Abstract
Objective: To develop and assess a set of criteria to grade inflammation including relative area of inflammation in periapical lesions in endodontically treated teeth.
Material and methods: A set of criteria was developed, encompassing data on: Lymphocytes, denoting chronic inflammation, were graded 0 (occasional) to 4 (heavy/dense inflammation). Polymorphonuclear cells, denoting acute inflammation, were graded 0 (none) to 2 (many). The third parameter, area of inflammation, that is, the relative area of the specimen that was inflamed, was graded 0 (none) to 4 (76–100%). The criteria were tested on 199 consecutive biopsies from 180 patients (aged 31–75 years). Information about symptoms was retrieved from the referrals. Mann–Whitney’s U-test was used to calculate possible differences in average values for the histopathological variables in the two groups of patients: symptomatic or asymptomatic.
Results: Using the criteria, varying grades of inflammation were seen in the biopsies. The majority showed few or no PMN cells. There was a correlation between symptoms and the extent of infiltration of lymphocytes and plasma cells (p = .001), PMN cells (p < .001) and the area of inflammation (p = .002): biopsies from the asymptomatic patients exhibited less pronounced and relatively smaller areas of inflammation.
Conclusions: Using the criteria on a specific selection of root-filled teeth with persisting apical periodontitis, periapical inflammation was common, but varied in extent and severity. The inflammation was less pronounced and affected a relatively smaller area in asymptomatic teeth, although outliers in both directions were identified.
Introduction
Apical periodontitis results from spread of infection from the root canal system, with progressive inflammation and changes to the periapical bone [Citation1–3]. The result is bone resorption, which appears as a radiolucent area on periapical radiographs. Root canal treatment is undertaken in order to eliminate infected tissues from the root canal. Periapical healing usually occurs with osseous regeneration, characterized by a reduction in size of the radiolucency, observed on follow-up radiographs [Citation4–8].
In periapical radiographic evaluation of the outcome of endodontic treatment, the persistence or development of periapical radiolucency, even in asymptomatic teeth, is often denoted as a therapeutic failure. According to the guidelines of the European Society of Endodontology [Citation9] and the classical follow-up evaluation system by Strindberg [Citation4], apical periodontitis should have healed within four years of endodontic treatment; any other outcome could be viewed as persistence of the original disease. Nevertheless, population based cross-sectional studies show a high frequency of apical periodontitis associated with root-filled teeth, ranging from 14 to 72% [Citation10].
Several histopathological studies have shown that apical periodontitis is the most prevalent type of periapical lesions of endodontic origin [Citation8,Citation11,Citation12], manifesting as granulation tissue surrounded by fibrous connective tissue. The histological patterns vary with respect to the number of different cell types and their products, including lymphocytes, neutrophils, plasma cells, endothelial cells and fibroblasts. Typically, lymphocytes and neutrophils are in varying extent present in the lesion, representing chronic and acute inflammation [Citation8,Citation13]. However, a few reports showed that the healing after conventional root canal treatment may also result in formation of fibrous tissue composed dense collagen fibres, few cells and little or no inflammation, which may be regarded as scar tissue [Citation8]. This fibrous tissue will present as a radiolucency in follow-up radiographs and mimic an ongoing inflammation/infection, i.e. apical periodontitis or a radicular cyst [Citation12]. Earlier studies have shown an association between inflammation and periapical radiolucency on radiographs, but little is actually known about the extent and degree of inflammation observed in biopsies from periapical tissue [Citation14].
The high prevalence of periapical lesions in endodontically treated teeth observed in cross-sectional studies indicates that guidelines are not strictly followed [Citation14–17]. Arguments in favor of treatment are that persisting chronic inflammation may exacerbate and cause pain and, in the worst case, may develop into a local abscess with potential for life-threatening spread to adjacent parts of the body [Citation18]. However, such treatment causes patient discomfort, considerable chairside time and added costs and the procedure itself could damage both the tooth and covering restorations and jeopardize the prognosis. The health-economic implications for society should also be taken into account. As persistent periapical lesions in endodontically treated teeth are not uncommon, there is a need for more detailed investigation of these lesions, to determine the characteristics and severity of the inflammation. A deeper understanding of the histopathology should aid formulation of a set of criteria to support clinical decisions about management of the condition.
The aim of the study was to develop and assess a set of histological criteria for grading inflammation in periapical lesions in endodontically treated teeth, including the relative area of inflammation.
