Abstract
Objective: To analyse the lifetime monetary and health related effects of the consumption of sugar-free chewing gum.
Material and methods: Using a Markov model we assumed that the German consumption of sugar-free chewing gum (111 gums/year) could be elevated to the level of Finland (202 gums/year). The calculation was based on a model patient representing the development of oral health from the age of 12 to 74 years and clinical data on the effectiveness of chewing sugar-free gum. Lifetime and yearly costs for the ‘Finland-scenario’ were determined and compared with the actual German expenses of the statutory health insurance companies for dental health.
Results: The actual total lifetime expenditures of the statutory health insurance companies are 17,199.96€ per capita and would be 12,188.94€ in the scenario with elevated consumption of sugar-free chewing gum in Germany. Thus, 5011.02€ per capita could be saved in a lifetime and 80.82€ per year.
Conclusions: On a national scale, the elevation of the consumption of sugar-free chewing gum in Germany to the level of Finland would lead to a considerable benefit for cost saving and oral health for the statutory health insurance companies.
Introduction
In Germany, a considerable caries decline was observed in the last two decades in children. As an example, caries declined in 12-year olds from DMFT 4.1 in 1989 to 0.7 in 2005, corresponding to a prevented fraction of 82.9% [Citation1,Citation2]. This was mainly due to the widespread use of fluorides in various application forms [Citation3]. However, caries prevalence in adults and seniors as well as its economic burden is still high. Last available data show a DMFT of 22.1 for 65- to 74-year olds [Citation2] and expenditures of 7.86 billion €/year for the treatment of caries [Citation4]. Therefore, additional preventive measures are required. Preferably, low-threshold preventive measures could help to face this problem. The success of such preventive measures which also include condition oriented prevention instead of behaviour oriented prevention is documented. For example, there is broad evidence for the benefit of water fluoridation [Citation5]. However, water fluoridation is discussed controversially since it impairs the freedom of choice [Citation6]. Other effective population-targeted fluoridation methods like fluoridated salt or milk are limited to few countries worldwide [Citation7] or to school-based programs [Citation8]. Since there are no legal restrictions as with fluoride, the consumption of sugar-free chewing gum could be a preventive measure with a worldwide public dental health perspective. Its caries preventive effect has been demonstrated in several clinical trials [Citation9–20]. Although not condition-oriented, the chewing of sugar-free gum is a low-threshold caries preventive method since it is not primarily used because of a health concern. Therefore, it can be argued that also high-risk groups with low socioeconomic status could be reached and that it could help to reduce oral health inequalities. Since the consumption of sugar-free chewing gum is effective in caries prevention and does not burden the health care system, it could be a cost-effective public health measure when used additionally to regular oral hygiene measures. However, its potential is not yet fully exploited in Germany. In comparison, the per capita consumption of chewing gum in Finland is about twice as much (202 vs. 111 servings) (Wrigley Company. Personal Communication 2017). Basis of the ‘per capita consumption’ is the entire population from birth to death. Therefore, it was the aim of the present study to analyse the cost-effectiveness of an elevation of the consumption of sugar-free chewing gum to the level of Finland.
Material and methods
A cost-minimization analysis was performed to compare the caries preventing effect of sugar-free chewing gum and related cost-savings of two different chewing scenarios within Germany: the current use of sugar-free gum and the increased consumption of sugar-free gum (according to Finnish level). The analysis was conducted to determine outcomes at the individual level. Monetary effects and health related outcomes were considered using a Markov model.
