Abstract
Objective: Organizations and state agencies that provide dental care continuously face various and novel demands related to the need for dental care. However, rearrangements of work tasks by reducing the number of tasks performed by dental personnel might make the work more monotonous, repetitive, and static within an organization. The aim of this study is to compare how two dental work organizations, with different staffing and clinic size, are perceived by dental personnel focusing on physical and psychosocial conditions, leadership, work ability and presenteeism in 2012 and 2014.
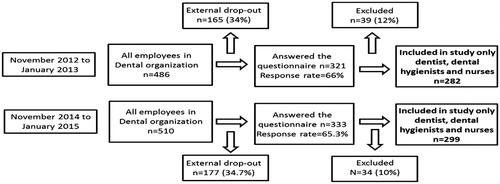
Material and Methods: This repeated cross-sectional study included personnel from the Public Dental Service in Sweden. There were 282 dentists, dental hygienists, and dental nurses who answered a questionnaire 2012 and 299 in 2014.
Results and conclusion: In 2012, nine per cent of medium clinics reported poor leadership compared with 27% in 2014. For large clinics, 17% perceived poor leadership in 2012 compared with 31% in 2014. A higher proportion of the employees reported presenteeism due to high physical load (43%) and high psychosocial load (21%) in 2014 compared with 31% and 13% in 2012. These results indicate the need for work place interventions promoting health among dental employees.
Introduction
Organizations and state agencies that provide dental care continuously face various and novel demands related to the need for dental care. When meeting these demands, treatment and workplace strategies need to change accordingly. Such changes in turn influence the planning of staffing to ensure that the numbers of dentists, dental hygienists, and dental nurses are optimal in relation to the local demands. Currently Sweden is planning to address the shortage of qualified dentists. One approach to resolving this issue to have an equal or larger number of dental hygienists in relation to the number of dentists in the clinics and another is to delegate the work tasks between the Odontological Health Personnel (OHPs), which has been shown to be effective in previous studies [Citation1–3].
Within the Swedish Public Dental Service, the OHPs include dentists, dental hygienists, and dental nurses working as a team and sharing the same objectives, that is, to treat and prevent oral health diseases and to promote oral health for all individuals in society [Citation4]. However, rearrangements of work tasks by reducing the number of tasks performed by dental personnel might make the work more monotonous, repetitive, and static within an organization, and this has been shown to increase the stress levels perceived by staff [Citation5]. Increased levels of work-related stress are a common risk for physical problems, leading to impaired physical and psychosocial health within dental care [Citation5–9].
OHPs are seen to be at high risk for musculoskeletal disorders due to the tasks they perform at work which are monotonous, repetitive, and static [Citation10], which might increase the risk for muscular imbalance, neuromuscular inhibition, pain, and dysfunction [Citation7,Citation8,Citation10]. Physical problems, predominantly back pain, have also been regularly reported from OHPs [Citation6,Citation11–13], and the relationship between physical and psychosocial problems in the work environment and sick absence has been reported previously among dental staff members [Citation5,Citation14,Citation15]. Work organization can affect employees' physical and psychosocial work environment, and the reorganization of workplaces often means not only a change in itself but also restructuring and downsizing as well as changes in the composition of the workgroup and management [Citation16]. This can have a subsequent effect on the mental and physical health of the employees and thus negatively affect their ability to work.
An earlier study described changes in the division of labor and tasks within public dentistry in relation to OHP work demands, health, and work ability in Sweden [Citation9]. The results showed that OHPs in clinics where the proportion of dental hygienists is [4]equal/larger than the proportion of dentists (HDH1) clinics reported significantly greater psychosocial demands and more sleep problems due to work compared with medium large clinics (defined as between 10 to 20 employees) where the proportion of dentists [Citation4] is larger than the proportion of dental hygienists (HD2), and large HD clinics (defined as more than 20 employees). OHPs in HDH workplaces also reported significantly more sleep problems than small HDH clinics (defined as fewer than 10 employees). A majority of the OHPs also reported a poor physical work environment regardless of workplace organization. This study followed the workers who participated in our previous work for 24 months in order to document the patterns of changes concerning workload and health among dental staff.
