Abstract
Aim
Poor oral health is related with bacteraemia that may lead to endocarditis in children with congenital heart disease (CHD). The aim of this study was to conduct a systematic literature review to compare caries prevalence in children (<18 years of age) with CHD with healthy children.
Material and methods
A literature search of studies from two online databases (Pubmed (MEDLINE) and Scopus) published from January 2000 to October 2019 using Medical subject heading terms Congenital Heart Disease, Congenital Heart Defect, and Caries was done, and manual search from the reference lists of selected publications. PICO (Patient/Population, Intervention, Comparison group, and Outcome) criteria was applied. Quality of the publications was assessed with the modified Newcastle-Ottawa scale.
Results
The search resulted in 151 articles of which nine fulfilled the inclusion criteria. Caries prevalence was significantly higher in children with CHD compared to healthy children in three out of nine studies. Information on predisposing background factors was limited but difference in caries prevalence was not attributed to SES. The quality of the studies varied.
Conclusions
Although evidence is limited, the current literature indicates that children with CHD experience a higher caries prevalence compared to healthy children.
Introduction
The human heart develops during early embryogenesis with chambers, septa and valves formed by the end of 9 weeks of gestation. A disturbance in this process may result in an anomaly, i.e. a congenital heart defect (CHD). These form a substantial part of major congenital anomalies in children with an incidence of 7–8 cases per 1000 live births [Citation1].The maintenance of optimal oral health in children with CHD is important. The risk of infective endocarditis is increased in children with major CHD and endocarditis prophylaxis is recommended [Citation2,Citation3].The risk for bacteraemia is more common during daily oral hygiene routines, such as tooth brushing, than during dental treatment [Citation4].
Oral health is a key indicator of overall health, well-being and quality of life. According to the World Health Organization (WHO), oral health is a state of being free from mouth and facial pain, and oral diseases and disorders that limit an individual’s capacity in biting, chewing, smiling, speaking and psychosocial well-being. Tooth decay, i.e. dental caries, is the most prevalent infectious disease in man and affects nearly 500 million children around the world [Citation5]. Dental caries is a multifactorial oral disease that is unevenly distributed. Although the prevalence of caries has decreased among children overall, there are important predisposing factors in the general population. Socioeconomic status (SES; e.g. mother’s and father’s years of education and nationality), smoking and inferior parental oral health are considered as major predisposing factors for caries development in children [Citation6].
Chronic disease with or without challenges in family functioning can also lead to a higher caries prevalence among children. Many factors may predispose children with CHD to develop caries during early childhood. Developmental enamel disturbances of the tooth enamel have been reported in children with CHD [Citation7], and hypomineralization defects, in particular, make teeth more vulnerable to early childhood caries. Factors related with CHD management in children challenge caregivers directly or indirectly in maintaining child’s oral health. Heart failure related increased need of calories lead to frequent dietary intake including additional meals during night-time. Medications are often provided in conjunction with sweetened yoghurt or jam, and sweets may be used for motivational purposes. Recurrent infections in early childhood can lead to an increased need of fluids during night-time and the fluids used are occasionally sweetened as well [Citation8]. Diuretics decreases the amount of saliva production [Citation9] which increases the risk for caries as the saliva serves as an important buffer in neutralising the acid producing bacteria.
Treatment of early caries confers risks to children with CHD. Dental treatments during early life commonly involve procedures performed under general anaesthesia, due to difficulties in co-operation related with age and development. As many anaesthetics alter hemodynamics, general anaesthesia is considered a high-risk procedure for children with severe CHD forms, and thus performed in tertiary care settings only.
By identifying caries in children with CHD, health care professionals could potentially implement reasonable and cost-effective preventive measures to address the problem in the early stages. Gaps in parental knowledge could potentially be addressed with counselling [Citation10]. However, information on caries prevalence in CHD children varies. Many of the published studies show high caries prevalence and other oral health problems among children with CHD, while similar and lower caries prevalence in comparison to healthy children have also been reported. Therefore, the aim of this study was to conduct a systematic review of dental caries prevalence in children (<18 years of age) with CHD in comparison with healthy children.
