Abstract
Objective
To examine the prevalence of sagittal relationships, asymmetries and midline shift, and their associations with temporomandibular disorders (TMD) in the Northern Finland Birth Cohort 1966 (NFBC1966).
Materials and methods
1845 subjects participated in a clinical examination at the age of 46. Occlusal measurements were performed using 3D models. Symptoms of TMD were screened using validated questions, and signs and diagnoses of TMD were assessed using a modified protocol of the Diagnostic Criteria for TMD (DC/TMD) and questionnaires. Associations between variables of occlusion and TMD were evaluated with χ2-test and Fisher's exact test and using logistic regression analyses, adjusted for self-reported general health, mental health, bruxism, and rheumatoid arthritis.
Results
The most common sagittal relationships were Class I and normal canine relationship. Half-cusp Class II and post-normal canine relationship were more frequent in females, and Class III and pre-normal canine relationship in males. Deviations from normal cuspid or molar relationships showed a weak but statistically significant association with TMD, especially in females. Half-cusp Class II and Class II relationships were more frequent in relation to joint-related TMD signs and diagnoses while missing canines were associated with pain-related TMD diagnoses.
Conclusions
The present study findings gave some indications that canine relationships are associated with pain-related TMD, whereas Angle II sagittal occlusal relations may associate with joint-related TMD. Occlusal characteristics should therefore be taken into account as one possible associating factor in subjects with TMD.
Introduction
Sagittal deviations from normal occlusion are common at the population level [Citation1]. Based on Angle’s classification, Class I is the normal molar relationship, and its prevalence on a population level is 64.5–71.2% [Citation2,Citation3]. Earlier studies among Caucasian adults have shown that in sagittal malocclusions, Class II is more prevalent (15–27.8%) compared to Class III (4.6–7.6%) [Citation2–4]. In addition to Angle classification, the canine relationship is an essential feature in the registration of sagittal deviations. The canine relationship has been considered clinically important, especially for occlusal function by canine guidance [Citation5–7], although its significance has not previously been widely studied.
The major indications for orthodontic treatment are improvement in occlusal function and aesthetics, and the demand for orthodontic treatment is high [Citation1,Citation8–10]. Functional aspects include pain symptoms and temporomandibular disorders (TMD), although the significance of occlusion in TMD is still in debate [Citation11–16].
The term TMD includes all pain and functional disturbances of the masticatory system, i.e. masticatory muscles, temporomandibular joints (TMJs), and associated structures [Citation17]. The aetiology of TMD is multifactorial and it can be influenced by occlusal characteristics, trauma, emotional stress, deep pain input, biopsychosocial and genetic factors, or parafunctions [Citation17]. Earlier studies have found associations between TMD and poor self-reported general health, psychosocial symptoms, general diseases (such as rheumatoid diseases), and bruxism [Citation18–24].
Most of the earlier studies have provided weak or no evidence for the occlusal aetiology of TMD [Citation11,Citation12,Citation15]. However, some studies have found a statistically significant association between unstable occlusion and TMD [Citation13,Citation14,Citation16]. Also, asymmetry of sagittal molar relationships and dental midline shift have been reported to associate with TMD [Citation25], and canine asymmetry and dental midline shift with facial pain or TMJ arthrosis [Citation26,Citation27]. However, the association between TMD and dental occlusion is still controversial at the population level, and there is a gap of knowledge in the literature of the potential role of malocclusion in the onset of TMD.
The aim of this study was to examine the prevalence of sagittal occlusal relationships of the first permanent molars and canines, their asymmetries and dental midline shift, and to study their association with the symptoms, signs, and diagnoses of TMD while taking into account confounding factors in middle-aged Finnish adult population. The hypotheses were that (1) Class II molar/post-normal canine relationships are the most common sagittal deviations, and (2) molar and canine relationships, asymmetries, and midline shifts are associated with TMD.