The aim of this study is to compare how two dental work organizations, with different staffing and clinic size, are perceived by dental personnel focusing on physical and psychosocial conditions, leadership, work ability and presenteeism in 2012 and 2014 [Citation1].
Material and methods
The Dental Organization in Transition in Sweden survey (DOiT), is a repeated cross-sectional study from the Public Dental Service in a Swedish region during the period from November 2012 to January 2013, all 486 employees in the dental organization were given the opportunity to answer the DOiT survey, and 321 employees responded (66% response rate). The same questionnaire was administered again between November 2014 and January 2015 to all 510 employees in the dental organization, and 333 employees responded (65.3% response rate). When participating clinics were contracted regarding response rate, lack of time and lack of willingness to respond were reported as reasons for non-responding. For this study only dentists, dental hygienists, and dental nurses from clinics, that is, OHPs were included (n = 282 in 2012 and n = 299 in 2014) ().
Dental clinics were divided by size into Small Clinics (10 or fewer employees), Medium Clinics (between 11 and 20 employees), and Large Clinics (more than 20 employees). The comparisons were made at the group level between 2012 and 2014. HD clinics included workplaces where the proportion of dentists is [Citation4] larger than the proportion of dental hygienists, and HDH clinics included those in which the proportion of dental hygienists is [Citation4] equal/larger than the proportion of dentists. Large HDH clinics and small HD clinics were not studied due to lack of data.
The questionnaire included questions on Demographics, Workplace, Physical and Psychosocial conditions, Leadership, Psychosomatic conditions, Pain and disorders of the musculoskeletal system, Work ability, and Presenteeism. All items are described in full in a previous article [Citation9].
The OHPs from each dental clinic were first informed about the study by their supervisors, but participation was voluntary. The questionnaire was developed as a web survey using the EsMaker NX3 software, with the link emailed to the participants. The DOiT project was approved by the Regional Ethical Review Board in Linköping (ref. no: 2012/186-31).
Exposure
Workplace physical conditions
The physical work conditions evaluated in this study was created with the same items as from an exploratory factor analysis in a previously conducted study [Citation8,Citation17]. Physical work conditions were evaluated with six items scored on a scale of 1 = ‘Not at all’ to 10 = ‘To a high degree’. The same procedure was conducted for Precision demands (three items) and Work posture (three items). A higher score reflects poorer physical conditions; for example, one question asks, ‘Does your work usually involve many repetitive motions?’
Perceived exertion after the end of the day
Strain in different body locations were evaluated for the Eyes, Neck, Shoulders, Upper back, Lower back, and the left and right of the Upper arm, Elbows, Wrists, Hands/fingers [Citation18]. An example of one such question is, ‘How strenuous for your eyes have you perceived your work to have been at the end of a normal working day in the past month?’ Each location was scored from 1 = Very, very little to 15 = Very, very strenuous. The Perceived exertion factor was dichotomized (1–7 and 8–15), and the proportions of those reporting scores from 8 to 15 are presented in percentages. A higher score reflects greater perceived exertion.
Workplace psychosocial conditions
Psychosocial conditions were evaluated with 15 items and also grouped into four separate factors by the structure from the previous explorative factor analysis [Citation8,Citation17], based on the middle value, into three factors containing conceptually related items: Poor psychosocial demands (six items), Poor work control (four items), and Poor social support (five items) [Citation8,Citation17]. Each item was scored on a scale of 1 = ‘Not at all’ to 10 = ‘To a high degree’. A higher score reflects poorer psychosocial conditions; for example, one question asks; ‘Does your work often demand maximum concentration for considerable periods at a time?’ Three items evaluated poor leadership and were scored on a similar scale, with a higher value indicative of poorer leadership [Citation19]. An example of one such question is, ‘Does your immediate superior show appreciation when you do a good job?’