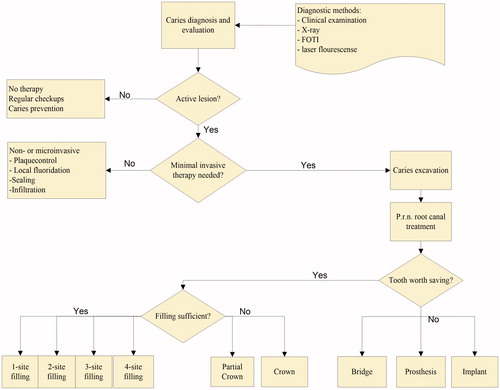
In order to determine the mean relative risk reduction for caries, a pragmatic literature review was performed in PubMed with the search terms ‘gum’ and ‘caries’, limited to studies published since 1985. A manual search provided further studies conducted before 1985. Inclusion criteria were the presence of a control group (no gum or sweetened gum), the assessment of a clinical impact after multiple chewing occasions and provision of a value for caries reduction. Thirty-three studies remained after screening of title and abstract. As none of the studies was conducted in Germany, the most transferable ones were selected for the meta-analysis. Fifteen studies were included based on full text review and 12 were finally identified to estimate the risk reduction of caries by sugar-free gum [Citation9–20]. The mean relative risk reduction for caries was found to be 5.38%. This value was adjusted to the different consumption levels of Germany and Finland, averaged for the whole population, and used in the Markov model to calculate the transition probability for a tooth to stay caries-free. It was the aim to determine the improvements in oral health and the resulting cost savings for the German statutory health insurance if the consumption of sugar-free chewing gum would be increased to the level of Finland. Latest available data show a total chewing gum consumption of 202 serving units per capita and year in Finland and 111 in Germany (see “Wrigley Company. Consumption of chewing gum in Finland and Germany, Personal Communication, 2014”). One serving unit corresponds to one chewing gum strip or 1.5 pellets. This definition was made to make comparable the consumption of strips and pellets. While usually only one strip is consumed at once pellets are chewed in portions of one or two. On behalf of Wrigley’s, these data were collected by Nielsen, an international market research company (http://www.nielsen.com). The data include all sugar-free and sugar containing chewing gums in the two countries. Overall, the proportion of sugar containing chewing gum is low in both countries (less than 15%), but lower in Germany (see “Wrigley Company. Consumption of chewing gum in Finland and Germany, Personal Communication, 2014”). Therefore, to be conservative, the ratio of 1.82 (202/111) was used for the present analysis and applied for a lifelong observational period. Consequently, the calculation is based on the assumption that the use of sugar-free chewing gum in Germany would increase from 111 pieces a year to 202. In order to determine the cost-effectiveness for an individual patient, a clinical pathway for the treatment of caries and its complications in Germany was developed (Figure 1). Since no relevant treatment guidelines for Germany were available from professional associations, the treatment pathway was derived from relevant textbooks [Citation21–23]. Based on this pathway, the Markov model was generated.
Compared scenarios and model patient
The development of dental health including restorations based on the treatment pathway () was projected on a time horizon of 62 years (62 cycles of one year each), representing the development from the age of 12 to 74 years. For these ages, data are available from the fourth German Oral Health Survey (DMS IV) [Citation2]. These data allow evaluation of the development over almost a lifetime from the complete eruption of the permanent dentition of a 12-year old to the dental situation of a senior person.
According to the DMS IV, the DMFT in 12-year olds is 0.7 (DT = 0.2, MT = 0.0, FT = 0.5) and in 65- to 74-year olds is 22.1 (DT = 0.3, MT = 14.1, FT = 7.7) [Citation2]. Development of caries, tooth loss and restorations was modelled between the endpoints of this lifespan (12 and 74 years) using transition probabilities described below. Although start and end DMFTs were used to calculate transition probabilities, the natural and treatment history of a carious tooth is complex and different states might change at different times with different probabilities. However, the assumptions utilized in this model seem reasonable for research design. Furthermore, according to our knowledge, there is no literature that describes the specific transitioning from one tooth state to another.
In order to verify the fit of the model, data from 40-year-olds from the same survey were used. Using values from the DMS IV study and modelling the run of DMFT values over the life span we estimated the average DMFT after the time horizon of 62 years. As a next step, we extrapolated values (known from the DMS IV) of decayed, missing and filled teeth and identified the percentage of teeth not affected, affected by fillings, affected by crowns and affected by bridges/prostheses/implants to the estimated DMFT at age 74 (62 years older than 12, which was taken as the start-off age for the model). This allowed us to solve the equation of the transitional probabilities so that the DMFT after 62 periods in our model equalled the estimated DMFT as well as the percentages of teeth not affect, affected by filling, affected by crowns and affected by bridges/prostheses/implants.