Materials and methods
Subjects
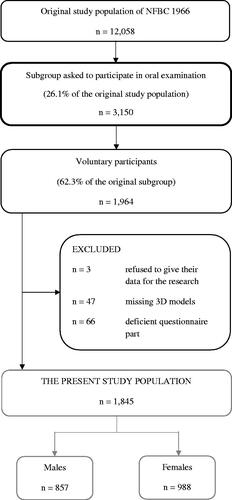
The study is part of the Northern Finland Birth Cohort 1966 (NFBC1966) (https://www.oulu.fi/nfbc/node/19663), which is an epidemiological and longitudinal research program aiming to promote the health and well-being of the population in Northern Finland [Citation28]. The NFBC1966 originally comprised all live births in 1966 (n = 12,058) in the former provinces of Oulu and Lapland in Finland. A subgroup of 3150 persons currently living in the Oulu region (range 100 km) was asked to attend a clinical oral and dental examination in the years 2012–2013 when the subjects were 46 years old; of those invited, 1964 persons (62.3%, 912 males, 1052 females) volunteered to participate. The clinical oral and dental health examination included digital 3D dental models, and a questionnaire on subjects’ background information, lifestyle, and health. The subjects signed an informed consent form on their own behalf. Three subjects refused to give their data for the study. The final study population was 1845 subjects after two other exclusion criteria: (1) missing three-dimensional (3D) models and (2) deficient questionnaire part. The flow chart of the final study population is presented in . The research program coordinated by the Department of Health Sciences, Faculty of Medicine, University of Oulu [Citation28], and the data collection in 2012–2013 has been approved by the ethical committee of the Northern Ostrobothnia Hospital District (74/2011).
3D occlusal measurements
The dental arches were digitized by using an iTero 3D scanner (Cadent, San Jose, CA, USA). Digital measurements in sagittal and occlusal view planes were carried out with Ortho Analyzer™ software (3Shape, Copenhagen, Denmark).
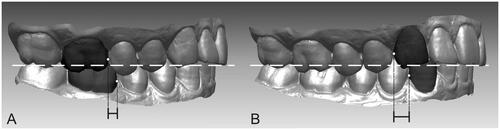
The inter-arch digital measurements of 3D models contained the bilateral first molar and canine relationships and were conducted by the method described by Pirttiniemi et al. [Citation29]. The first molar and canine relationships were divided into four categories: Class I, half-cusp Class II, Class II, and Class III. To assess the sagittal relationships, the most mesial points of the upper and lower first molars, and the most distal points of the upper and lower canines were determined (). When a missing tooth was replaced with an implant or pontic in a fixed dental prosthesis, it was handled as own tooth. The midline shift was registered by two calibrated examiners (L.N. and A-S.S.) according to the midline component of the Peer Assessment Rating (PAR) index dividing midline shift into three categories: 0 = Coincident and up to ¼ width of the lower incisor, 1 = ¼–½ width of the lower incisor, 2 = >½ width of the lower incisor [Citation30].
Figure 2. Measurements of the bilateral first molar (A) and canine (B) in the sagittal view were performed by defining the most mesial points of the upper and lower first molars (A) and the most distal points of the upper and lower canines (B).
Missing teeth were also registered from 3D models. Dental arches with one or more missing teeth from 1st molar to 1st molar (other than 1st molars) in either upper or lower arch were defined as ‘dental arches with missing teeth’. In addition, missing 1st molars and canines were registered and observed separately in the analysis.
The intra-examiner error was measured from 20 randomly selected 3D models before actual measurements. The repeated measurements in 3D models were compared using intra-class correlation. The correlation ranged from 0.885 to 0.922 and was found to be at a good level.
Questionnaires
The questions concerning TMD symptoms included two questions, which are valid in screening TMD pain [Citation31].