The factors of Precision demands, Work posture, Psychosocial demands, Social support, and Leadership were then dichotomized (1–5 and 6–10) on the middle value, and the proportions of 6–10 indicates the negative aspect of exposure at work and presenteeism, are presented in percentages.
Outcome
Pain and symptoms of the musculoskeletal system
The presence of pain and symptoms of the Neck, Shoulders, Elbows, Wrists/hands, Upper back, Lower back, One hip or both, One knee or both, and One ankle or both were identified with nine items [Citation20] with dichotomous ‘Yes/No’ options. Only those who reported problems (Yes) in any of these nine regions are presented as percentages.
Psychosomatic conditions
The presence of psychosomatic conditions was evaluated with four items – Sleep problems, Stomach disturbances, Difficulty disconnecting from work during leisure time, and Headaches [Citation19]. Each item was scored on a 10-point scale from 1 = ‘Not at all’ to 10 = ‘To a high degree’. A higher score reflects poorer psychosomatic conditions. The items were then dichotomized (1–5 and 6–10), and the proportions of those reporting 6–10 are presented in percentages. An example of one of the statements is, ‘Has frequent headaches due to work’.
Work ability
Work ability was evaluated with three items [Citation21]. The two items ‘Your work ability in relation to physical demands’, and ‘Your work ability in relation to psychosocial demands’ was measured with five options and were dichotomized into ‘good’ and ‘poor’ work ability in relation to the physical and psychosocial demands of their job. The response options of ‘Very good’, ‘Fairly good’, and ‘Reasonably good’ were grouped as ‘Good’, and the options of ‘Less good’ and ‘Poor’ were grouped as ‘Poor’. For the third item, ‘Due to your health, do you think that you can work at your current job in two years’ time’, which was originally measured with three options, the option ‘Hardly’ (Poor) remained as one option, while the options ‘Maybe’ and ‘Yes’ formed the second option. A fourth item, ‘Considering your work and work environment, how satisfied are you?’, was measured on an eleven-point scale (0–10), where a higher score reflects poorer psychosomatic conditions. The proportion of participants scoring higher than five is presented as a percentage.
Work absence
Sickness absence because of physical or psychosocial problems was evaluated with two separate items, both with five possible response options: ‘No’, ‘Yes, less than a week’, ‘Yes, one to four weeks’, ‘Yes, four weeks to two months’, and ‘Yes, more than two months’. Responses were regrouped for the both items to form a dichotomous variable of ‘No’ and ‘Yes’ for Sickness absence caused by physical and psychosocial load. The number of ‘Yes’ responses is presented as a percentage.
Presenteeism
Presenteeism means that the employee is ill and has problems with the physical work environment, such as neck pain or of psychosocial reasons, such as stress symptoms, but still at work and working. Presenteeism due to physical or psychosocial problems was evaluated with two separate items with four possible response options – ‘Not at all’, ‘Sometimes’, ‘Often’, and ‘Always’ [Citation19]. Responses were combined to form the dichotomous variable ‘Not at all’, renamed ‘No Presenteeism’, and the options ‘Sometimes’, ‘Often’, and ‘Always’ were combined to form the category ‘Presenteeism’. In this study, responses to the option ‘Presenteeism’ are presented as a percentage.
Statistics
Descriptive statistics are shown in percent, frequencies (n), and 95% confidence intervals. Bootstrapping was used to calculate the 95% confidence interval. Bootstrapping is the inference about a population from sample data that can be modelled by resampling the data and making new inferences in an iterative manner. This process is repeated a number of times (typically 1000 or 10,000 times), and it provides an estimate from which we can answer questions about the dispersion in the data. Chi-square analysis (the likelihood ratio) was used for group comparisons over time between 2012 and 2014 and between clinics in 2012 and between clinics in 2014. Due to the large number of tests, the limit for significance was set at α = .01. Data processing was performed using SPSS version 22 (IBM Corp, Armonk, New York, USA).