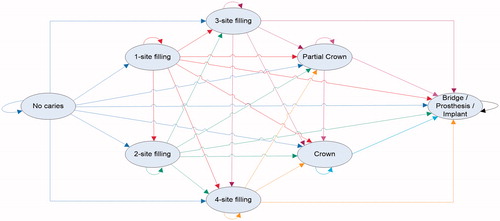
In order to define the share of FT and MT in the teeth affected by caries, the ratio of FT, MT and no caries for the age group of 65- to 74-year-old people is considered, which results in the distribution of dental states as described in . To assign probabilities to the possible transitions described in , we first used the information that 20.32% of the time the analysed tooth is not affected by caries after 62 cycles. The transitional probability for a tooth to stay in the state ‘No caries’ for one cycle is therefore calculated as 97.46% by solving the equation x62 = 20.32% for x.
Table 1. Distribution of the dental condition at age 74.
Table 2. Costs for medical services refunded by the statutory health insurance companies in Germany.
To define transitional probabilities for the other states, the following mathematical conditions were imposed:
The chance of remaining in one state is always greater or equal to the chance of transitioning to the next state, which is always greater than the chance of transitioning to the second next stage and so on.
The probability of a crown after 62 cycles equals the probability of a partial crown.
The cumulative probability of the tooth being in one of the states 1-, 2-, 3- or 4-surface filling, crown or partial crown is 28.14%.
The probability of a tooth being in the state bridge, prosthesis or implant equals 51.54%.
In order to define the share of FT and MT in the teeth affected by caries, the ratio of FT, MT and no caries for the age group of 65- to 74-year-old people is considered.
By applying these conditions, the transitional probabilities can be solved using MS Excel Solver. As a next step, separate distributions for both one molar and one anterior tooth need to be defined so that the combination of both distributions equals the overall model. Since the human permanent dentition consists of 16 posterior teeth (without third molars) and 12 anterior teeth, relative weights of 16/28 for posterior and 12/28 for anterior teeth for each distribution are the result. On the basis of clinical experience, one out of the six remaining teeth at the age of 74 is a molar and five are anterior teeth. Transitional probabilities for posterior and anterior teeth can be calculated separately, on the basis of the described considerations so that the combined and weighted distribution of probabilities corresponds to the overall model. Transitional probabilities from one tooth state to another may vary depending on age of teeth or other parameters.
The analysis was carried out for the current German scenario (sugar-free gum Germany: sfgG) and the scenario based on a consumption of sugar-free gum increased to the level of Finland (sugar-free gum Finland: sfgF). The model patient used as the starting point of the projection was defined on the basis of the representative data from the fourth German Oral Health Survey (DMS IV) [Citation2]. According to this, the model patient showed the following characteristics which were used as starting point and descriptive circumstances:
12-year old.
DMFT: 0.7.
Fissure sealing in 2.7 teeth.
Teeth brushed at least twice a day.
At least one dental appointment per year.
Health insurance: statutory health insurance.
On the basis of the DMFT value, it was assumed that the model patient had one filling in a molar. Furthermore, we considered that each patient in both scenarios maintained his or her habits in oral hygiene (tooth brushing at least twice a day, regular dental appointments). In the sfgF scenario, patients additionally consumed more sugar-free gum. In both scenarios, the risk of caries was modelled per single tooth. Results then were extrapolated to the entire dentition. To address the different risks for the appearance of primary or secondary caries as well as localization and severity, the model differentiated between front and posterior teeth. Assuming caries on one tooth, one posterior tooth (molar) was already in the status ‘one-site filling’ at the beginning of the evaluation. All other teeth were attributed to the status ‘no caries’.