Do you have pain in your temples, temporomandibular joints, face, or jaw? (Answer options were: no/once a week/more often; dichotomized as no pain/pain)
Do you have pain when you open your mouth wide or chew? (Answer options were: no/once a week/more often; dichotomized as no pain/pain)
The subjects were asked further questions associated with TMD which were used in the modified DC/TMD diagnostics protocol [Citation32]. Details of the questions related to TMD are also presented in Jussila et al. [Citation33].
During the prior 30 days, have you felt pain that was modified by jaw movement, function, parafunction, or being at rest? (With options: no/yes)
Have you had jaw locking in the closed position that restricted maximum mouth opening? (With options: no/yes)
Did this restricted opening cause difficulty in mastication? (With options: no/yes)
Have you had clicking noises in the TMJ during opening or closing jaw movements or during mastication? (With options: no/yes)
Have you had crepitation in the TMJ during opening or closing jaw movements or during mastication? (With options: no/yes)
The questionnaire also contained questions concerning orthodontic treatment history before or after the age of 20. Answers were dichotomized as no orthodontic treatment/orthodontic treatment history.
In addition, these questions were used to analyze the selected confounding factors in the present study:
self-reported general health (Answer options were: very good/good/fair/poor/very poor; dichotomized as good/poor)
diagnosed mental health including mental disorder and/or psychosis and/or depression and/or other mental-related problem (With options: no/yes)
self-reported bruxism including awake and/or sleep bruxism (With options: no/yes)
diagnosed rheumatoid arthritis (With options: no/yes)
Clinical examination of TMD
Six calibrated dentists carried out the clinical oral and dental health examination at the Institute of Dentistry of the University of Oulu. Both before and during the study, all examiners were trained and calibrated to ensure the repeatability of the examination, intra- and inter-examiner agreements presented by Krooks et al. [Citation9]. The details of the clinical stomatognathic examination and TMD diagnoses were based on the modified DC/TMD diagnostics protocol (DC/TMD) [Citation32] as presented by Jussila et al. [Citation33].
Statistical analysis
Statistical analyses were conducted using IBM SPSS Statistics 25.0. Comparisons between occlusal characteristics and gender, orthodontic treatment history, and full dental arches/dental arches with missing teeth, as well as comparisons between occlusal characteristics and TMD were performed with cross-tabulation: Pearson’s Chi-square test (χ2-test) and Fisher's exact test, if over 20% of the cells had an expected count of less than five. Using logistic regression analyses, the associations of outcome variables (symptoms, signs, and diagnoses of TMD) with explanatory variables (occlusion, self-reported general health, mental health, bruxism, and rheumatoid arthritis) were evaluated for the associations showing statistical significance in the pairwise analyses. Models of TMD symptoms and signs were conducted among all participants and were also adjusted with gender. Class I was used as a reference when the bilateral molar relationship was analyzed as an explanatory variable. A value of p < .05 was accepted as statistically significant.
Results
Sagittal occlusal relationships
shows that the most common sagittal relationship in molars was Class I occlusion on both sides (63.4% right, 69.1% left) followed by Class II, half-cusp Class II, and Class III. In canine relationships, the order from the most common to the least common was normal (64.3% right, 68.2% left), cusp-to-cusp, post-normal, and pre-normal relationship. The distribution of different molar and canine relationships differed between genders. Females had more distal (Class II, half-cusp Class II, and post-normal) relationships compared to males, while mesial (Class III and pre-normal) relationships were more common in males than females (p < .05).
Table 1. Distributions [n (%)] of molar and canine relationships, asymmetries and midline shift according to gender (χ²-test).
Asymmetries were common in both molar and canine relationships (31.6, 42.2%, respectively). No gender difference in asymmetries was found. However, in midline shift scores, there was a statistically significant difference between genders, with males having a higher prevalence of midline shifts than females (p = .009) (). The differences in measured occlusal characteristics were not statistically significant between subjects with and without orthodontic treatment history.
In bilateral molar relationships, Class II and Class III molar occlusions were significantly more common in dental arches with missing teeth than in full dental arches (p < .001). Asymmetries in molar and canine relationships were more frequent in dental arches with missing teeth (p = .046, p < .001, respectively), and a higher prevalence of midline shift was found as well (p < .001) ().