Material and methods
Search strategy and selection of publications
The search for all the relevant publications on dental caries prevalence in children with CHD was performed in Pubmed (Medline) and Scopus, with the search limited to articles published between January 2000 and October 2019 to review contemporary and relevant studies for the current and future paediatric population. In addition, we performed a manual search from the reference lists of the selected publications. The Medical Subject Heading (MeSH) terms used for search in Pubmed and search terms used for Scopus, were ‘Congenital Heart Disease’, ‘Congenital Heart Defect’, and ‘Caries’.
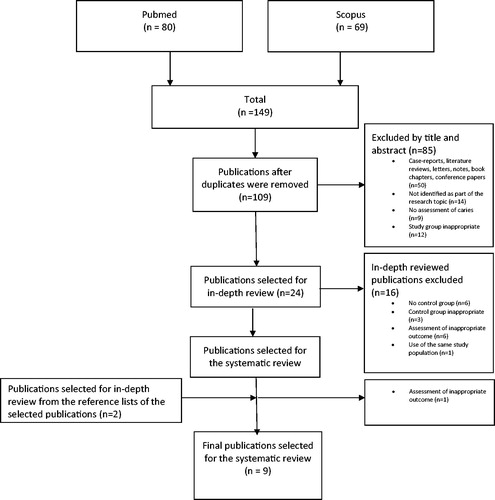
After the literature search was performed the publication selection process was conducted. The selection of the studies is described in detail in . One investigator (EK) screened the articles from the primary search by title and abstract following removal of duplicate studies, where after case-reports, letters, notes, book chapters, conference papers or studies that did not fit the inclusion criteria were excluded.
Publications that were not excluded based on the title and abstract, were then included in full text for in-depth assessment according to PICO criteria (Patient/Population, Intervention, Comparison, Outcome) by two independently working investigators (EK and MB) [Citation11].
The selected studies had to include children under 18 years of age (Population) with congenital heart disease (Intervention/exposure), and include a comparison group of healthy children (Comparison). Only studies that reported dental caries according to the definition by the WHO [Citation12] as an outcome (Outcome) in cohort or cross-sectional study settings (Study design) were included. Furthermore, studies had to be peer-reviewed and written in English. Studies including CHD children with other comorbidities or syndromes (e.g. 22q11, Turner or Down syndrome) and children with acquired heart diseases or heart transplant recipients were included. Consensus between investigators was obtained by discussion. There was a strategy in case of disagreement to consult a third reviewer, but this was never needed. The in-depth review and careful assessment resulted in nine studies selected for the systematic review.
Data extraction
Information from the articles was collected independently by two investigators (EK and MB) using a predefined standard data collection form. Agreement was assessed by discussion. Information on author, year of publication, country, and study design was collected. Type of CHD was collected and categorized by one of the investigators (TS) as mild (grade 1), simple (grade 2), or complex-type (grade 3–4). Further data included sample size of patients and controls, age of study subjects (range and mean (SD), inclusion of syndromes and other general diagnoses, dental caries prevalence, and how caries was assessed.
Dental caries prevalence was extracted in accordance with WHO criteria [Citation12]. Significant caries index value (Sic; calculated as the mean of DMFT or dmft scores of the highest one-third of all the participants) was also recorded. Proportion of subjects with DMFT > 0 or dmft > 0 was also registered. Level of significance was set at p < .05 in the original references.
Methodological quality
Assessment of the quality of the studies was done separately by the investigators (EK and MB) using a modified Newcastle-Ottawa scale for cross-sectional studies. The original scale was designed for assessing quality of nonrandomized studies [Citation13]. Disagreement between investigators was solved by discussion. Three quality categories were assessed separately: 1) selection (four items), 2) comparability (one item), and 3) outcome (three items). Each item generated 0 (not performed or inadequate) to 1 (adequate) score, except for comparability that generated 0 to 2. A total score (range 0–9) was calculated by adding the scores of the different items.