Model and states
The effectiveness of the sfgF scenario was measured in terms of its ability to prevent caries and/or its consequences. Eight states were defined depending on the prevalence of caries, its severity and possible consequence (). In the state ‘No caries’, no treatment is required. For the calculation of the DMFT, the tooth counts with DMFT = 0. All following states count with DMFT = 1. If caries occurs and no denture is needed, the tooth passes to one of the states ‘1-site filling’, ‘2-site filling’, ‘3-site filling’ or ‘4-site filling’. It was assumed that all lesions are treated in the same cycle. Depending on the risk, root canal treatment may also be necessary. If the tooth is too weak to be restored with a filling, a crown is needed. In this case, the tooth passes to the state ‘partial crown’ if there is enough dental substance. Transition into the state ‘full crown’ takes place if the substance loss reaches the gum. Before placing a crown, fillings must be removed and root canal treatment must be completed. If fillings and crowns are no longer adequate and the tooth has to be extracted, it passes to the state ‘B/P/I’ (Bridge/Prosthesis/Implant). The tooth remains in its respective state as long as there is no progression of the destruction. Transition to more severe caries-related states is possible, depending on the progression of the disease after every cycle. As lost natural tooth substance cannot be regained, transition to less severe conditions is not possible. All calculations were conducted with Microsoft Excel and TreeAge Pro 2012.16. shows the model and the transitional probabilities.
Costs
Costs were calculated from the perspective of the German statutory health insurance system based on BEMA (Assessment Standards for Dental Services) and the subsidies for prosthetic restorations [Citation24]. The BEMA is a kind of a mandatory price list for all essential dental services for members of the statutory health insurances, which account for 85.5% of all German citizens [Citation25]. Health services are directly discounted with the statutory health insurance companies. All expenditures for caries and its consequences are included. All costs were adjusted by the inflation and calculated based on the price level of 2013. According to national standards, a discount rate of 3% was chosen. shows the costs considered in our model.
Results
The results of the analysis for one single front or posterior tooth are displayed in . The table shows the average costs per tooth and the probability of certain states, that is being restored by filling, partial crown or crown, or being replaced by bridge, prosthesis or implant. In both scenarios, a front tooth caused less average lifetime costs (413.82€ for sfgG vs. 188.43€ for sfgF). In contrast, lifetime costs for a posterior tooth were higher (754.18€ for sfgG vs. 604.02€ for sfgF). These differences are reflected by the observation that a front tooth had a higher lifetime probability to stay caries free (41.67% for sfgG vs. 47.75% for sfgF). The respective probabilities for a posterior tooth to stay caries free after 62 cycles were considerably lower (4.06% for sfgG vs. 8.54% for sfgF). The scenario of elevated consumption of sugar-free gum had a high impact on the risk of a tooth being replaced (front tooth: 37.73 for sfgG vs. 7.33 for sfgF; posterior tooth: 60.13 for sfgG vs. 46.43 for sfgF). shows the cumulative results for the entire dentition and therefore gives the total lifetime and yearly costs that can be saved by an elevated consumption of sugar-free gum. The actual total lifetime costs per capita are 17,199.96€ and would be 12,188.94€ in the scenario where the consumption of sugar-free chewing gum in Germany (sfgG) could be elevated to the status of Finland (sfgF). Thus, 5011.02€ per capita could be saved in a lifetime and 80.82€ per year.
Table 3. Average costs per tooth and the probability of certain states, that is being restored by filling, partial crown or crown, or being replaced by bridge, prosthesis or implant.
Table 4. Cumulative states of teeth and total lifetime and yearly costs for the two scenarios (sfgG, sfgF).
Health-related outcomes can also be seen in . As a main result, the elevated use of sugar-free gum results in six additional teeth that do not have to be replaced by bridges, prostheses or implants. Statistically, five of these teeth move to filled and another one to caries free teeth.
Discussion
The present study could demonstrate that an elevation of the consumption of sugar-free chewing gum could result in a considerable cost saving of the statutory health insurance companies in Germany and an improved oral health status. The cost saving is 29.13% whereas the assumed caries preventive effect was only 5.38%. This can be explained by the fact that both effects are not linear proportional. A slight reduction in caries initiation and progression might considerably reduce the expenses for restorations. This can be seen in . The main benefit was not a considerable increase in healthy teeth but a reduction of large and expensive restorations.
