Abstract
Objective: Many patients with temporomandibular disorders (TMD) seem to go undetected within primary dental health care. Primarily we evaluated if the implemented intervention increased the clinical decision-making for TMD patients; secondarily we evaluated if other factors could be identified that predicted performed or recommended TMD treatment.
Material and Methods: This case–control study was carried out within the Public Dental Health service in Västerbotten County, Sweden. An intervention based on a decision-tree with three screening questions for TMD (3Q/TMD) was implemented during 2015 in four clinics and compared with the remaining county. A total of 400 individuals were selected—200 3Q-positives and 200 3Q-negatives. The 3Q/TMD consists of Q1—frequent jaw pain, Q2—frequent pain on function, and Q3—frequent catching and/or locking of jaw. The 3Q/TMD answers were analyzed in relation to TMD treatment and any TMD related decision that was collected from the digital dental records.
Results: The intervention did not increase the frequencies of traceable clinical decisions among patients with TMD.
Conclusions: Despite the implemented intervention aimed, the indicated undertreatment of patients with TMD remains. Future studies are still needed to gain a deeper understanding of the clinical decision-making process for TMD patients in general practice dentistry.
Introduction
Temporomandibular disorders (TMD) are the umbrella term to include pain and dysfunction involving the masticatory muscles and/or the temporomandibular joint (TMJ) [Citation1,Citation2]. TMD is considered as the most common chronic pain condition in the orofacial region, and after pain in the lower back and knee it is the most prevalent chronic pain condition [Citation3]. Characteristic symptoms related to TMD are not only pain but also functional disturbances such as clicking and locking of the TMJ as well as impaired jaw movements. TMD affects the quality of life negatively and patients with TMD often have comorbid conditions including depression and stress [Citation4]. With the perspective that any pain can evolve into a chronic and more complex condition with more demanding treatment strategies and worsening long-term prognosis, the importance of early identification of TMD is advocated [Citation5].
Evidence-based medicine (EBM) was introduced and defined as the incorporation of best available scientific evidence, clinical judgment, and patient’s values in the care of every individual patient [Citation6]. Even though the possibilities for providing EBM for patients with TMD already seem to exist and the majority of individuals with TMD could be effectively managed in dentistry [Citation7], many patients with TMD seem to go undetected and under-treated within dentistry [Citation8–10]. The reasons for the discrepancy between estimated treatment need and performed treatment is not known, and there may be several reasons that contribute to this observed discrepancy. Among those are the patient’s financial capacity, the clinical decision-making process in primary care where both diagnosis and management of TMD may be challenging tasks [Citation11], or organizational inequities within the dental care system [Citation12,Citation13]. These are, however, all factors contributing to the nonclinical influences on decision-making [Citation13]. Decision-making is described as the complex phenomenon that is guided by ones previous experiences and frequencies rather than probability theories [Citation14]. The nonclinical influences are described as related to both patient and clinician characteristics and include sociodemographic factors such as age, gender, and ethnicity [Citation15]. Moreover, uncertainties among clinicians also increase the risk of biased decisions. Previous findings have identified uncertainties in the management of patients with TMD [Citation16], and these patients are therefore at risk of being affected by the clinicians’ biased decisions [Citation9]. Decision-trees have been suggested to be important to prevent unjustified inequities in health care [Citation17] as well as in dentistry [Citation12]. The 3Q/TMD is an example of a valid screening tool for the identification of patients who could benefit from a further TMD examination [Citation18]. The 3Q/TMD consists of three screening questions for the identification of frequent TMD symptoms. Even though the 3Q/TMD has the ability to predict a TMD diagnosis, we have previously found that the majority of individuals with a screen positive to 3Q/TMD, still did not receive TMD treatment [Citation10]. Taken together, the screening tool does not appear to be used as intended, and it was concluded that additional efforts were needed to improve the dental care for patients with TMD in dentistry. One example of improvement of care could be an intervention based both on education and implementation of a strict management guideline.
The overall objective of this study was to evaluate the efficacy of an intervention aimed at optimizing the use of the 3Q/TMD. Therefore, the first specific aim was to evaluate if an implemented intervention in 2015, based on the 3Q/TMD, affected the clinical decision-making for 3Q-positive patients at clinics included in the intervention programme in comparison to clinics that were not included. The hypothesis was that the implementation of the decision tree would increase the clinical decisions related to TMD symptoms for 3Q-positive patients. Our second aim was to evaluate if specific nonclinical factors predicted performed or recommended TMD treatment. Our last and third aim was to assess treatment frequencies between 3Q-positive patients and 3Q-negative patients at clinics included in the intervention programme.