The items of the modified Newcastle-Ottawa scale are described in detail in . The items ‘sample size’ and ‘calibration’ were modified from the original scale. The requirements for scoring in the second item ‘comparison group’ was a comparison group of healthy children without evidence of chronic disease or long term medication obtained from a) the same community as the children with CHD (i.e. community controls), or b) children referred to the same hospital as the CHD group for investigation of suspected CHD, but who did not fulfil diagnosis of CHD (i.e. hospital controls).
Table 1. Quality of the studies included in the systematic review on caries in children with congenital heart disease (CHD) according to the modified Newcastle-Ottawa scale.
The comparability category assessed whether exposed and non-exposed individuals were matched in the design and/or confounders were adjusted for in the analysis. For the ‘Follow-up’ item majority of patients had to be at least 3 years of age, as caries progression into the dentine requires time.
Results
Study selection
The identification and selection process of the studies is described in a PRISMA Flow Diagram [Citation14] in . The primary search resulted in 149 publications, from which eight publications were selected and supplemented with one article from reference lists of selected publications. In total, nine studies were included in the systematic review.
Study outcome
Dental caries prevalence in children with CHD and healthy children is summarized in . The caries prevalence was higher in children with CHD compared with healthy children in seven out of nine studies, although the difference was statistically significant (p < .05) in only three [Citation15–17]. For primary dentition, dmft was 2.8 in children with CHD compared with 1.4 for healthy children [Citation16], and dmfs was 4.7 compared with 2.1 for healthy children [Citation17]. For primary dentition 77,4% of CHD and 56,5% of healthy children, were not caries free (dmft > 0), and the SiC value was 8.2 in children with CHD compared with 5.9 for healthy children [Citation15]. For permanent dentition, DMFT was 2.0 in children with CHD compared with 1.1 in healthy children in one study [Citation16], and 1.3 compared to 0.6 in another [Citation15]. For permanent teeth 53,1% of CHD and 34,6% of healthy children, were not caries free (DMFT > 0), and the SiC value was 1.8 in CHD group compared to 0.8 in the healthy children [Citation15]. Lower caries prevalence in children with CHD, compared with healthy children, was also reported, yet the differences were not statistically significant [Citation18,Citation19]. The children with significantly higher caries prevalence, suffered from CHD, severity grades 2–4 in two studies [Citation16,Citation17] and severity grades 2 and 3 in one study [Citation15].
Table 2. Age, sample size, meth of caries assessment, and dental caries prevalence in children with CHD compared to a healthy control group.
Study characteristics
describes child age, sample size, and method of dental caries assessment. Study subjects were less than 16 years of age with the youngest children reported to be one year of age. Mean age in the study groups ranged from 2.7 (1.4) to 10 (1.3) years. Most studies included less than 100 CHD patients. Less than 30 CHD patients were included in two studies [Citation20,Citation21], and the largest study sample included 165 CHD patients. The number of children with primary or permanent dentition was outlined in four of the studies [Citation15,Citation18,Citation22,Citation23].
summarizes the study characteristics in relation to publication year, geography, study design, CHD type and severity, patient syndromes and other diagnoses. Studies were published between 2004 and 2018. The geographical distribution of the studies was wide and included three from the Middle East (Iran and Turkey) [Citation16,Citation22,Citation24], three from Europe (Germany, Sweden and UK) [Citation17,Citation21,Citation23], one from Africa (Sudan) [Citation15], one from the USA (Ohio) [Citation19], and one from India [Citation18]. Most of the CHD and healthy children were recruited from a tertiary care setting (e.g. University hospital) [Citation15,Citation16,Citation18–24]. The study design was cross-sectional in all studies.