Table 2. Distributions [n (%)] of molar and canine relationships, asymmetries and midline shift according to ‘Full dental arches’ and ‘Dental arches with missing teeth’ (χ²-test).
Occlusal characteristics in relation to TMD
presents the associations of the measured occlusal characteristics with self-reported pain symptoms. Canine relationship and canine asymmetry were associated with pain in temples, TMJs, face, or jaw; those who reported pain had more often cusp-to-cusp relationship and/or symmetric canine relationship (p = .015, p = .039, respectively). Based on the multivariable model (), the association between canine asymmetry and pain in temples, TMJs, face, or jaw after was still statistically significant (p = .041), but there was no significant association between bilateral canine relationship and self-reported pain symptoms.
Table 3. Frequencies [n (%)] of TMD symptoms and signs in the following occlusal groups: molar and canine relationships, asymmetries and midline shift (χ²-test).
Table 5. Frequencies [n (%)] of diagnosed TMD in the following occlusion groups: molar and canine relationships, asymmetries, midline shift and missing first molars or canines for genders separately (χ²-test).
In addition, summarizes the associations of the measured occlusal characteristics with signs of TMD. Limited mouth opening was more frequent in subjects with asymmetry in canine relationships compared to those with symmetric relationships (p = .040, and in the multivariable model p = .060). There was a statistically significant difference in crepitus in TMJs between groups of different molar relationships, crepitus being most frequent in the half-cusp Class II group (p = .020), and in the multivariable model, half-cusp Class II was still significantly associated with crepitus in TMJs (p = .024) ().
Table 4. Logistic regression analysis for TMD symptom (pain in temples, temporomandibular joints, face, or jaw) and signs (limited mouth opening and crepitus in TMJs).
The distributions of the measured occlusal characteristics and their associations with TMD diagnoses are shown in . Half-cusp Class II was found to be the most frequent bilateral molar relationship in females with disc displacement with reduction and degenerative joint disease (15.8%, p = .043 and 26.3%, p < .001, respectively). Based on the multivariable models (), the bilateral molar relationship was statistically significantly associated with disc displacement with reduction and degenerative joint disease (p = .034, p < .001, respectively).
Table 6. Logistic regression analysis for TMD diagnoses among women.
Considering the association between missing first molars or canines and TMD diagnoses, females with one or more missing canines had significantly more often myalgia and arthralgia as compared to females with no missing canines (p = .014, p = .022 and in the multivariable model p = .002, p = .004, respectively). In men, such associations were not found ().
Of the confounding factors (), self-reported general health had a statistically significant association with pain symptoms, limited mouth opening, myalgia, and arthralgia (p < .001, p = .047, p = .001, p < .001, respectively). Mental health was associated with arthralgia (p = .049), rheumatoid arthritis with crepitus in TMJs, arthralgia (p = .002, p = .018), and gender with TMD symptoms and signs (p < .001, p = .004, p = .024).
Discussion
In the present study sample consisting of 46-year-old cohort subjects, the prevalence of sagittal occlusal relationships, asymmetries and midline shift, and their association with TMD were studied. Class I molar relationship and normal canine relationship were the most common sagittal relationships both in males and females, but distributions of the sagittal deviations differed between genders. An association between TMD and some occlusal characteristics was found, especially with missing canines and deviations of normal molar relationship. In addition, statistically significant gender differences in these associations were revealed.
As TMD has a multifactorial background, associations of occlusal characteristics with TMD were adjusted with the potential confounders, which were selected based on the previous findings in the same study population [Citation22,Citation24]. Nevertheless, most of the analyzed associations remained statistically significant in the multivariable models in this study. It is noteworthy, however, that among selected confounders, especially self-reported general health was also strongly associated with pain-related TMD.
