Abstract
Objectives
The aim of this study was to compare periapical status transitions in teeth after post placement compared with other post-endodontic treatments in root-filled teeth.
Material and methods
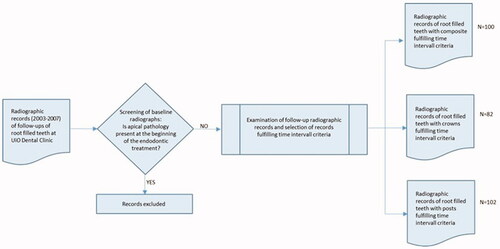
This retrospective longitudinal radiographic study included radiographs of 284 patients with root filled and restored teeth with composite fillings (Endo-fill group, n = 100), crown or fixed prosthesis (Endo-crown group, n = 82) or post and core restorations (Endo-post group, n = 102). All post and core restorations were made of gold alloy. The radiographs taken at the end of endodontic treatment, at the end of post-endodontic treatment and at least 8 months after post-endodontic treatment were evaluated. Post-operative periapical status was assessed according to the periapical index (PAI) and all teeth included in the study had no apical periodontitis preoperatively. Multi-state Markov analysis was used to assess periapical status transitions among the treatment groups.
Results
Of 284 root-filled teeth without apical periodontitis at baseline, 7.7% developed clear apical pathology within a minimum of 8 months observational period. In the Endo-post group 11 (10.78%) teeth transited from Healthy (PAI 1) to Disease (PAI 2-4) state compared with eight (9.75%) in the Endo-crown group and four (4%) in the Endo-fill group. The transition probabilities from Healthy (PAI 1) to Mild diseased (PAI 2) were 17.5% in the Endo-post group, 13.1% in the Endo-crown group and 5.3% in the Endo-fill group. Multivariate analysis showed that teeth in the Endo-fill group had 60% lower hazard to transit from Healthy (PAI 1) to Mild diseased (PAI 2) state [HR 0.40; 95% CI 0.12, 0.94]. A period exceeding 8 months between the end of the endodontic treatment and prosthetic treatment significantly increased the hazard of disease progression by three times compared with a period of ≤8 months [HR 3.16; 95% CI 1.06, 9.42].
Conclusions
Teeth without radiographic lesions at baseline and restored with posts had higher hazard to transit from healthy to diseased periapical status compared with teeth restored with composite restorations. Controlled clinical trials with longer follow-up periods are needed to validate these findings.
Introduction
It is generally accepted that the outcome of root canal treatment is positively related to the quality of endodontic treatment [Citation1,Citation2]. An effective seal provided by a good root filling will limit bacterial growth and prevent the development of periapical pathosis.
Emphasis has also been placed on coronal leakage and its effect on the prognosis of endodontic treatment. Even well-placed root fillings may show leakage in vitro [Citation3], and it has been suggested that root fillings without a coronal seal may become contaminated and that the endodontic treatment should be redone prior to placement of the definite restoration in such cases [Citation4]. However, clinical studies with histological findings have demonstrated that optimally prepared and filled root canals may resist bacterial penetration even upon long-standing oral exposure by caries, fracture or loss of restoration [Citation5].
In a study of 1010 endodontically treated teeth, Ray and Trope found that the quality of the coronal restoration had a greater impact on the periradicular status than the quality of the endodontic treatment [Citation6]. Since their study many cross-sectional studies were followed in various countries attempting to evaluate the influence of the quality of root canal fillings and coronal restorations on the periradicular status of root canal treated teeth [Citation7–12]. Those studies show variable results; some concluded that periradicular health depends equally on the quality of the root canal filling and the coronal restoration [Citation9,Citation11]; others placed more emphasis on the quality of the root canal filling [Citation2,Citation7,Citation10].
Longitudinal studies, comparing treatment outcomes of teeth restored with versus without post and core restorations are scarce. Eckerbom and co-workers investigated the prevalence of apical periodontitis after five to seven years in teeth with crowns and cast posts to evaluate if such treatment affected the apical status [Citation13]. They concluded that teeth with posts more often had apical periodontitis. Other studies compared technical and biological complication of teeth restored with versus without post and core systems over a mean observation period of four to five years [Citation14,Citation15]. It was found that teeth with posts had the same incidence of endodontic failures as teeth without posts but higher survival rates. One recent study even found that teeth with posts or screws were associated with better periapical health compared with teeth without [Citation12]. It should be noted that the cited studies are quite heterogenic: teeth were restored following different treatment protocols, and the preoperative periapical diagnosis was either unknown or not recorded.
Preparation and insertion of a post and core restoration carry an additional risk of contaminating the critical area and thus increasing the risk for occurrence of periapical lesion. To the best of the authors’ knowledge, there is a lack of longitudinal studies comparing endodontic treatment outcomes in teeth that subsequently have received post and core restorations with teeth without post and core restorations and including only teeth without periapical pathology at the outset.
The aim of this study was to investigate the periapical status transitions in teeth with posts compared with root-filled teeth without post and core restorations when all teeth included in the study at baseline had no apical pathosis.
The null hypothesis, therefore, was that there is no difference in the transition rate from healthy to diseased states in root-filled teeth restored with posts and crowns compared with root filled-teeth restored either with composite fillings or crowns without posts.