Results
There were a significantly greater proportion of HDH clinicians in 2012 (61%) and 2014 (64%) working in medium workplaces compared with HD clinics (55-52%) in 2012 and 2014. There was no HD staff who worked at small clinics in 2012 and 2014. There was also no HDH staff who worked at large clinics in 2012 and 2014. No significant differences between HD and HDH clinicians were found for the distribution of gender, age, profession, years in dental service, or working hours per week in 2012 or in 2014 ().
Table 1. Characteristics of participants in frequencies (n), percentages (%), and 95% confidence intervals (95%CI).
Exposure
Workplace physical and psychosocial conditions and perceived exertion comparisons between 2012 and 2014
shows a difference for impaired physical exposure with 86% of the employees in all clinics in 2012 reporting poor work posture compared with 92% of employees in 2014. Another significant change was observed in the proportion of those reporting poor leadership that increased from 17% in 2012 to 30% in 2014.
Figure 2. Summary of changes in percent for separate clinics and cumulative percent for all clinics together. Data are from 2012 and 2014 and are distributed as to whether the clinic has an HD or HDH organization type. *p < .05, **p < .01, ***p < .001.
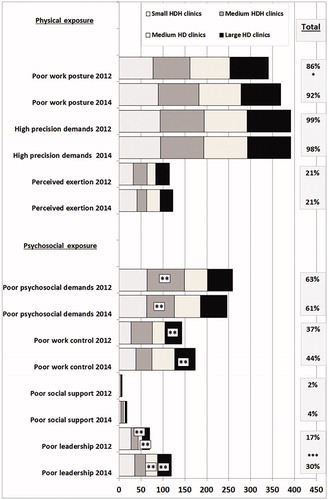
When considering the clinics separately, a significantly greater proportion of employees in large HD clinics (31%) and medium HD clinics (27%) reported poor leadership in 2014 compared with large HD clinics (17%) and medium HD clinics (9%) in 2012. Both medium HD clinics and large HD clinics reported poorer leadership (27% and 31%, respectively) compared to 2012.
Improvements were evident in the medium HDH clinics, with a lower proportion (63%) reporting poor psychosocial demands in 2014 compared with 85% in 2012. In 2014, large HD clinics reported poorer work control (47%).
Outcome
Pain and symptoms of the musculoskeletal system, work ability, presenteeism and sickness absence of physical reasons. Comparisons between 2012 and 2014
In , more than half reported pain and/or disorders during the past 12 months in the neck, shoulders, upper back, and lower back both in 2012 and 2014 among all employees. In addition, about half of all employees (55% in 2012 and 51% in 2014) reported pain and/or some disorders in the lower limbs during the past 12 months. There was a significant increase in presenteeism caused by high physical workload (43%) in 2014 compared with 31% in 2012. Considering the clinics separately, there was a tendency for increased presenteeism for large HD clinics in 2014 at 43% compared with 25% in 2012.
Figure 3. Summary figure of the changes in percent for separate clinics and in cumulative percent for all clinics together between 2012 and 2014 and distributed according to HD and HDH organization type. *p < .05, **p < .01.
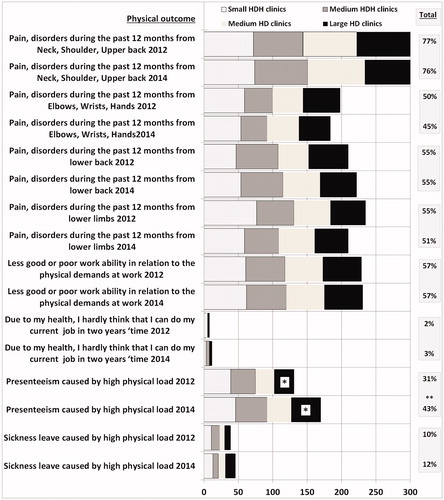
In both 2012 and 2014, 57% reported ‘poor’ work ability in relation to the physical demands at work ().