Sagittal occlusal relationships
Most of the previous studies among Caucasian adults have found that the Class I molar relationship has the highest prevalence, followed by Class II [Citation2–4,Citation34], and the findings of the present study were in agreement with these studies. The results showed that half-cusp Class II and cusp-to-cusp relationships were more prevalent in females, while Class III and pre-normal canine relationships were significantly more frequent in males. This is in accordance with previous studies that have also found that males have Class III more often compared to females [Citation2,Citation3,Citation34].
Occlusal characteristics in relation to TMD
The results of this study showed that half-cusp Class II and Class II seem to be more frequent in adults with TMD than Class III. Sagittal malocclusions have previously been found to relate to TMJ changes, especially in Class II vertical cases [Citation35], and in Class II and Class III discrepancies [Citation36]. Paunonen et al. [Citation37] reported that Class II malocclusion and retrognathic mandible were associated with pain-related TMD diagnoses. It has also been found that Class II malocclusion is associated with the altered position of the condyle in the mandibular fossa [Citation38]. Furthermore, the distal position of the mandible may expose especially to disc displacement [Citation35].
In the present study, especially the half-cusp Class II relationship stood out in association with disc displacement with reduction and degenerative joint disease. The association of bilateral molar relationships with these TMD diagnoses was seen especially in females. The female gender has generally been associated with destructive processes and derangements of TMJ [Citation39–42]. However, among men, the sample size of TMD diagnoses was small in the present study and thus, the lack of association between measured occlusal characteristics and TMD diagnoses cannot be confirmed.
Although the cusp-to-cusp molar relationship is a normal occlusal feature in the primary dentition, in the permanent dentition half-cusp Class II relationship seems to be unstable due to deficient intercuspidation. Unstable occlusion may lead to increased slide from centric relation to intercuspal position, which has been found to associate with symptoms and signs of TMD [Citation16,Citation43]. However, it has also been suggested that since Class I has the highest prevalence also in TMD, dental sagittal malocclusions should not be considered as a predictor of TMD [Citation44].
Asymmetry in relation to TMD
In the present study, symptoms of TMD were assessed based on two questions published by Nilsson et al. [Citation31] to screen for self-reported TMD pain. Earlier, Sipilä et al. [Citation26] examined a subsample of the NFBC1966 when the subjects were at the age of 31 years and found that sagittal canine relationship was associated with facial pain and pain on palpation in the masticatory muscles. Interestingly, in this study, those with a symmetric canine relationship reported more pain symptoms than subjects having asymmetry. The explanation for this may be that in an asymmetric sagittal relationship one side is possible in normal cuspidation. It should also be noted that the measurements of the present study were conducted in stable occlusion, and therefore, only static asymmetry. Earlier studies have shown that occlusal and dentofacial asymmetry are associated with TMD [Citation13,Citation45]. It has also been shown that subjects with lateral malocclusions had more often asymmetric positions of the condyles [Citation29].
Missing teeth in relation to TMD
Missing posterior teeth have previously been found to associate with disc displacement [Citation46] and enlarge the risk of TMD especially in young females [Citation47]. In the present study, a statistically significant association was only found between missing canines and myalgia and arthralgia among females. It should be noted, however, that the number of subjects with missing canines (n = 4) was small. Findings of the present study indicate that missing canines are more associated with pain-related TMD, which supports the importance of effective canine guidance. This is also supported by previous findings suggesting that electromyographic (EMG) activity is significantly lower with canine guidance than with group function [Citation5–7]. In addition, the absence of lateral canine guidance has been reported to be a risk factor for TMD and altered muscle activities [Citation43,Citation48].
Strengths and limitations
The strength of the present study was a large population-based data, with all subjects born in the same year. Occlusal measurements were done using 3D models, which have shown to be precise and even more repeatable compared to manual measurements [Citation49]. In addition, half-cusp Class II and cusp-to-cusp relationships were also taken into account, in contrast to the majority of earlier studies which have only reported the prevalence of Class I, II, and III.