Materials and methods
Study setting
This prospective case–control study was carried out within the county of Västerbotten, Sweden, during 2015. Four Public dental health service (PDHS) clinics that formed a larger unit, Umeå Nord, were included in the intervention program. The four clinics were all lead by a mutual head-of-chief and had the daily practice led by separate floor managers at each clinic.
3 Q/TMD (Exposure)
In Västerbotten Sweden, the three screening questions (3Q/TMD) are a part of a mandatory digital health declaration on general health status in the patient’s dental record [Citation19]. At every regular dental check-up, the dentist or dental hygienist is expected to fill out a digital health declaration for each patient. The health declaration cannot be finalized without the three questions answered. The three screening questions of the 3Q/TMD are formulated as follows:
Q1: ‘Do you have pain in your temple, face, jaw or jaw joint once a week or more?’
Q2: ‘Do you have pain once a week or more when you open your mouth or chew?’
Q3: ‘Does your jaw lock or become stuck once a week or more?’
Patients who answered ‘yes’ to any of the 3Q/TMD questions were categorized as 3Q-positives, whereas patients who answered ‘no’ to all of the 3Q/TMD questions were categorized as 3Q-negatives. In the present study, 3Q-positives were regarded as cases and 3Q-negatives as controls.
Study population
The intervention clinics comprised of patients from Umeå Nord and the reference clinics from the remaining clinics in Västerbotten county that were not included in the intervention programme. Umeå Nord consisted of 10,354 patients (female/male ratio 1:1; mean age 27.3 ± SD = 22.6 years) and the reference clinics of 53,440 individuals (female/male ratio 1:1; mean age 42.3 ± SD = 15.3 years) [Citation9].
Following inclusion criteria were used at the intervention clinics:
A dental check-up within the time period of January to December 2015
A completed digital health declaration during the dental check-up
20–70 years of age
There were no exclusion criteria.
The same inclusion criteria were used at the reference clinics [Citation9].
Intervention and outcome
The intervention was approved by both the head-of-chief and all four floor managers at each clinic. The adherence to the predetermined steps of the intervention was agreed to be an overall priority during the fiscal year of 2015. Prior to the implementation of the decision-tree, all staff members in the four clinics were educated about; TMD in general and how to proceed into management of these patients.
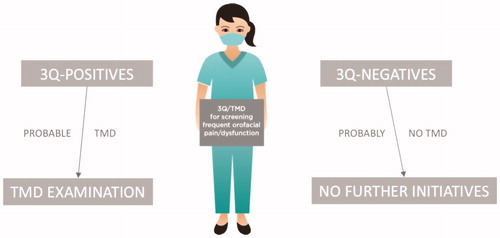
The implemented intervention with the decision-tree was comprised of strict information about how to offer all individuals, with at least one affirmative answer to the 3Q/TMD, an extended evaluation and examination performed by a dentist (). All clinicians were instructed to document the outcome of the following decision process in each patient’s record, as well they were informed about a planned follow-up of the adherence to the decision-tree. The primary outcome was the frequency of traceable clinical decisions related to TMD symptoms at the intervention clinics.
Sample size calculation
The power was calculated using 100,000 Monte Carlo simulations. This was accomplished by simulating the outcomes for the two groups from two different Bernoulli distributions. A logistic regression model was then fitted to the simulated data and power was estimated as the proportion of times the group effect was significant at a .05 significance level. The probabilities for TMD decisions are assumed to be 54% for the reference clinics during 2015 [Citation9] and expected to be slightly increased to 70% in the intervention clinics. These percentages were used in the simulation of the probabilities of traceable TMD decisions as binary outcomes. The simulation experiment showed that a sample size of total 240 individuals was needed to achieve a power of 80%. Since TMD decisions were expected to be rare among the 3Q-negatives, the total sample size was determined to n = 400. Therefore, a total of 400 individuals were randomly selected—one sample of 200 3Q-positives creating the case group, and a corresponding sample of 200 3Q-negatives creating the control group (SPSS, random sample).