Table 3. Publication year, geography, study design, CHD severity and type, syndromes and other diagnoses of the studies included in the analysis.
The descriptions of the CHD type differed between studies, and the severity of the heart defects in the studies varied, as shown in . Most of the studies included a variety of CHD severity. Seven out of nine studies included children with complex CHD grades 3 or 4, and five studies included children with the most severe heart defects (grade 4). Two studies [Citation15,Citation18] included CHD severity grade 2 and 3 only, and, thus, a limited number of children at risk for infective endocarditis. CHD types were not outlined in two studies [Citation19,Citation22]. One study also included children with rheumatic heart disease (RHD) [Citation18]. One study included children with heart transplants (HTx) [Citation21], these children were presented as a separate group and compared with CHD and controls.
Children with syndromes or other diseases were excluded in most studies [Citation16,Citation17,Citation19,Citation22,Citation23]. Only one study [Citation15] included children with Noonan, Marfan and Down syndromes but the number of patients with syndromes or type of CHD in these children were not described. Three studies [Citation18,Citation21,Citation24] did not include information on syndromes or other comorbidities.
Background information on the comparison group was limited in most studies. Three studies [Citation15,Citation21,Citation22] reported that children in the healthy control group were free from cardiac conditions, and another four studies [Citation17–19,Citation24] reported, with no additional information, that the control group consisted of healthy children. One study [Citation16] excluded control children who had received active orthodontic therapy or had any systemic disease. In one study [Citation23] the control group included healthy children with normal hearts followed up due to heart disease in the family (e.g. cardiomyopathy).
Study quality assessment
The quality scores of the studies ranged from 4 to 9 points, as assessed according to the modified Newcastle-Ottawa Scale (). In three [Citation18,Citation19,Citation24] studies, the selection of the healthy children was insufficiently described with information on the selection process or background population lacking. Power analysis was performed in only one study [Citation15]. Differences in age between the groups were evaluated in six [Citation16,Citation17,Citation22–25] out of nine studies with no significant differences reported.
SES was evaluated in four [Citation15,Citation21,Citation23,Citation24] studies included in this systematic review, and there were no differences reported between the groups. Only one study outlined the distribution of SES variables (mother’s educational level, marital status, occupation and size of home reported as numbers of rooms) between the groups [Citation15]. There were no differences between the study groups reported, but both groups were from represented low income areas. One of the studies [Citation23] mentioned recording SES with the Townsend deprivation index, but SES results were not presented. Another study [Citation24] reported collecting demographic data, but SES variables were not included in the assessment. Furthermore, one study [Citation21] reported SES by stating that all participants came from Germany with a similar family background.
Caries data were collected by clinical examination in seven [Citation15,Citation18,Citation19,Citation21–24] out of nine studies. One of these studies reported that bite-wing radiographs were evaluated in addition to the dental examination [Citation22]. Furthermore, two studies assessed caries retrospectively from previously collected dental and radiographical records [Citation16,Citation17]. All studies assessed caries using WHO diagnostic criteria [Citation12].
One study [Citation15] included information on standardization of outcome assessments with two calibrated dentists performing the clinical examinations, and another study [Citation23] reported that training of the investigator was supervised by a dentist investigator with documented expertise.
Discussion
The aim of this systematic review was to summarize the current literature on caries prevalence among children with CHD in comparison with healthy peers. Overall, this systematic review indicates a higher caries prevalence among CHD children compared with healthy children. In particular, operated and complex CHD children seem to experience higher caries prevalence than healthy children.
Two studies [Citation16,Citation17] reported significantly higher caries prevalence in the primary dentition among children with CHD. Caries during early life commonly involves procedures performed under general anaesthesia that is considered a risk procedure in children with complex CHD (grade 3–4), and therefore the treatment is performed in tertiary care settings only. Poor oral health with high dental treatment needs may necessitate repeat dental procedures delaying invasive cardiac interventions and potentially leading to dental anxiety as well. Furthermore, longitudinal studies in healthy children show that caries experience in primary dentition increases the risk of caries development in the permanent dentition [Citation26]. With early effective caries prevention, these high risk dental procedures could potentially be avoided among children with CHD.