Pain and symptoms of the musculoskeletal system, work ability, presenteeism and sickness absence of psychosocial reasons. Comparisons between 2012 and 2014
In all employees, 52% and 55% reported ‘poor’ work ability in relation to the psychosocial demands at work in 2012 and 2014, respectively (). In 2014, there was a tendency for deterioration in psychosomatic symptoms, with 20% of employees from all clinics reporting frequent headache and 22% reporting difficulty disconnecting from work compared with 13% and 15%, respectively, in 2012. Furthermore, of all employees, 21% reported presenteeism caused by high psychosocial demands in 2014 compared with 13% in 2012, which suggests a tendency toward deterioration.
Figure 4. Summary figure of the changes in percent for separate clinics and in cumulative percent for all clinics together between 2012 and 2014 and distributed according to HD and HDH organizational type. *p < .05.
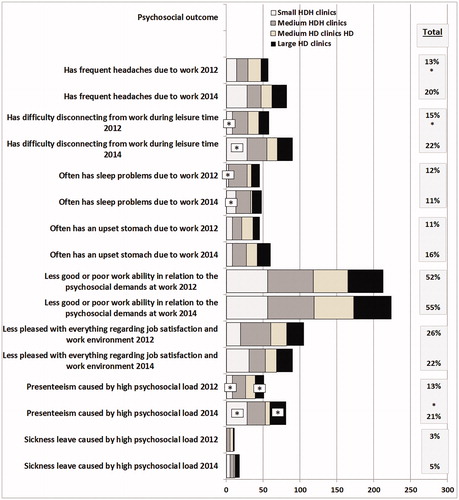
In 2014, more employees in small HDH clinics reported difficulty disconnecting from work during leisure time (28%) and sleep problems due to work (13%) compared with 8% and 3%, respectively, in 2012.
In addition, there is a significant larger proportion of presenteeism due to high psychosocial load was reported from small HDH clinics (28%) and large HD clinics (22%) in 2014 compared with 8% and 2%, respectively in 2012.
Discussion
The focus of this study was to compare different proportions of staffing and clinic size in dental organizations in terms of physical and psychosocial exposure, health, sickness, leadership, and work ability. Employees in the dental organization studied here reported deterioration in the ability to make decisions about their work and high psychosocial load. This was especially found in large clinics with more dentists than dental hygienists (HD). The employees at the large and medium HD clinics also perceived an increase in poor leadership during the study period. In addition, employees working in large HD clinics reported increased presenteeism caused by high physical load. This shows a conceivable relationship, and there are studies that support a connection between poor leadership, poor social support, and musculoskeletal disorders [Citation22,Citation23], and relationships between physical and psychosocial problems in the work environment and sick absence have previously been reported among dental staff members [Citation5,Citation14,Citation15].
There is also some evidence that organizational changes such as transferring certain tasks from dentists to dental hygienists and dental nurses might change the physiological working conditions [Citation24] and might make the work more monotonous, repetitive, and static for dentists. Therefore, it is not unthinkable that there are organizational changes that contribute to negative effects in the work environment. However, in this study, it was primarily employees in large HD clinics who reported a more deteriorated work environment with increased presenteeism. A similar deterioration was not seen for clinics with equal or more dental hygienists than dentists (HDH). That the deterioration was more pronounced in HD clinics might be at least partly explained by the fact that these clinics always are larger, and this might adversely affect the working environment. These clinics are also more often located in urban areas with more patients and thus greater workloads. However, the results also show some deterioration in the working environment for HDH clinics, which partly can be an expression of a generally increased workload in dental care. In small HDH clinics, there were a greater proportion of employees who reported difficulty in disconnecting from work, sleep problems, and presenteeism caused by psychosocial factors. Small clinics are usually found in rural areas, and in recent years, many small clinics have been shut down and the patients moved to larger clinics, which can create an air of uncertainty in the workplace. It is also likely that dentists and dental hygienists in small workplaces work alone and have no colleagues to discuss things with, which can be perceived as negative. Transferring tasks from dentists to dental hygienists and dental nurses also means that these occupational groups have more work tasks to perform than before, and in addition to increased working pace such transfers might also involve increased diversity in the work and more interesting tasks.