Materials and methods
Set of criteria
In order to grade inflammation, a schedule consisting of three parameters was created: Lymphocytes, denoting chronic inflammation, were graded 0 (occasional) to 4 (heavy/dense inflammation). Polymorphonuclear cells, denoting acute inflammation, were graded 0 (none) to 2 (many). The third parameter, area of inflammation, that is, the relative area of the specimen that was inflamed, was graded 0 (none) to 4 (76–100%). This could also be described as the proportion of the specimen; if only scattered inflammatory cells (of either sort) were detected, then the area of inflammation was graded 0 (none). In other words, even though a small number of lymphocytes were noted, their relative area of the biopsy could be very small, less than 1%. On the other hand, if all or nearly all (76–100%) of the specimen was infiltrated by inflammatory cells then the area of inflammation was graded 4 ().
Table 1. Schedule of the assessment criteria used for the histopathological investigation.
In order to test the developed criteria, biopsies of periapical lesions in endodontically treated teeth were examined histologically applying the criteria and thus determining the degree and extent of inflammation. These findings were correlated with available clinical information regarding symptoms. Thus two sets of variables were collected: histological and clinical.
Test of criteria
The material was specifically chosen, comprising 233 biopsies from 205 patients sent between 1988 and 1993 to the Department of Oral Pathology, Malmö University, Sweden, by one oral surgeon. The biopsies were differentially diagnosed as apical periodontitis or scar tissue, codes 522,6X and 998, respectively, according to the International Classification of Diseases, Ninth Revision (ICD-9). Biopsies differentially diagnosed as periapical cysts were not included. The most central part of the biopsies were at the time routinely processed, that is cut into 3 µm sections and stained with haematoxylin and eosin and analyzed. They have since been stored in biobank 497 at the Department of Oral Pathology, Malmö University. For this study, only one section per tooth was analyzed, if more than one section was available, a joint decision was made which one to analyze.
Inclusion of
Biopsies of periapical lesions from root-filled teeth, diagnosed as apical periodontitis or scar tissue.
Exclusion of
Biopsies diagnosed as apical periodontitis from teeth which had not been root-filled.
Biopsies re-diagnosed as radicular cysts.
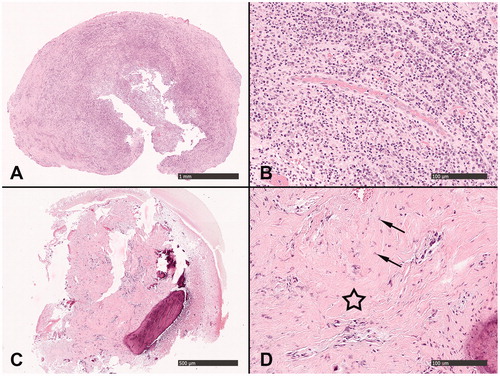
The samples were analysed independently by two calibrated, blinded observers, using a Nikon eclipse 80i light microscope (LRI microscope, Lund, Sweden). The observers did not have access to any clinical information from the referrals. Inter- and intra-rater reliabilities were calculated. In case of disagreement, the observers discussed the cases until they reached consensus. In biopsies with more than one histological appearance, the most severe state of inflammation was registered ().
Figure 1. Biopsies showing example of application of the schedule of assessment criteria in the histopathological investigation (). (A) Infiltration of lymphocytes and plasma cells, with a higher magnification in (B), was denoted as heavy/dense general inflammation (4) and heavy infiltration of PMN cells (2). (C) Fibrous tissue with no area of inflammation (0) with a higher magnification in (D), which presents tightly packed collagen and scattered fibroblasts: only occasional possible lymphocytes (0) and no PMN cells (0). Star denotes fibrous tissue and arrows denote fibroblasts.
Clinical variables
The following variables from the coded referrals were registered, as reported by the oral surgeon:
symptoms from the tooth, described as discomfort, pain, swelling or a fistula or intake of antibiotics
age and sex of the patient
upper or lower jaw
interval between root canal treatment and periapical surgery
progressive increase in lesion size since the root canal filling.
Statistical method
Mann–Whitney’s U-test was used to analyze possible differences in average values for the following histopathological variables: infiltration of lymphocytes, infiltration of PMN-cells and area of inflammation in the biopsy, in relation to symptoms, the clinical variable.
The results were analyzed using IBM Statistical Packages of Social Sciences version 22 (SPSS Inc., Chicago, IL, USA). The level of significance was set at 5% (p ≤ .05).
Ethical issues
The ethical application was approved (Dnr 2014/226) by the Regional Ethical Board at Lund University, Sweden.