The present study has some limitations. Firstly, as the present study is a cross-sectional study, a cause-effect relationship between occlusion and TMD cannot be determined. A follow-up study would certainly provide more information. Secondly, as the number of subjects in distinct subgroups remained relatively low, the results of this study cannot be directly generalized to the population level. Thus, studies with larger samples are needed to increase the statistical power.
No mathematical correction was made for multiple comparisons, but if all the null hypotheses are true, 5% of the comparisons are expected to have uncorrected p-values <.05 [Citation50,Citation51]. We presented 98 p-values and expected coincidentally 5 small p-values if the null hypotheses are true. We resulted in 38 small p-values, indicating support to our study hypotheses.
Conclusion
The prevalence of sagittal relationships was in agreement with the results of earlier studies. In addition, the present study findings gave some indications that canine relationships are associated with pain-related TMD, whereas Angle II sagittal occlusal relations may associate with joint-related TMD. Occlusal characteristics should therefore be taken into account as one possible associating factor in subjects with TMD.
Acknowledgements
The authors thank the late professor Paula Rantakallio who launched NFBC1966, the participants of this study, and the work of the NFBC project centre.
Disclosure statement
The authors report no conflict of interest.
Data availability statement
NFBC data is available from the University of Oulu, Infrastructure for Population Studies. Permission to use the data can be applied for research purposes via electronic material request portal. The use of data follows the EU general data protection regulation (679/2016) and Finnish Data Protection Act. The use of personal data is based on cohort participant’s written informed consent at his/her latest follow-up study, which may cause limitations to its use. Please, contact NFBC project centre ([email protected]) and visit the cohort website (www.oulu.fi/nfbc) for more information.
Additional information
Funding
References
- Proffit WR, Fields HW Jr., Moray LJ. Prevalence of malocclusion and orthodontic treatment need in the United States: estimates from the NHANES III survey. Int J Adult Orthodon Orthognath Surg. 1998;13(2):97–106.
- Salonen L, Mohlin B, Gootzlinger B, et al. Need and demand for orthodontic treatment in an adult swedish population. Eur J Orthod. 1992;14(5):359–368.
- Jonsson T, Arnlaugsson S, Karlsson KO, et al. Orthodontic treatment experience and prevalence of malocclusion traits in an Icelandic adult population. Am J Orthod Dentofacial Orthop. 2007;131(1):8.e11–8.e18.
- Laine T, Hausen H. Occlusal anomalies in Finnish students related to age, sex, absent permanent teeth and orthodontic treatment. Eur J Orthod. 1983;5(2):125–131.
- Shupe RJ, Mohamed SE, Christensen LV, et al. Effects of occlusal guidance on jaw muscle activity. J Prosthet Dent. 1984;51(6):811–818.
- Manns A, Chan C, Miralles R. Influence of group function and canine guidance on electromyographic activity of elevator muscles. J Prosthet Dent. 1987;57(4):494–501.
- Akören AC, Karaağaçlioğlu L. Comparison of the electromyographic activity of individuals with canine guidance and group function occlusion. J Oral Rehabil. 1995;22(1):73–77.
- Josefsson E, Bjerklin K, Lindsten R. Malocclusion frequency in Swedish and immigrant adolescents – influence of origin on orthodontic treatment need. Eur J Orthod. 2007;29(1):79–87.
- Krooks L, Pirttiniemi P, Kanavakis G, et al. Prevalence of malocclusion traits and orthodontic treatment in a Finnish adult population. Acta Odontol Scand. 2016;74(5):362–367.
- Rolland SL, Treasure E, Burden DJ, et al. The orthodontic condition of children in England, Wales and Northern Ireland 2013. Br Dent J. 2016;221(7):415–419.
- Pullinger AG, Seligman DA, Gornbein JA. A multiple logistic regression analysis of the risk and relative odds of temporomandibular disorders as a function of common occlusal features. J Dent Res. 1993;72(6):968–979.