Variables
From the intervention clinics, data were scrutinized and extracted from digital dental records by two independent examiners (A.N. and J.F.). The extracted data was retrieved by the examiners blinded to whether the current patient was a case (3Q-positive) or a control (3Q-negative). When the two examiners did not agree on their evaluation of a variable, a third blinded examiner assessed the data (A.L.). Consensus was reached based on all three examiners opinion, and the final consensus agreement for each variable was then used in the statistical analyses. All entries reported in the dental record for each patient, starting from the date of routine dental check-up with a completed health declaration and 1 year ahead, were retrieved and analyzed. The following data were extracted from the dental records, registered in an Excel spread sheet and encoded for the individual patient: patients’ gender and age, profession of the examiner (dentist or dental hygienist), gender of examiner, TMD treatment, including type of treatment, if the patient declined prescribed or recommended treatment, when no treatment was deemed necessary. Since patients in Sweden can choose either to pay a fee for service or enter a 3-year agreement in an insurance-system (subscription dental care) where you pay a predefined charge, these variables were also extracted.
All variables were extracted to enable comparison of treatment frequencies at the intervention clinics among 3Q-positive and 3Q-negative patients. The results from Lövgren et al. were used for comparison between intervention clinics and reference clinics (Lövgren et al., 2018).
Statistical analyses
Descriptive statistics were used to characterize the study sample (frequencies, χ2 and Mann-Whitney U). The inter-rater reliability was calculated according to Cohen’s κ. In relation to our first aim, comparisons between intervention clinics and reference clinics were conducted by χ2. Univariate predictive regression models were used to evaluate the possible association between 3Q-positives and TMD treatment (odds ratio, OR). TMD treatment was used as a dependent variable in the analysis. It was categorized as positive (1) when TMD treatment was performed (individual information and behavioral treatments, jaw exercises, occlusal appliances, adjustment of occlusal appliances, referral to TMD specialist, referral to other health service, TMD treatment not charged for), was performed, and the remaining was categorized as zero (0). Any TMD related decision was used as another dependent variable and categorized positive (1) whenever a TMD decision was made (including TMD treatment, if the patient declined to recommended and offered treatment, and if the examiner deemed no treatment needed) and the remaining was categorized as zero (0). Independent variables that were associated to TMD treatment at a probability level of <.1 were included in the multiple predictive regression model. Observed differences were considered as statistically significant when the odds ratio and its confidence interval did not include 1 (one) or for probability levels below .05. The data were analyzed with SPSS (IBM SPSS Statistics for Macintosh, version 24; IBM Corp Armonk, NY). The study was ethically reviewed and approved by the Central Ethical Review Board, Umeå University, Sweden (Ref no: 2015-80-32-M).
Results
The 3Q-positives were significantly more often women (72%) compared to the 3Q-negatives (47%) (χ2 value 26.025, p < .001). There was no significant difference in age between 3Q-positives compared to 3Q-negatives (Mann-Whitney U 18,370.00, p = .2). In the total sample, 23% were registered for a subscription dental plan. Two records (one 3Q-positive and one 3Q-negative) out of the 400 were excluded due to missing data.
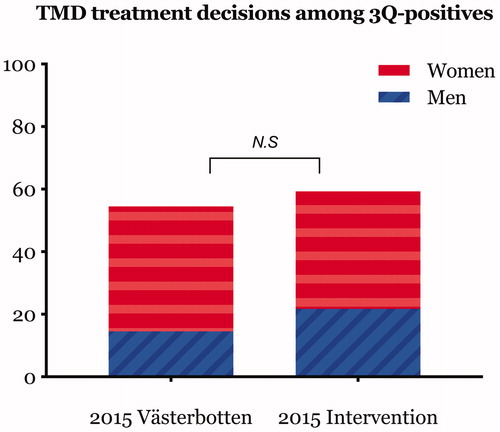
In total, a traceable clinical decision in relation to TMD was observed among 59% of the 3Q-positives and 55% of the 3Q-negatives. When compared to the clinics that was not included by the intervention and during the same period in the total county of Västerbotten, Sweden [Citation9], no significant increase in traceable clinical decision were observed (χ2 value 2.2, p = .14) ().
Figure 2. Percentage distribution of traceable decisions in dental records in relation to symptoms indicative of temporomandibular disorders (TMD). 2015 intervention constitutes decisions by dentists or dental hygienists during 2015 after education and with support of a decision tree, and 2015 Västerbotten constitutes decisions by the remaining dentists or dental hygienists in Public Dental Health Service, Västerbotten, Sweden.
The inter-rater reliability of the variable ‘TMD treatment’ and ‘Any TMD related decision’ were nearly perfect ( κ value .91, respectively).
The 3Q-positives were prescribed or recommended TMD treatment significantly more often compared to 3Q-negatives (OR 11.1, 95% CI 4.6–26.5) ().
Table 1. Frequency distribution for TMD treatment.