In the present study, it could not be differentiated between chewing gums with different sugar substitutes. However, according to the literature, polyols such as Xylitol, Sorbitol, Maltitol, Mannitol and Erythritol do not seem to have a different effectiveness with respect to caries reduction [Citation26–29].
The question how to realize the elevation of the consumption of sugar-free gum was not an issue of this study. It was only the aim to analyse whether this could be cost- and health-effective. Since this effect could be demonstrated, the next step could be to implement the elevated chewing gum consumption. This could be realized by public information campaigns, for example by oral health organizations. Such a campaign was already successfully realized by the Finnish Dental Association for the use of xylitol, a sugar substitute [Citation30].
In Germany, there is no legal or cultural obstacle against sugar-free chewing gum. However, although there is a public awareness of its caries preventive effect, the use of sugar-free chewing gum is not promoted in most schools due to the fear of littered gum in schoolyards, playgrounds and school furniture. Therefore, a chewing gum promotion campaign would also have to address this issue.
It is a limitation of the analysis that a model patient has been modelled on retrospective data, because dental hygiene and dental health has changed remarkably over the past 40 years. However, we decided to take the values at hand rather than model values ourselves, which again would have had to be based on certain assumptions.
Expenses for chewing gum were not included in the calculation because they are not health-care expenses, even though the consumption has an effect on oral health. Furthermore, expenses for chewing gum are a private matter only the savings from healthcare expenses related to the statutory health insurance should be analysed in the present study. In Germany, the price for a sugar-free chewing gum averages between 1.5 and 9.75€cent. This means, that an increase in the consumption from 111 to 202 chewing gums per year would result in actual costs of 1.36€ to 8.87€ per capita and year.
The costs associated with the clean-up of littered gum have not been included in the model as this exceeded the scope of the specific analysis. However, the removal of irresponsibly disposed chewing gum can be difficult and expensive. In Singapore, chewing gum was banned for a period of time and remains under sales channel restrictions, allowing only dental or nicotine chewing gums [Citation31]. As all data had been derived from official statistical databases, these real-world data did not undergo a sensitivity analysis [Citation2,Citation32]. The data taken for cost calculation is based on the official reimbursement of dental services. There are no other data sources for these parameters in Germany. The same applies for the transition probabilities. There is no other source then the DMS IV for the data required in this model. There may be variations in the transitional probabilities, but performing a sensitivity analysis is problematic, because transitional probabilities have to add up to one at all stages of the model. Hence, adjusting one transitional probability would result in a required change of further transitional probability parameters, because values depend on one another.
More important than the cost saving however is the increase in dental health that could be reached by this measure. This could be underestimated if looking only at caries-free teeth. As shown in , the number of caries-free teeth increases only slightly from six to seven in the scenario with elevated consumption of sugar-free chewing gum. But more important is the reduction of the number of lost teeth that have to be replaced by bridges, prosthesis or implants. On average, this number could be reduced from 14 to 8 per individual. The average consumption of sugar-free chewing gum which is underlying the present analysis is less than four gums per week. The actual respective number for Germany is slightly above two gums per week. It seems realistic to reach this level of consumption if the consumption of sugar-free gum is promoted by health authorities as it happens in Finland [Citation33].
In the recently published study of Claxton et al., cost savings in dental care were calculated for a 12-year-old population in UK [Citation34]. When consuming two to three sugar-free chewing gums per day, a cost reduction between £1.2 and £8.2 million could be achieved. The risk reduction was calculated on the basis of one only study which showed a caries reduction of 25% to 33% when at least five gums were chewed per day [Citation11]. The risk reduction in the present analysis is considerably lower, because the chewing gum consumption was less than four pieces per week. Type (stripes, pellets), size, taste and formulation of sugar-free gum were not considered in the present study. There is no evidence for differences in the effectiveness of the usually used sugar substitutes Xylitol and Sorbitol [Citation27,Citation35] and because there is no data about the influence of other chewing gum characteristics.