- McNamara JA, Seligman DA, Okeson JP. Occlusion, orthodontic treatment, and temporomandibular disorders: a review. J Orofac Pain. 1995;9(1):73–90.
- Raustia AM, Pirttiniemi PM, Pyhtinen J. Correlation of occlusal factors and condyle position asymmetry with signs and symptoms of temporomandibular disorders in young adults. Cranio. 1995;13(3):152–156.
- Seligman DA, Pullinger AG. Analysis of occlusal variables, dental attrition, and age for distinguishing healthy controls from female patients with intracapsular temporomandibular disorders. J Prosthet Dent. 2000;83(1):76–82.
- Manfredini D, Lombardo L, Siciliani G. Temporomandibular disorders and dental occlusion a systematic review of association studies: end of an era? J Oral Rehabil. 2017;44(11):908–923.
- Jussila P, Krooks L, Näpänkangas R, et al. The role of occlusion in temporomandibular disorders (TMD) in the Northern Finland birth cohort (NFBC) 1966. Cranio. 2019;37(4):231–237.
- Okeson JP. Management of temporomandibular disorders and occlusion. 8th ed. St Louis: Elsevier; 2019.
- Kindler S, Samietz S, Houshmand M, et al. Depressive and anxiety symptoms as risk factors for temporomandibular joint pain: a prospective cohort study in the general population. J Pain. 2012;13(12):1188–1197.
- Manfredini D, Stellini E, Marchese-Ragona R, et al. Are occlusal features associated with different temporomandibular disorder diagnoses in bruxers? Cranio. 2014;32(4):283–288.
- Kurtoglu C, Kurkcu M, Sertdemir Y, et al. Temporomandibular disorders in patients with rheumatoid arthritis: a clinical study. Niger J Clin Pract. 2016;19(6):715–720.
- Yeung E, Abou-Foul A, Matcham F, et al. Integration of mental health screening in the management of patients with temporomandibular disorders. Br J Oral Maxillofac Surg. 2017;55(6):594–599.
- Jussila P, Knuutila J, Salmela S, et al. Association of risk factors with temporomandibular disorders in the Northern Finland birth cohort 1966. Acta Odontol Scand. 2018;76(7):525–529.
- Pantoja LLQ, de Toledo IP, Pupo YM, et al. Prevalence of degenerative joint disease of the temporomandibular joint: a systematic review. Clin Oral Investig. 2019;23(5):2475–2488.
- Ekman A, Rousu J, Näpänkangas R, et al. Association of self-reported bruxism with temporomandibular disorders – Northern Finland birth cohort (NFBC) 1966 study. Cranio. 2020;3:1–6.
- Fushima K, Inui M, Sato S. Dental asymmetry in temporomandibular disorders. J Oral Rehabil. 1999;26(9):752–756.
- Sipilä K, Ensio K, Hanhela H, et al. Occlusal characteristics in subjects with facial pain compared to a pain-free control group. Cranio. 2006;24(4):245–251.
- Manfredini D, Lombardo L, Siciliani G. Dental angle class asymmetry and temporomandibular disorders. J Orofac Orthop. 2017;78(3):253–258.
- University of Oulu: Northern Finland Birth Cohort 1966. University of Oulu. Available from: http://urn.fi/urn:nbn:fi:att:bc1e5408-980e-4a62-b899-43bec3755243
- Pirttiniemi P, Raustia A, Kantomaa T, et al. Relationships of bicondylar position to occlusal asymmetry. Eur J Orthod. 1991;13(6):441–445.
- Richmond S, Shaw WC, Roberts T, et al. The PAR index (peer assessment rating): methods to determine outcome of orthodontic treatment in terms of improvement and standards. Eur J Orthod. 1992;14(3):180–187.
- Nilsson IM, List T, Drangsholt M. The reliability and validity of self-reported temporomandibular disorder pain in adolescents. J Orofac Pain. 2006;20(2):138–144.