Results
The developed criteria were assessed on a sample consisting of 233 biopsies obtained from 205 patients. After applying inclusion and exclusion criteria, the final sample comprised 199 biopsies from 180 patients.
Characteristics of the 180 patients
A summary of the characteristics of the entire study material is presented in . The age range was 31–75 years, mean 53 years. The interval between root canal treatment and periapical surgery varied from 2 months to 50 years, mean 12 years. For 41 patients (20.6%) this information was missing.
Table 2. Characteristics of the complete material registered from the referrals: the patient was classed as symptomatic when the referral noted discomfort, pain, swelling, a fistula, or antibiotic administration.
Reliability of the histopathological examination
If more than one biopsy per tooth was available, a joint decision was made, based on the quality of the biopsies, as to which histological section was to be included. The biopsy showing the most severe inflammation was consistently selected.
One of the two observers undertook two separate analyses, one month apart, achieving an intra-rater agreement of 87%. Inter-rater agreement, between the two observers, was 90%. In 19 cases, the observers discussed the biopsies until they reached consensus.
Grading of inflammation in relation to symptoms
Lymphocytic infiltration varied according to whether or not the patients had reported symptoms at the time of the apical surgery (p = .001) (1, ). Seventy percent (73/105) of the biopsies from patients reporting symptoms exhibited severe infiltration of lymphocytes (Grade 3). Larger and denser accumulation of lymphocytes and plasma cells (Grade 4) was more frequent in the symptomatic group, while modest infiltration of cells (Grades 1 and 2) was more frequent in the asymptomatic group (). PMN infiltration also differed according to whether or not the patients had reported symptoms at the time of the apical surgery (p < .0001) (). The relative area of inflammation was larger in symptomatic than in asymptomatic patients (p = .002) ().
Table 3. Extent of infiltrations and area of inflammation in the biopsies in relation to any reported symptoms in the referrals.
Discussion
This study evaluated a set of criteria assessing the inflammation in biopsies of periapical lesions in endodontically treated teeth. Some recent studies have investigated a possible correlation between symptoms and histopathological diagnosis of the periapical radiolucency [Citation19,Citation20]. In contrast to most previously used criteria, the present criteria included assessments of the severity and extent of the inflammation, which could possibly be an indirect measure of the extent of scar tissue in the overall evaluation. The two observers who tested the grading system showed high inter-and intra-rater reliability.
Most periapical lesions in endodontically treated teeth should heal completely within 4 years of endodontic treatment [Citation4]. The sample to which the developed criteria were applied comprised all 199 consecutive biopsies from one surgeon who seems to have adhered to the Strindberg criteria, considering apical surgery on asymptomatic lesions persisting more than 4 years. As it has been shown that many periapical lesions in endodontically treated teeth are left untreated [Citation21], we considered it valuable to test the developed criteria on this specific sample of periapical lesions from endodontically treated teeth as it probably reflects a very strict selection and possibly cases of what we today would presumably consider overtreatment. In a prospective study it would not be advisable to collect samples from only one surgeon: data collected from multiple centres would increase the generalizability of the study results [Citation22].
The test of the criteria was applied to the most severe inflammation in the biopsy and the inflamed area as a percentage of the total biopsy area. As this study was set up primarily in order to develop criteria to be applied in a prospective study, the results regarding the assessment of biopsies should be interpreted cautiously: there are major limitations, such as lack of proper access to patient history and symptoms. As the most inflamed area could be expected to be found in the area of the apical foramina, the specimen should ideally be longitudinally serially sectioned [Citation23]. A future study could also include staining for microorganisms, as it would be of interest to study the location of these in relation to clinical signs and symptoms [Citation23].
When applying the set of criteria to this specific set of biopsies of apical periodontitis, the lesions exhibited varying degrees of inflammation. The morphology of lymphocytes and PMN-cells is easily distinguishable histologically and was applied in this study to represent chronic and acute inflammatory states, respectively [Citation13]. The developed grading-system disclosed that the level of lymphocyte and PMN-cell infiltration differed considerably. The appearances of the biopsies ranged from heavy/dense generalized inflammation with abundant PMN-cells, to the occasional possible lymphocyte with no PMN-cells. Even though the selected set of biopsies has its shortcomings, the clinical parameters were significantly related to the histological appearance: the biopsies from patients who had reported symptoms exhibited a denser accumulation of lymphocytes and PMN-cells than those from asymptomatic patients. Irrespective of the type of inflammation, the area of inflammation was relatively larger in the symptomatic group. However, there were also outliers in both directions: that is, biopsies from some patients reporting no symptoms showed heavy inflammation and those from some patients with symptoms showed little or no inflammation.