Finland was chosen as a reference not only because of its higher consumption of sugar-free chewing gum but also because it is comparable to Germany with respect to oral health care provision. Health services in Finland are mainly arranged by public sector and financed by taxes, whereas in Germany a mandatory membership in a health insurance company exists [Citation36]. However, in both countries, a comparable oral health supply is provided for everyone. Both countries show a DMFT of 0.7 in 12-year olds in the first decade of the twenty-first century [Citation2,Citation32]. However, no actual data for other age groups are available for Finland and therefore, predictions from our study cannot be validated against Finnish data.
It was argued that high-risk groups with low socioeconomic status could particularly benefit from the consumption of sugar-free chewing gum because it is a low-threshold caries preventive measure. However, no data about the effectiveness of sugar-free chewing gum is available for this group. Therefore, it is not possible to give any information for this special subpopulation but only for the average German population.
The caries preventive effect of sugar-free chewing gum is based on the assumption that there is an even consumption of 0.30 pieces per capita and day in Germany which should be elevated to the Finnish level of 0.55 pieces. It is clear that this does not reflect the reality of chewing gum consumption. However, there is no data basis that allows us to identify proportions of high, medium, minimal and non-users nor do we have data that allow us to differentiate the benefits arising from chewing sugar-free gum in the different groups.
Studies analysing the cost-effectiveness of the consumption of sugar-free chewing gum with respect to oral health are rare. There is only the already mentioned study by Claxton et al. which analysed the economic benefit for 12-year olds when sugar-free gum was consumed two to three times per day. In the present study, the benefit was calculated over a complete lifespan (12 to 74 years) and a consumption of less than four chewing gums per week (ca. 0.5 per day) was assumed. Furthermore, Claxton et al. calculated the risk reduction on the basis of one study [Citation11] whereas it was based on a meta-analysis of several studies in the present paper [Citation9–20]. For Germany, no study has evaluated the benefit of sugar-free chewing gum, but only the lifelong use of various fluoride-applications on dental health [Citation37]. These authors found a cost-reduction of 77% based on the costs for prevention and therapy.
Within a budget-impact analysis, annual cost savings due to an increased consumption of sugar-free gum were calculated. In Germany, with an actual population of 81.2 million people [Citation25], annual cost savings of 313 million € can be achieved if the consumption of SFG increases to the level of Finland. The cost savings for the statutory health insurance account for 240 million €; private health insurance can achieve savings of 72 million € [Citation38].
In the present study, a lifelong observational period (62 years) was chosen to evaluate long-term outcomes. Since most patients visit the dentist once a year, a cycle was defined to be one year. Limitations of this analysis are given due to the missing heterogeneity of the model patient. The fourth German Oral Health Survey (DMS IV) [Citation2] shows differences in caries experience depending on age and socio-economic background. These differences could not be considered in the present analysis. Since the calculation of the transitions from one state to another is based on average DMFT values of the German population, the difference might be marginal. However, we cannot state which population groups would benefit most from the increased consumption of sugar-free gum.
There are currently only results from clinical studies assessing the influence of sugar-free chewing gum on primary caries. Since the causes leading to secondary caries are comparable to those causing primary decay, effects on the development of secondary caries were estimated on the basis of the risk reduction in primary caries. This assumption might lead to an underestimation of the effects of sugar-free chewing gum since the lifetime prevalence of secondary caries is higher than the lifetime prevalence of primary caries. Thus, greater potential for improvement seems possible.