- Schiffman ED. Algorithms for TMJ disorders. Diagnostic criteria for TMD (DC/TMD): a new version of the RDC/TMD. J Dent Res. 2010;89(Spec Iss B).
- Jussila P, Kiviahde H, Näpänkangas R, et al. Prevalence of temporomandibular disorders (TMD) in the Northern Finland birth cohort (NFBC) 1966. J Oral Facial Pain Headache. 2017;31(2):159–164.
- El-Mangoury NH, Mostafa YA. Epidemiologic panorama of dental occlusion. Angle Orthod. 1990;60(3):207–214.
- John ZAS, Shrivastav SS, Kamble R, et al. Three-dimensional comparative evaluation of articular disc position and other temporomandibular joint morphology in class II horizontal and vertical cases with class I malocclusion. Angle Orthod. 2020;90(5):707–714.
- Toll DE, Popović N, Drinkuth N. The use of MRI diagnostics in orthognathic surgery: prevalence of TMJ pathologies in angle class I, II, III patients. J Orofac Orthop. 2010;71(1):68–80.
- Paunonen J, Helminen M, Sipilä K, et al. Temporomandibular disorders in class II malocclusion patients after surgical mandibular advancement treatment as compared to non-treated patients. J Oral Rehabil. 2019;46(7):605–610.
- Lin M, Xu Y, Wu H, et al. Comparative cone-beam computed tomography evaluation of temporomandibular joint position and morphology in female patients with skeletal class II malocclusion. J Int Med Res. 2020;48(2):300060519892388.
- Stegenga B, de Bont LG, Boering G. Osteoarthrosis as the cause of craniomandibular pain and dysfunction: a unifying concept. J Oral Maxillofac Surg. 1989;47(3):249–256.
- Carlsson GE. Epidemiology and treatment need for temporomandibular disorders. J Orofac Pain. 1999;13(4):232–237.
- Manfredini D, Piccotti F, Ferronato G, et al. Age peaks of different RDC/TMD diagnoses in a patient population. J Dent. 2010;38(5):392–399.
- Li W, Cheng Y, Wei L, et al. Gender and age differences of temporomandibular joint disc perforation: a cross-sectional study in a population of patients with temporomandibular disorders. J Craniofac Surg. 2019;30(5):1497–1498.
- He S, Wang S, Song F, et al. Effect of the use of stabilization splint on masticatory muscle activities in TMD patients with centric relation-maximum intercuspation discrepancy and absence of anterior/lateral guidance. Cranio. 2019;20:1–9.
- Aboalnaga AA, Amer NM, Elnahas MO, et al. Malocclusion and temporomandibular disorders: verification of the controversy. J Oral Facial Pain Headache. 2019;39(4):440–450.
- Chung K, Richards T, Nicot R, et al. ENPP1 and ESR1 genotypes associated with subclassifications of craniofacial asymmetry and severity of temporomandibular disorders. Am J Orthod Dentofacial Orthop. 2017;152(5):631–645.
- Tallents RH, Macher DJ, Kyrkanides S, et al. Prevalence of missing posterior teeth and intraarticular temporomandibular disorders. J Prosthet Dent. 2002;87(1):45–50.
- Wang MQ, Xue F, He JJ, et al. Missing posterior teeth and risk of temporomandibular disorders. J Dent Res. 2009;88(10):942–945.
- Selaimen CM, Jeronymo JC, Brilhante DP, et al. Occlusal risk factors for temporomandibular disorders. Angle Orthod. 2007;77(3):471–477.2.0.CO;2]
- Kiviahde H, Bukovac L, Jussila P, et al. Inter-arch digital model vs. manual cast measurements: accuracy and reliability. Cranio. 2018;36(4):222–227.
- Rothman KJ. No adjustments are needed for multiple comparisons. Epidemiology. 1990;1(1):43–46.
- Saville DJ. Multiple comparison procedures: the practical solution. Am Stat. 1990;44:174–180.