Periapical lesions in endodontically treated teeth are of interest to most clinicians and patients, as little is known about this condition. Successful root canal treatment has conventionally been determined on radiographic evidence, the healed apical tissues appearing as bone regeneration [Citation4]. However, in the clinical setting, radiographic signs of apical periodontitis in asymptomatic root-filled teeth might be accepted by dental practitioners [Citation24,Citation25]. This is highlighted by a survey in Denmark in which retreatment was rarely cited as a reason for root canal treatment [Citation26]. In accordance with this finding, a longitudinal epidemiological study disclosed that 42% of root-filled teeth with apical periodontitis at base-line examination remained untreated 20 years later [Citation21].
It is important to gain more knowledge about the periapical lesions in endodontically treated teeth and a central question is whether the asymptomatic periapical lesion in an endodontically treated tooth is a threat to health. Sometimes the condition exacerbates. However, little is known about the incidence and severity of such events. In a study from a university hospital in Singapore, a cohort of 127 patients with 185 teeth with persistent periapical lesions in endodontically treated teeth was studied retrospectively for 4–38 years [Citation27]. After twenty years, there had been at least one severe pain event in 6% of the lesions and less acute discomfort or pain in 45%. The results of studies investigating a possible association between apical periodontitis and cardiovascular disease are inconsistent [Citation28–30]. In a cross-sectional study from Finland it was concluded that apical periodontitis, especially on non-root-filled teeth, is associated with coronary artery disease [Citation31]. This difference of root-filled and non-root-filled teeth could be supported by the classical study by Brynolf [Citation32] in which less acute cell infiltration was seen in root-filled compared to non-root-filled teeth.
It is sometimes argued that Cone Beam CT (CBCT) should be used to assess the periapical tissues, as the technique allows the detection of smaller apical lesions. In the present study, the root-filled teeth with apical periodontitis were assessed by conventional periapical radiographs. Biopsies from many of the asymptomatic patients showed a very small relative area of inflammation, or none at all; thus it may be argued that they were over-treated. Using CBCT would increase the risk of overtreatment. In a Danish study, 42% of teeth which underwent apical surgery, diagnosed with asymptomatic apical periodontitis, had no periapical inflammation [Citation33]. The corresponding number in the present study was 51%. The results highlight not only the scientific uncertainty about the true nature of persistent apical radiolucency associated with asymptomatic root-filled teeth, but also the need to develop systems for differential diagnosis of cases which warrant urgent treatment and those in which further intervention is more questionable. It has been shown that the clinical decision making varies between clinicians [Citation34], possible due to the scientific uncertainty regarding the persistent apical periodontitis and it would be valuable to the society if the clinical decision process should be based on more solid scientific knowledge, in order to avoid over- and under treatment.
Conclusions
Using the developed set of criteria on a specific selection of root-filled teeth with persisting apical periodontitis, periapical inflammation was common, but varied in extent and severity. The inflammation was less pronounced and affected a relatively smaller area in asymptomatic teeth, although outliers in both directions were identified.
Acknowledgements
Authors N. D. and A. C. L. have contributed equally to this project.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Kakehashi S, Stanley HR, Fitzgerald RJ. The effects of surgical exposures of dental pulps in germfree and conventional laboratory rats. J South Calif Dent Assoc. 1966;34:449–451.
- Moller AJ. Microbiological examination of root canals and periapical tissues of human teeth. Methodological studies. Odontol Tidskr. 1966;74:1–380.
- Nair PN. Light and electron microscopic studies of root canal flora and periapical lesions. J Endod. 1987;13:29–39.
- Strindberg LZ. The dependence of the results of pulp therapy on certain factors. An analytic study based on radiographic and clinical follow-up examinations. Acta Odont Scand. 1956;14:1–175.
- Kerekes K, Tronstad L. Long-term results of endodontic treatment performed with a standardized technique. J Endod. 1979;5:83–90.
- Sjogren U, Hagglund B, Sundqvist G, et al. Factors affecting the long-term results of endodontic treatment. J Endod. 1990;16:498–504.
- Sundqvist G, Figdor D, Persson S, et al. Microbiologic analysis of teeth with failed endodontic treatment and the outcome of conservative re-treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85:86–93.