This study also shows an improvement for medium HDH clinics, although a poor level of psychosocial demands was reported in 2012. This improvement was apparent only for this type of clinic, which makes the result more difficult to interpret and might be indicative of a temporary deterioration for 2012. Moreover, the results in 2014 show that these clinics do not deviate in any major way from the other clinics.
Generally, all employees tended to indicate an increased difficulty in disconnecting from work and increased presenteeism for psychosocial reasons. Severe physical load is still the most apparent work factor in dentistry regardless of the type of dental organization structure, and poor work positions also deteriorated for all employees between 2012 and 2014, a result that is supported by a previous study [Citation25]. Almost all employees reported high precision demands both in 2012 and 2014, and this shows that physical load in general continues to pose the greatest risk of ill health for employees in dentistry. This is probably the case even if a smaller proportion reported physical exertion due to work after the end of the day. One possible explanation could be that dental work often involves low muscular load for prolonged periods of time with few breaks for recovery [Citation26]. This work is most often conducted in static forward bent and twisted postures in order to be able to see into the patient's mouth. It is likely that such burdensome work positions lead to the large proportion of the treating staff reporting problems in the upper part of the body [Citation27]. Around half or more of the employees reported pain and/or disorders in the past 12 months with neck and shoulder regions being the most commonly affected in both 2012 and 2014. It has been reported that neck and shoulders disorders increase the risk for reduced work ability [Citation28]. In this study, more than half of the employees estimated that they had reduced work ability in relation to their physical or psychosocial demands at work. Employees with self-reported musculoskeletal disorders had more than twice as high a risk of low work ability compared to healthy employees. In another study, employees with mental disorders had six times higher risk for low work ability. This suggests a certain connection between pain and disorders and work ability [Citation29] as well as presenteeism, and these can be costly for the employer [Citation30]. However, the concept of presenteeism is not well defined, and some caution in the interpretation of these results is necessary [Citation31]. It has been shown that there is a connection between presenteeism and work production in such a way that production is negatively affected and that costs increase [Citation30,Citation32]. Our results indicate that presenteeism due to both physical and psychosocial factors may be associated with high work demands. However, the number of employees who reported sick absence was almost unchanged between 2012 and 2014, and at a low level. This might be an indication that the work load and the symptoms are still manageable and are not an obstacle to work. It has been shown that sickness absence is related to motivation and work ability. The Model for Illness Flexibility [Citation33] identifies the complex relationship between a person's state of health, their ability to perform work tasks, and their ability to meet attendance/absence requirements (ought/should) and to respond to attendance/absence incentives (motivation). It does not seem inconceivable that dental professionals perceive both a strong motivation and duty to be at work despite poor working conditions and work-related ill health, and this might explain the difference between increasing presenteeism and decreasing sickness absence as is shown in present study.
Methodological considerations’
A weakness in this study is that the comparisons between 2012 and 2014 were analysed at the group level, and there was a risk that the new employees participating in 2014 but not participating in 2012 deviated from the employees who participated in 2012 and vice versa. During the period, there was a turnover of employees, and the total number of employees also increased by about 5%. The choice for making group comparisons was based on the fact that in a pairwise comparison the group size would drastically decrease (n = 174) and thus significantly reduce the power of the study. The fact that about 65% answered the questionnaire on both occasions might be due to staff turnover and a smaller proportion of new staff (a 5% increase in 2014) or that employees had been specifically selected in certain years or could only answer the questionnaire on one occasion.
