telemedicine model. J Cardiovasc Magn Reson. 2015;17(S1):226–232.
- Bhf.org.uk. Lives at risk due to 50% drop in heart attack A&E attendances; 2020 [Accessed 2020 Jun 8]. Available from https://www.bhf.org.uk/what-we-do/news-from-the-bhf/news-archive/2020/april/drop-in-heart-attack-patients-amidst-coronavirus-outbreak.
- Metzler B, Siostrzonek P, Binder R, et al. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. Eur Heart J. 2020;41(19):1852–1853.
- Rodríguez-Leor O, Cid-Álvarez B, Ojeda S, et al. Impact of the COVID-19 pandemic on interventional cardiology activity in Spain. RECICE. 2020;2(2):82–89.
- Zhang S. What it really means to cancel elective surgeries. The Atlantic; 2020 [Accessed 2020 Jun 7]. Available from: https://www.theatlantic.com/science/archive/2020/03/patients-whose-surgeries-are-canceled-because-coronavirus/608176/.
- Mahmud E, Dauerman H, Welt F, et al. Management of acute myocardial infarction during the COVID‐19 pandemic. Catheter Cardiovasc Interv. 2020. [published online ahead of print]. DOI:https://doi.org/10.1016/j.jacc.2020.04.039
- Marijon E, Karam N, Jost D, et al. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France: a population-based, observational study. Lancet Public Health. 2020;2667(20):1–7. DOI:https://doi.org/10.1016/S2468-2667(20)30117-1
- Singh M, Agarwal A, Sinha V, et al. Application of handheld tele-ECG for health care delivery in rural India. Int J Telemed Appl. 2014;2014:981806–981806.
- Kapoor A, Pandurangi U, Arora V, et al. Cardiovascular risks of hydroxychloroquine in treatment and prophylaxis of COVID-19 patients: a scientific statement from the Indian Heart Rhythm Society. Indian Pacing Electrophysiol J. 2020;20(3):117–120.
- Kwong J, Schwartz K, Campitelli M, et al. Acute myocardial infarction after laboratory-confirmed influenza infection. N Engl J Med. 2018;378(4):345–353.
- Welt F, Shah P, Aronow H, et al Catheterization laboratory considerations during the Coronavirus (COVID-19) pandemic: from the ACC's interventional council and SCAI. J Am Coll Cardiol. 2020;75(18):2372–2375.
- Khan IH. Savarimuthu S.Leung MST. Harky A. The need to manage the risk of thromboembolism in COVID-19patients J Vasc Surg. 2020;S0741–5214(20):31157. [published online ahead of print].DOI:101016/jjvs202005.015
- Khan I H, Zahra S A, Zaim S, et al. At the heart of COVID-19. Journal of Cardiac Surgery. J Card Surg. 2020;35(6):1287–1294. DOI:https://doi.org/10.1111/jocs.14596.32369872
- López-Bueno R, Calatayud J, Casaña J, et al. COVID-19 confinement and health risk behaviors in Spain. Front Psychol. 2020;11: 1426. DOI:https://doi.org/10.3389/fpsyg.2020.01426.
- Medscape. What UK cardiologists need to know about COVID-19; 2020 [Accessed 2020 Jun 8]. Available from: https://www.medscape.com/viewarticle/927236.
- Cms.gov. 2020 [Accessed 2020 Jun 7]. Available from: https://www.cms.gov/files/document/cms-non-emergent-elective-medical-recommendations.pdf.
- Collins GB, Jenner WJ, Kaier TE, et al. COVID-19: A United Kingdom National Health Service cardiology perspective. JACC Case Rep. 2020. [published online ahead of print]. DOI:https://doi.org/10.1016/j.jaccas.2020.04.024
- Tanguturi V, Lindman B, Pibarot P, et al. Managing severe aortic stenosis in the COVID-19 era. JACC Cardiovasc Interv. 2020.[published online ahead of print]. DOI:https://doi.org/10.1016/j.jcin.2020.05.045
- Yoganathan A, Sajjad MS, Harky A. Cardiovascular disease and the impact of COVID-19 . J Card Surg. 2020. [published online ahead of print].DOI:https://doi.org/10.1111/jocs.14682.
- Al-Jabir A, Kerwan A, Nicola M, et al. Impact of the Coronavirus (COVID-19) pandemic on surgical practice - Part 1. Int J Surg. 2020;79:168–179.
- Portnoy J, Waller M, Elliott T. Telemedicine in the Era of COVID-19. J Allergy Clin Immunol Pract. 2020;8(5):1489–1491.
- Elliott T, Yopes M. Direct-to-consumer telemedicine. J Allergy Clin Immunol Pract. 2019;7(8):2546–2552.
- Flodgren G, Rachas A, Farmer A, et al. Interactive telemedicine: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2015;Art. No.:(9), 1–583. https://doi.org/https://doi.org/10.1002/14651858.CD002098.pub2.www.cochranelibrary.com
- Bashshur R, Shannon G, Krupinski E, et al. National telemedicine initiatives: essential to healthcare reform. Telemed J E Health. 2009;15(6):600–610.
- Reza N, DeFilippis E, Jessup M. Secondary impact of the COVID-19 pandemic on patients with heart failure. Circ Heart Failure. 2020;13(5):11–13. DOI:https://doi.org/10.1161/CIRCHEARTFAILURE.120.007219
- Gorodeski E, Goyal P, Cox Z, et al. Virtual visits for care of patients with heart failure in the era of COVID-19: a statement from the Heart Failure Society of America. J Card Fail. 2020;26(6):448–456.
- Tasneem S, Kim A, Bagheri A, et al. Telemedicine video visits for patients receiving palliative care: a qualitative study. Am J Hosp Palliat Care. 2019;36(9):789–794.
- Thiyagarajan A, Grant C, Griffiths F, et al. Exploring patients' and clinicians' experiences of video consultations in primary care: a systematic scoping review. BJGP Open. 2020;4(1):bjgpopen20X101020.DOI:https://doi.org/10.3399/bjgpopen20X101020
- White T, Watts P, Morris M, et al. Virtual postoperative visits for new ostomates. Comput Inform Nurs. 2019;37(2):73–79.
- Thomas E, Gallagher R, Grace S. Future-proofing cardiac rehabilitation: transitioning services to telehealth during COVID-19. Eur J Prev Cardiol. 2020:1–2.
- Klompstra L, Jaarsma T. Delivering healthcare at distance to cardiac patients during the COVID-19 pandemic: Experiences from clinical practice. Eur J Cardiovasc Nursing. 2020;1–2.
- Stahel P. How to risk-stratify elective surgery during the COVID-19 pandemic? Patient Saf Surg. 2020;14(1):8.
- Mohamed Abdel Shafi A, Hewage S, Harky A.The impact of COVID-19 on the provision of cardiac surgical services. J Card Surg. 2020;35(6):1295–1297. DOI:https://doi.org/10.1111/jocs.14631.
- Yoganathan A, Sajjad MS, Harky A.Cardiovascular disease and the impact of COVID-19. J Card Surg. 2020. [published online ahead of print]. DOI:https://doi.org/10.1111/jocs.14682.