- Nair PN, Sjogren U, Figdor D, et al. Persistent periapical radiolucencies of root-filled human teeth, failed endodontic treatments, and periapical scars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;87:617–627.
- European Society of Endodontology. Quality guidelines for endodontic treatment: consensus report of the European Society of Endodontology. Int Endod J. 2006;39:921–930.
- Pak JG, Fayazi S, White SN. Prevalence of periapical radiolucency and root canal treatment: a systematic review of cross-sectional studies. J Endod. 2012;38:1170–1176.
- Garcia CC, Sempere FV, Diago MP, et al. The post-endodontic periapical lesion: histologic and etiopathogenic aspects. Med Oral Patol Oral Cir Bucal. 2007;12:E585–E590.
- Love RM, Firth N. Histopathological profile of surgically removed persistent periapical radiolucent lesions of endodontic origin. Int Endod J. 2009;42:198–202.
- Abbas A, Lichtman AH. Basic immunology, functions and disorders of the immune system. 5th ed. St Louis (MO): Elsevier; 2015.
- Bergenholtz G. Assessment of treatment failure in endodontic therapy. J Oral Rehabil. 2016;43:753–7538.
- Kirkevang LL, Orstavik D, Horsted-Bindslev P, et al. Periapical status and quality of root fillings and coronal restorations in a Danish population. Int Endod J. 2000;33:509–515.
- Skudutyte-Rysstad R, Eriksen HM. Endodontic status amongst 35-year-old Oslo citizens and changes over a 30-year period. Int Endod J. 2006;39:637–642.
- Frisk F, Hugoson A, Hakeberg M. Technical quality of root fillings and periapical status in root filled teeth in Jönköping, Sweden. Int Endod J. 2008;41:958–968.
- Green AW, Flower EA, New NE. Mortality associated with odontogenic infection!. Br Dent J. 2001;190:529–530.
- Barthel CR, Zimmer S, Trope M. Relationship of radiologic and histologic signs of inflammation in human root-filled teeth. J Endod. 2004;30:75–79.
- Ricucci D, Siqueira JF, Bate AL, et al. Histologic investigation of root canal-treated teeth with apical periodontitis: a retrospective study from twenty-four patients. J Endod. 2009;35:493–502.
- Petersson K, Fransson H, Wolf E, et al. Twenty-year follow-up of root filled teeth in a Swedish population receiving high-cost dental care. Int Endod J. 2016;49:636–645.
- Bellomo R, Warrillow SJ, Reade MC. Why we should be wary of single-center trials. Crit Care Med. 2009;37:3114–3119.
- Ricucci D, Pascon EA, Ford TR, et al. Epithelium and bacteria in periapical lesions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:239–249.
- Kvist T, Reit C, Esposito M, et al. Prescribing endodontic retreatment: towards a theory of dentist behaviour. Int Endod J. 1994;27:285–290.
- Kvist T, Heden G, Reit C. Endodontic retreatment strategies used by general dental practitioners. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;97:502–507.
- Bjørndal L, Laustsen MH, Reit C. Root canal treatment in Denmark is most often carried out in carious vital molar teeth and retreatments are rare. Int Endod J. 2006;39:785–790.
- Yu VS, Messer HH, Yee R, et al. Incidence and impact of painful exacerbations in a cohort with post-treatment persistent endodontic lesions. J Endod. 2012;38:41–46.
- Jansson L, Lavstedt S, Frithiof L, et al. Relationship between oral health and mortality in cardiovascular diseases. J Clin Periodontol. 2001;28:762–768.
- Frisk F, Hakeberg M, Ahlqwist M, et al. Endodontic variables and coronary heart disease. Acta Odontol Scand. 2003;61:257–262.
- Caplan DJ, Chasen JB, Krall EA, et al. Lesions of endodontic origin and risk of coronary heart disease. J Dent Res. 2006;85:996–1000.
- Liljestrand JM, Mäntylä P, Paju S, et al. Association of endodontic lesions with coronary artery disease. J Dent Res. 2016;95:1358–1365.
- Brynolf I. A histological and roentgenological study of the periapical region of human upper incisors. Odontol Revy. 1967;18:11.
- Kruse C, Spin-Neto R, Reibel J, et al. Diagnostic validity of periapical radiography and CBCT for assessing periapical lesions that persist after endodontic surgery. Dentomaxillofac Radiol. 2017;46:20170210.
- Kvist T. Endodontic retreatment. Aspects of decision making and clinical outcome. Swed Dent J Suppl 2001;(144):1–57.