However, we made the assumption that most of the new employees were unlikely to deviate to a significant extent from other employees. A response rate of around 65% while rather good may have posed a certain risk to the external validity of the results when a 35% large proportion of employees do not respond to the survey. However, there are indications that the risk is not likely to be high because the reports we received point to lack of time or willingness in answering the questionnaire. Another aspect to consider is the so-called healthy worker effect which means the exclusion of unhealthy workers at employment during the study period and that healthy workers remain and will constitute a larger proportion of the study population. However, the conclusion is that this effect cannot be particularly pronounced since the time span between the two measuring points is only two years. The conclusion is therefore that the external validity is acceptable.
The strength of this study is the inclusion of all dentistry units in an entire county council in eastern Sweden, which means that clinics of different sizes, with different staff compositions, and in rural and urban areas are represented, indicating that the study is representative.
Conclusion
This repeated cross sectional study shows a generally reported deterioration of Work posture and Leadership, increased presenteeism, and larger proportions reporting headache caused by work and difficulty in discontinuing work at leisure, and these changes vary only little between organizational type or clinic size on these responses. These results indicate the need for work place interventions promoting health among dental employees.
Disclosure statement
No potential conflict of interest was reported by the authors.
Notes
Notes
1 HDH = Clinics with an [Citation4] equal/larger proportion of dental hygienists than dentists.
2 HD = Clinics with a [Citation4] larger proportion dentists than dental hygienists.
References
- Ordell S. Organisation and management of public dentistry in Sweden. Past, present and future. Swed Dent J Suppl. 2011;210:10–92.
- Ordell S, Unell L, Soderfeldt B. An analysis of present dental professions in Sweden. Swed Dent J. 2006;30(4):155–164.
- National Board of Health, Sweden 2007.
- Hasenfeld Y. Human Services as Complex Organizations. London, UK: SAGE Publications, Inc; 2010. pp. 608.
- Winkel J, Westgaard RH. A model for solving work related musculoskeletal problems in a profitable way. Appl Ergon. 1996;27(2):71–77.
- Sakzewski L, Naser-Ud-Din S. Work-related musculoskeletal disorders in Australian dentists and orthodontists: risk assessment and prevention. Work. 2015;52(3):559–579.
- Jonker D, Rolander B, Balogh I, et al. Rationalisation in public dental care - impact on clinical work tasks and mechanical exposure for dentists - a prospective study. Ergonomics. 2013;56(2):303–313.
- Rolander B, Jonker D, Winkel J, et al. Working conditions, health and productivity among dentists in Swedish public dental care–a prospective study during a 5-year period of rationalisation. Ergonomics. 2013;56(9):1376–1386.
- Rolander B, Wahlin C, Johnston V, et al. Changes in division of labour and tasks within public dentistry: relationship to employees work demands, health and work ability. Acta Odontol Scand. 2016;74(6):471–479.
- Yamalik N. Musculoskeletal disorders (MSDs) and dental practice Part 2. Risk factors for dentistry, magnitude of the problem, prevention, and dental ergonomics. Int Dent J. 2007;57(1):45–54.
- Lindfors P, von Thiele U, Lundberg U. Work characteristics and upper extremity disorders in female dental health workers. Jrnl of Occup Health. 2006;48(3):192–197.
- Sakzewski L, Naser-Ud-Din S. Work-related musculoskeletal disorders in dentists and orthodontists: a review of the literature. Work. 2014;48(1):37–45.
- Ylipaa V, Arnetz BB, Benko SS, et al. Physical and psychosocial work environments among Swedish dental hygienists: risk indicators for musculoskeletal complaints. Swed Dent J. 1997;21(3):111–120.