In total, 26% of the 3Q-positives were prescribed or recommended any TMD treatment. The most frequent TMD treatments were a referral (3.5%) and occlusal appliance (3.0%). Thirteen percent of the 3Q-positives declined prescribed or recommended treatment. No treatment was deemed necessary by the clinician among 34% of the 3Q-positives (Q1-positive: 28%, Q2-positive: 25%, and Q3-positive: 40%).
In the multiple regression model, a positive answer to Q1 (frequent pain) and younger ages predicted performed or recommended TMD treatment ().
Table 2. Multipredictor analysis of responses to the three screening questions in relation to TMD treatment among all patients (n = 398).
A majority of the individuals were examined by a dentist (80%) and there was no significant difference between 3Q-positives and 3Q-negatives (χ2 value .76, p = .383). The majority of dental care providers were women (68%).
Discussion
The main finding from this study was that the intervention based on a decision-tree did not increase the use of the 3Q/TMD in the clinical decision process in the Public dental health services. In addition, approximately 40% of individuals who screened positive to at least one of the 3Q/TMD, did not receive a traceable clinical decision in relation to their reported symptoms. Among the nonclinical factors evaluated, TMD treatment was more frequently distributed to younger patients.
Implementation science is described as the evaluation of the systematic uptake and use of evidence-based interventions. To enable a successful implementation of a method, the adaptation among clinicians is crucial. Previous studies on implementation science have highlighted that even though an intervention is introduced, there are still difficulties when striving for an incorporation in clinical practice [Citation15]. Therefore, the importance of starting an implementation with the understanding of the recipients as active agents instead of top down has been suggested [Citation20]. In addition, not only does the quality of the suggested method affect the decision-making but also a strong leadership with clear guidelines, and a functional interplay between working professionals and effective communication affect the use of the method. In our study, the ambition was to reduce the potential effects of the top down structure by providing education and motivation for the importance of the adherence to the suggested method. The intervention was also supported by managers at multiple levels within the organization. The 3Q/TMD was previously suggested to be appropriate for the identification of individuals who would benefit from a further TMD examination [Citation18]. Therefore, it could be expected that the incorporation and use of three short questions should be conveniently implemented. On the contrary, it is apparent that this additional approach still was insufficient since 40% of the individuals who screened positive, still did not receive a traceable, related decision. In a previous study on TMD treatment among dentists in the UK, it was concluded that there is need for a development and better quality evidence for decision-making related to TMD treatment [Citation16]. Furthermore, the care-givers attitudes, knowledge and interest regarding TMD can also affect the clinical decision- making. How the screening questions are asked and if they are clarified in context, to facilitate the understanding for the patient, as well as the patient´s own thoughts and knowledge about their own individual symptoms, are all factors that can affect the decision-making and hence promote the use of the new method. Since patients’ values should be incorporated in evidence-based methods in medicine, future studies could elaborate the patients’ perception and understanding of the 3Q/TMD as well as their related complaints. Taken together, there seems to be uncertainties in the decision-making process for patients with TMD in dentistry and results from this study support our previous findings. This suggests a need of an in-depth study of the decision-making process in dentistry to gain further understanding and to generate hypothesis of clinical decisions in relation to TMD.
Among the individual screening questions, a positive answer to Q1; frequent pain, was the only predictor for performed or recommended TMD treatment. A possible explanation could be a general interpretation of the Q1 to, functioning as an overall screening question about perceived pain from the orofacial region that, includes headaches, pain and locking from the TMJ. On the other hand, and from the patients’ perspective, pain intensity has been related to a perceived treatment need [Citation21], and it could therefore be reasonable that primarily patients with TMD pain indeed do need treatment. The relationship between screen positives to the individual questions and treatment need is, however, not yet established. When compared to the reference clinics, gender of examiner was not a predictor for TMD decisions in the intervention clinics. This may indicate, that the intervention still had impact on the nonclinical factors affecting the decision process.
Among the treatments provided, an occlusal appliance and referral were equally frequent, as in comparison with previous studies that reported occlusal appliances as the most frequent treatment [Citation9]. Treatments not charged for and patients who decline recommended treatment remains rare. Taken together, the implementation of the intervention does not seem to have affected the outcome of the clinical decision-making process.
It has been previously suggested that the outcome of TMD treatment is dependent on the profession of the dental examiner and that TMD treatment differs when a dental hygienist perform the examination [Citation12]. Since the knowledge and education in the field of TMD are more extended among dental students’ curriculum in comparison to that of dental hygienists’, it has been argued that there may exists a risk of missing out on TMD when check-ups are not performed by a dentist. However, in our study nor in our previous studies, we did not obtain any confirming results of such an existing risk.