In the analysis, only those costs were included which could probably be influenced by increased consumption of sugar-free chewing gum. We assumed that diagnostic and some other costs (such as impact on temporo-mandibular disorders) would not be influenced. It still would be necessary to visit the dentist at least once a year, to take X-rays, to remove calculus etc. However, the real impact of sugar-free gum on the expenditures for caries is still underestimated by this analysis. For every treatment, only the costs for the basic service are considered. Further possible treatments are not taken into account. In addition, the actual ratio of the consumption of sugar-free chewing gum for Finland and Germany is slightly higher than 1.82 since sugar containing gums are included in the consumption data (202 vs. 111 pieces per capita and year). According to this, cost savings due to sugar-free chewing gum are above our calculated results. Therefore, the present analysis is a conservative approach in terms of sugar-free chewing gum. For Germany, the elevation of the consumption of sugar-free chewing gum to the level of Finland would lead to a considerable benefit for oral health and cost saving for the statutory health insurance companies. Therefore, an increased consumption of sugar-free chewing gum should be promoted.
Disclosure statement
The funding company did not sponsor the preparation of the manuscript and did not influence its content. None of the authors is employed by the company, acts as a consultant, has patents which are related to the company or has any other financial conflict of interest.
Additional information
Funding
References
- Micheelis W, Bauch J. The Second German Oral Health Study. (Mundgesundheitszustand und -verhalten in der Bundesrepublik Deutschland. DMS II). Köln (Germany): Deutscher Ärzte-Verlag; 1991.
- Micheelis W, Schiffner U. The Fourth German Oral Health Study. (Vierte Deutsche Mundgesundheitsstudie. DMS IV). Köln (Germany): Deutscher Zahnärzte Verlag; 2006.
- Petersson GH, Bratthall D. The caries decline: a review of reviews. Eur J Oral Sci. 1996;104:436–443.
- Statistisches Bundesamt. 2018. German Federal Health Report. (Gesundheitsberichterstattung des Bundes.). Berlin, Germany. Available from: http://www.gbe-bund.de/gbe10/ergebnisse.prc_tab?fid = 26101&suchstring=&query_id=&sprache=D&fund_typ=TXT&methode=&vt=&verwandte = 1&page_ret = 0&seite = 1&p_lfd_nr = 1&p_news=&p_sprachkz=D&p_uid=gast&p_aid = 8629309&hlp_nr = 2&p_janein=J
- Iheozor-Ejiofor Z, Worthington HV, Walsh T, et al. Water fluoridation for the prevention of dental caries. Cochrane Database Syst Rev. 2015;6:CD010856.
- Rippe KP. [Ethical aspects of the fluoridation of water, salt, and milk]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2009;52:543–548.
- Marthaler TM. Salt fluoridation and oral health. Acta Med Acad. 2013;42:140–155.
- Banoczy J, Rugg-Gunn A, Woodward M. Milk fluoridation for the prevention of dental caries. Acta Med Acad. 2013;42:156–167.
- Moller IJ, Poulson S. The effect of sorbitol-containing chewing gum on the incidence of dental caries; plaque and gingivits in Danish schoolchildren. Commun Dent Oral Epidemiol. 1973;1:58–67.
- Isokangas P, Alanen P, Tiekso J, et al. Xylitol chewing gum in caries prevention: a field study in children. J Am Dent Assoc. 1988;117:315–320.
- Machiulskiene V, Nyvad B, Baelum V. Caries preventive effect of sugar-substituted chewing gum. Community Dent Oral Epidemiol. 2001;29:278–288.
- Scheinin A, Makinen KK, Tammisalo E, et al. Turku sugar studies XVIII. Incidence of dental caries in relation to 1-year consumption of xylitol chewing gum. Acta Odontol Scand. 1975;33:269–278.
- Glass RL. A two-year clinical trial of sorbitol chewing gum. Caries Res. 1983;17:365–368.
- Kandelman D, Gagnon G. A 24-month clinical study of the incidence and progression of dental caries in relation to consumption of chewing gum containing xylitol in school preventive programs. J Dent Res. 1990;69:1771–1775.
- Makinen KK, Bennett CA, Hujoel PP, et al. Xylitol chewing gums and caries rates: a 40-month cohort study. J Dent Res. 1995;74:1904–1913.
- Makinen KK, Makinen PL, Pape HR Jr, et al. Stabilisation of rampant caries: polyol gums and arrest of dentine caries in two long-term cohort studies in young subjects. Int Dent J. 1995;45:93–107.