- Kuoppala J, Lamminpaa A, Liira J, et al. Leadership, job well-being, and health effects–a systematic review and a meta-analysis. J Occup Environ Med. 2008;50(8):904–915.
- Petren V, Petzall K, Preber H, et al. The relationship between working conditions and sick leave in Swedish dental hygienists. Int J Dent Hyg. 2007;5(1):27–35.
- Salin D. Ways of Explaining Workplace Bullying: A Review of Enabling, Motivating, and Precipitating Structures and Processes in the Work Environment. Hum Relat. Swedish School of Economics and Business Administration, Department of Management and Organisation Contract No.: 10. 2003.
- Rolander B, Bellner AL. Experience of musculo-skeletal disorders, intensity of pain, and general conditions in work – The case of employees in non-private dental clinics in a county in southern Sweden. Work. 2001;17(1):65–73.
- Lindegard A, Wahlstrom J, Hagberg M, et al. Perceived exertion, comfort and working technique in professional computer users and associations with the incidence of neck and upper extremity symptoms. BMC Musculoskel Disord. 2012;13:38.
- Ekberg K, Bjorkqvist B, Malm P, et al. Controlled two year follow up of rehabilitation for disorders in the neck and shoulders. Occup Environ Med. 1994;51(12):833–838.
- Kuorinka I, Jonsson B, Kilbom A, et al. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl Ergon. 1987;18(3):233–237.
- Tuomi KIJ, Jahkola A, Katajarinne L, et al. (Ed). Work ability index 2nd revised edn. Helsinki: Finnish Institute of Occupational Health.1998
- Aasa U, Barnekow-Bergkvist M, Angquist KA, et al. Relationships between work-related factors and disorders in the neck-shoulder and low-back region among female and male ambulance personnel. J Occup Health. 2005;47(6):481–489.
- Cole DC, Ibrahim SA, Shannon HS, et al. Work correlates of back problems and activity restriction due to musculoskeletal disorders in the Canadian national population health survey (NPHS) 1994-5 data. Occup Environ Med. 2001;58(11):728–734.
- Hertting A, Theorell T. Physiological changes associated with downsizing of personnel and reorganisation in the health care sector. Psychother Psychosom. 2002;71(2):117–122.
- Alexopoulos EC, Stathi IC, Charizani F. Prevalence of musculoskeletal disorders in dentists. BMC Musculoskelet Disord. 2004;5(1):16.
- Rolander B, Jonker D, Karsznia A, et al. Evaluation of muscular activity, local muscular fatigue, and muscular rest patterns among dentists. Acta Odontol Scand. 2005;63(4):189–195.
- Akesson I, Hansson GA, Balogh I, et al. Quantifying work load in neck, shoulders and wrists in female dentists. Int Arch Occup Environ Health. 1997;69(6):461–474.
- Jay K, Friborg MK, Sjogaard G, et al. The consequence of combined pain and stress on work ability in female laboratory technicians: a cross-sectional study. Int J Environ Res Public Health. 2015;12(12):15834–15842.
- Wolf I, Friede T, Hallier E, et al. Work-related outcomes in randomised placebo-controlled pain trials: a systematic review and meta-analysis. J Occup Med Toxicol. 2014;9(1):25.
- Vanni K, Neupane S, Nygard CH. An effort to assess the relation between productivity loss costs and presenteeism at work. Int J Occup Saf Ergon. 2017;23(1):33–43.
- Vingard E, Alexanderson K, Norlund A. Swedish Council on Technology Assessment in Health Care (SBU). Chapter 10. Sickness presence. Scand J Public Health Suppl. 2004;63:21621.
- Vanni K, Virtanen P, Luukkaala T, et al. Relationship between perceived work ability and productivity loss. Int J Occup Saf Ergon. 2012;18(3):299–309.
- Johansson G, Lundberg I. Components of the illness flexibility model as explanations of socioeconomic differences in sickness absence. Int J Health Serv. 2009;39(1):123–138.