Dental caries is a multi-factorial disease process. Only a few of the included studies investigated factors that might explain the higher caries prevalence in CHD children. Although studies were performed in different countries with a variance in preventive dental health care, significantly higher caries prevalence was observed compared with healthy children in the same population [Citation15–17]. Furthermore, no difference in SES between CHD and healthy children was reported in the studies included. Altogether, this suggests that the higher caries prevalence in CHD children compared with healthy children is not mediated by a difference in SES or the level of dental health care service.
Children with complex CHD commonly have a higher disease burden including feeding difficulties, needs of longer periods of medication, and repeated cardiac interventions with prolonged in-hospital care during childhood. High CHD disease burden may increase the risk of neglected oral health care routines and lower the attention on caries prevention in the family. Low priority may also lead to cancellations of preventive oral health care contacts commonly offered to healthy children.
According to this systematic review, children with operated and complex CHD seem to experience a higher caries prevalence than healthy children. However, many of the studies included mild to complex CHD severity grades combined in the comparison of healthy children. Mild CHD forms may have diluted the CHD sample and low the number of complex CHD precluded an assessment of caries prevalence in relation to CHD severity. In addition, sample size calculations and power analyses were rarely performed. Thus, studying dental caries prevalence in a larger sample and including more children with complex CHD (i.e. at risk of developing bacterial endocarditis) is needed to address these aspects in more detail.
The selection and comparability of healthy controls was emphasized in the quality assessment process in this systematic review. In the studies included healthy controls were recruited from the same community and, displayed comparable age and SES distributions as CHD children. All these factors are essential to consider when evaluating dental caries related with CHD. Thus, this systematic review suggests limited effects of bias from these important confounders.
As caries progression into the dentine requires time, the majority of study subjects had to be at least three years of age at the time of dental examination. In most of the studies outcome measures were based on prospectively and similarly performed clinical examinations. However, two studies [Citation16,Citation17] that found a statistically higher caries prevalence in children with CHD used previously collected data with the potential influence of multiple investigators. Nonetheless, another prospective high quality study [Citation15] based on the modified Newcastle-Ottawa Scale also reported statistically higher caries prevalence in children with CHD compared with healthy children.
Another potential limitation of the included studies was the lack of information on outcome assessment (caries) standardization. Intra- and inter observer calibration and blinding of study subject characteristics during the assessment are important factors to consider in the study design in order to avoid observer bias and decrease technical variability in data collection. In this systematic review only two studies [Citation15,Citation23] addressed observer calibration.
Strengths of this study include collected information on CHD type and severity providing some insights into association between CHD severity and caries prevalence. On the other hand, the study is limited by use of only one metric of study quality (modified Newcastle-Ottawa Scale).
Conclusion
Although, evidence is limited the current literature indicates that the children with CHD experience higher caries prevalence compared with healthy controls. Future studies should focus on comparability of control groups and standardization of outcome measures in data collection.
Disclosure statement
The authors have no conflicts of interests to declare.
Additional information
Funding
References
- van der Linde D, Konings EE, Slager MA, et al. Birth prevalence of congenital heart disease worldwide: a systematic review and meta-analysis. J Am Coll Cardiol. 2011;58:2241–2247.
- Rushani D, Kaufman JS, Ionescu-Ittu R, et al. Infective endocarditis in children with congenital heart disease: cumulative incidence and predictors. Circulation. 2013;128:1412–1419.
- Wilson W, Taubert KA, Gewitz M, et al.; Quality of Care and Outcomes Research Interdisciplinary Working Group. Prevention of infective endocarditis: guidelines from the American Heart Association: a guideline from the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working Group. Circulation. 2007;116:1736–1754.