Strengths and limitations
The study was designed as a case–control study, with two blinded, independent examiners. The inter-rater reliability was found to be an excellent value, which is considered a strength. The 3Q/TMD is regarded a valid tool for the identification of individuals with a probable TMD diagnosis. Therefore, it is also reasonable to assume an awareness of a potential treatment need among the screen positive patients. However, the general potential risk for bias when retrieving and analyzing retrospective data (dental records) could be regarded as a limitation of our study. All told, we still regard the results generalizable for Sweden and comparable countries.
Conclusions
Despite the specific intervention aimed at an optimal use of an already existing screening tool, the indicated undertreatment of patients with TMD remains. However, the intervention seems to affect gender biases in dentistry. Future studies are needed to gain a deeper understanding of the factors that affecting the clinical decision-making process for patients with TMD in dentistry.
Acknowledgements
We extend our sincere gratitude’s to head-of-chief Per-Ivan Marklund, all four floor-managers, and colleagues at the clinics participating in this study at the Public dental health services in Västerbotten, and by that, enabling this study.
No potential conflict of interest was reported by the authors.
Disclosure statement
Additional information
Funding
References
- Okeson JP. Management of temporomandibular disorders and occlusion. 7th ed. Maryland Heights (MI): Mosby; 2013.
- Dworkin SF, LeResche L. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord. 1992;6:301–355.
- Breivik H, Collett B, Ventafridda V, et al. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain 2006;10:287–333.
- Velly A, List T, Lobbezoo F. Comorbid pain and psychological conditions in patients with orofacial pain. Orofacial pain: recent advances in assessment, management, and understanding of mechanisms. Washington (DC): IASP Press; 2014.
- Macfarlane GJ. The epidemiology of chronic pain. Pain 2016;157:2158–2159.
- Rosenberg WM, Sackett DL. On the need for evidence-based medicine. Therapie 1996;51:212–217.
- Sidebottom AJSF, Cascarini L. Current management of temporomandibular joint (TMJ) disease. J Arthritis 2014;3:3.
- National Board of Health and Welfare. 2017 [updated 2016 Apr 12;2017 Jan 30]. Available from: http://www.socialstyrelsen.se/statistik/statistikdatabas/tandhalsa
- Lövgren A, Karlsson Wirebring L, Häggman-Henrikson B, et al. Decision-making in dentistry related to temporomandibular disorders: a 5-yr follow-up study. Eur J Oral Sci. 2018;126:493–499.
- Lövgren A, Marklund S, Visscher CM, et al. Outcome of three screening questions for temporomandibular disorders (3Q/TMD) on clinical decision-making. J Oral Rehabil. 2017;44:573–579.
- Chisnoiu AM, Picos AM, Popa S, et al. Factors involved in the etiology of temporomandibular disorders – a literature review. Clujul Med. 2015;88:473–478.
- Lindfors E, Tegelberg A, Magnusson T, et al. Treatment of temporomandibular disorders – knowledge, attitudes and clinical experience among general practising dentists in Sweden. Acta Odontol Scand. 2016; 74:460–465.
- Hajjaj FM, Salek MS, Basra MK, et al. Nonclinical influences on clinical decision-making: a major challenge to evidence-based practice. J R Soc Med. 2010; 103:178–187.
- Tversky A, Kahneman D. Judgment under uncertainty: heuristics and biases. Science 1974;185:1124–1131.
- Lukas CV, Holmes SK, Cohen AB, et al. Transformational change in health care systems. An organizational model. Health Care Manage Rev. 2007;32:309–320.
- Durham J, Exley C, Wassell R, et al. ‘Management is a black art’–professional ideologies with respect to temporomandibular disorders. Br Dent J. 2007;202:E29; discussion 682–683.
- Bonabeau E. Don’t trust your gut. Harv Bus Rev. 2003;81:116–123, 130.
- Lövgren A, Visscher CM, Häggman-Henrikson B, et al. Validity of three screening questions (3Q/TMD) in relation to the DC/TMD. J Oral Rehabil. 2016;43:729–736.
- Lövgren A, Häggman-Henrikson B, Visscher CM, et al. Temporomandibular pain and jaw dysfunction at different ages covering the lifespan – a population based study. Eur J Pain. 2016;20:532–540.
- Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;236:42.
- Rollman A, Visscher CM, Gorter RC, et al. Care seeking for orofacial pain. J Orofac Pain. 2012;26:206–214.