- Beiswanger BB, Boneta AE, Mau MS, et al. The effect of chewing sugar-free gum after meals on clinical caries incidence. J Am Dent Assoc. 1998;129:1623–1626.
- Petersen PE, Razanamihaja N. Carbamide-containing polyol chewing gum and prevention of dental caries in schoolchildren in Madagascar. Int Dent J. 1999;49:226–230.
- Szoke J, Banoczy J, Proskin HM. Effect of after-meal sucrose-free gum-chewing on clinical caries. J Dent Res. 2001;80:1725–1729.
- Peng B, Petersen PE, Bian Z, et al. Can school-based oral health education and a sugar-free chewing gum program improve oral health? Results from a two-year study in PR China. Acta Odontol Scand. 2004;62:328–332.
- Meyer-Lückel H, Paris S, Ekstrand K. Karies. Stuttgart (Germany): Thieme; 2012.
- Hellwig E, Klimek J, Attin T. Introduction to Operative Dentistry. (Einführung in die Zahnerhaltung.) Köln (Germany): Deutscher Zahnärzte Verlag; 2013.
- Bückmann B. Healthy Teeth: Prevention, Treatment, and Costs. (Gesunde Zähne: Vorsorge, Behandlung und Kosten.) Berlin (Germany): Stiftung Warentest; 2010.
- Kassenzahnärztliche Bundesvereinigung. Tables of Charges. (Gebührenverzeichnisse.) Köln (Germany): Kassenzahnärztliche Bundesvereinigung; 2014.
- Kassenzahnärztliche Bundesvereinigung. Yearbook 2015. (Jahrbuch 2015.) Köln (Germany): Kassenzahnärztliche Bundesvereinigung; 2015.
- Van Loveren C. Sugar alcohols: what is the evidence for caries-preventive and caries-therapeutic effects? Caries Res. 2004;38:286–293.
- Mickenautsch S, Yengopal V. Effect of xylitol versus sorbitol: a quantitative systematic review of clinical trials. Int Dent J. 2012;62:175–188.
- Honkala S, Runnel R, Saag M, et al. Effect of erythritol and xylitol on dental caries prevention in children. Caries Res. 2014;48:482–490.
- Thabuis C, Cheng CY, Wang X, et al. Effects of maltitol and xylitol chewing-gums on parameters involved in dental caries development. Eur J Paediatr Dent. 2013;14:303–308.
- Finnish Dental Association. Recommendations of the Finnish Dental Association. Helsinki (Finland): Finnish Dental Association; 2016.
- Civil Aviation Authority Singapore. National Regulations and Requirements Gen 1.3 Entry, Transit and Departure of Passengers and Crew. Singapore: Singapore Aviation Authority Singapore; 2016.
- Widström E, Järvinen S. Caries prevalence and use of dental services in Finnish children and Adolescents in 2009. Oral Health Dent Man. 2011;10:185–192.
- Honkala S, Honkala E, Tynjala J, et al. Use of xylitol chewing gum among Finnish schoolchildren. Acta Odontol Scand. 1999;57:306–309.
- Claxton L, Taylor M, Kay E. Oral health promotion: the economic benefits to the NHS of increased use of sugarfree gum in the UK. Br Dent J. 2016;220:121–127.
- Riley P, Moore D, Ahmed F, et al. Xylitol-containing products for preventing dental caries in children and adults. Cochrane Database Syst Rev. 2015;(3):CD010743.
- Tiemann B, Klingenberger DMW. Dental Services in Germany. (System der zahnärztlichen Versorgung in Deutschland.) Köln (Germany): Institut der Deutschen Zahnärzte; 2003.
- Splieth CH, Flessa S. Modelling lifelong costs of caries with and without fluoride use. Eur J Oral Sci. 2008;116:164–169.
- Kreimendahl F, Spyra A, Zimmer S, et al. [Sugar free gum: cost savings possible]. Gesellschaftspolitische Kommentare. 2015;56:9–10.