- Lockhart PB, Brennan MT, Sasser HC, et al. Bacteremia associated with toothbrushing and dental extraction. Circulation. 2008;117:3118–3125.
- Vos T, Abajobir AA, Abate KH, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet. 2017;390:1211–1259.
- Peres MA, Macpherson LMD, Weyant RJ, et al. Oral diseases: a global public health challenge. Lancet. 2019;394:249–260.
- Hallett KB, Radford DJ, Seow WK. Oral health of children with congenital cardiac diseases: a controlled study. Pediatr Dent. 1992;14:224–230.
- Tanaka K, Miyake Y, Sasaki S, et al. Infant feeding practices and risk of dental caries in Japan: the Osaka maternal and child health study. Pediatr Dent. 2013;35:267–271.
- Nederfors T. Xerostomia and hyposalivation. Adv Dent Res. 2000;14:48–56.
- da Silva DB, Souza IP, Cunha MC. Knowledge, attitudes and status of oral health in children at risk for infective endocarditis. Int J Paediatr Dent. 2002;12:124–131.
- Schardt C, Adams MB, Owens T, et al. Utilization of the PICO framework to improve searching PubMed for clinical questions. BMC Med Inform Decis Mak. 2007;7:16–16.
- World Health Organisation. Oral health surveys, basic methods. 5th ed. Geneva: World health organization; 2013.
- Orchi.ca. The Ottawa Hospital Research Institute. The Newcastle Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses; [cited 2020 Nov 2]. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
- Moher D, Shamseer L, Clarke M, et al.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1–1.
- Ali HM, Mustafa M, Hasabalrasol S, et al. Presence of plaque, gingivitis and caries in sudanese children with congenital heart defects. Clin Oral Investig. 2017;21:1299–1307.
- Cantekin K, Yilmaz Y, Cantekin I, et al. Comprehensive dental evaluation of children with congenital or acquired heart disease. Cardiol Young. 2013;23:705–710.
- Stecksen-Blicks C, Rydberg A, Nyman L, et al. Dental caries experience in children with congenital heart disease: a case-control study. Int J Paediatr Dent. 2004;14:94–100.
- Suma G, Usha MD, Ambika G, et al. Oral health status of normal children and those affiliated with cardiac diseases. J Clin Pediatr Dent. 2011;35:315–318.
- da Fonseca MA, Evans M, Teske D, et al. The impact of oral health on the quality of life of young patients with congenital cardiac disease. Cardiol Young. 2009;19:252–256.
- Ajami B, Abolfathi G, Mahmoudi E, et al. Evaluation of salivary Streptococcus mutans and dental caries in children with heart diseases. J Dent Res Dent Clin Dent Prospects. 2015;9:105–108.
- Siahi-Benlarbi R, Nies SM, Sziegoleit A, et al. Caries-, candida- and candida antigen/antibody frequency in children after heart transplantation and children with congenital heart disease. Pediatr Transplant. 2010;14:715–721.
- Cantekin K, Gumus H, Torun YA, et al. The evaluation of developmental enamel defects and dental treatment conditions in a group of turkish children with congenital heart disease. Cardiol Young. 2015;25:312–316.
- Tasioula V, Balmer R, Parsons J. Dental health and treatment in a group of children with congenital heart disease. Pediatr Dent. 2008;30:323–328.
- Pourmoghaddas Z, Meskin M, Sabri M, et al. Dental caries and gingival evaluation in children with congenital heart disease. Int J Prev Med. 2018;9:52.
- Mohamed Ali H, Berggreen E, Nguyen D, et al. Dental plaque microbial profiles of children from khartoum, sudan, with congenital heart defects. J Oral Microbiol. 2017;9:1281556.
- Skeie MS, Raadal M, Strand GV, et al. The relationship between caries in the primary dentition at 5 years of age and permanent dentition at 10 years of age - a longitudinal study. Int J Paediatr Dent. 2006;16:152–160.