Materials and methods
Study design and participants
This retrospective longitudinal radiographic study includes radiographs of 284 patients with root filled and restored teeth (). The radiographic data were records of follow-ups of root-filled teeth retrieved from patient records at the Endodontic Department of Clinical Dentistry, University of Oslo from the period of 2003–2007. With these radiographs as a starting point, it was possible to find the type and time the restorations were placed. Data collection started and ended in 2008.
The following inclusion criteria were applied:
Absence of periapical pathosis at the start of the endodontic treatment. The indications for treatment of the teeth included were asymptomatic pulpitis, symptomatic pulpitis, pre-prosthetic endodontics, necrotic pulp without periapical lesion and prophylactic treatment without periapical lesion. Prophylactic treatment was performed on teeth scheduled for restorative treatment including posts, which were without lesions but with root fillings judged inadequate or exposed to the oral cavity and on teeth with deep fillings and questionable pulp vitality. In patients with more than one root canal treatment, one tooth for analysis was randomly selected and the other teeth excluded.
Availability of radiographs with sufficient clarity and details to evaluate the periapical status and conclude on a PAI score at the beginning of the endodontic treatment, at a minimum 8 months after the endodontic treatment and a minimum of 8 months after the end of the prosthetic treatment.
Assessment of radiographs
The periapical radiographs were taken with either a Siemens Heliodent MD (Heliodent MD; Siemens) or an Oralix AC (Oralix AC; Gendex Dental Systems) unit using the paralleling technique and Kodak Ultra Speed DF-57 (Kodak Ultra SpeedDF-57; Eastman Kodak) or Kodak Insight IP-22 (Kodak Insight IP-22; Eastman Kodak) film. Film processing was automated with Dental XR-24 Nova (Dental XR-24 Nova; Durr Dental) and XR 24 PRO (XR 24 PRO; Durr Dental). All radiographs were scanned using Epson Expression 1680 Pro scanner (Expression 1680 Pro scanner; Epson) and the images were evaluated on the computer monitor using software program Silver Fast Epson T8 (dot/inch 320 dpi Epson). When necessary, periapical radiographs were evaluated using a radiographic viewer magnification. Evaluation of the periapical area was performed using a light box and a magnifier (Mattsson; DAB Dental, Sweden) with 2× magnification. The radiographic evaluation was performed under standardized conditions, in a darkroom without daylight.
The periapical status was assessed radiographically using the periapical index (PAI) system [Citation16,Citation17]. One observer (MKH) examined all the radiographs. The observer was calibrated against a standard of 100 reference radiographs that were provided and pre scored by the developers of the index. An intra- and inter Cohen’s Kappa of 0.79 and 0.73 was obtained, ensuring satisfactory calibration.
Each tooth was evaluated at the time of diagnosis to determine inclusion, at the time of endodontic treatment (PAI baseline) and at the time of the follow-up examination at a minimum of 8 months after the endodontic treatment and at minimum of 8 months after the end of the prosthetic treatment. (PAI end). Within multi-rooted teeth, the most diseased root identified the respective score.
Treatment protocols
All the patients included in this study had been treated by undergraduate or postgraduate students. The endodontic and prosthetic treatment was rendered under controlled and standardized conditions and under the supervision of the attending faculty member to ensure quality and consistency of treatment.
Endodontic treatment
The root fillings were judged as adequate when ending 0–2 mm from the radiographic apex and had no visible voids. In addition, it was mandatory for the root canal treatment to be approved that four periapical radiographs were documented at specific times during the treatment. These were: preoperative diagnostic, working length, masterpoint, and postoperative final radiographs.
The endodontic treatment was done aseptically under a rubber dam disinfected with chlorhexidine 5 mg/ml in 70% ethanol for 1 min. The endodontic treatment included chemical irrigation with 1% NaOCl and 15% EDTA and mechanical instrumentation with stainless steel and nickel-titanium files (Maillefer, Switzerland). Roots with necrotic pulps were always treated in two or several appointments with a dressing of calcium hydroxide in sterile water and a seal of IRM (Intermediate Restorative Material; Dentsply). The filling technique included gutta-percha points (De Trey; Dentsply) and a root canal sealer (AH Plus; Dentsply) using lateral condensation. On completion, the canal orifices and access cavity were filled with IRM.
Postgraduate students had at the time the possibility to use nickel-titanium rotating file systems (Quantec, Kerr; Race, FKG; Protaper, Maillefer).
Prosthetic treatment
Root filled teeth were restored by a post and core restoration when the loss of structural integrity resulted in insufficient hard tissue support for a permanent coronal restoration. Irrespective of post placement, a minimum of 2 mm of coronal dentine was required for the preparation of a ferrule. The length of the post should be equal to the clinical length of the crown, and at least 3 mm well-condensed root filling should remain apical to the post preparation. All posts and cores in this study were custom cast posts made from gold alloy. Preparation for the post was made with the Parapost system (Parapost XP; Coltene Whaledent). Between post and core preparation and cementation, the post space was filled with calcium hydroxide paste and the coronal cavity sealed with IRM. Polyether impression material (Permadyne, Impregum Penta; 3M) was used. When possible, and especially in the front region, interim prostheses were made using prefabricated metal posts (Parapost XP; Whaledent), celluloid or polycarbonate crown forms and resin. Temporary restorations were cemented med zinc-oxide-eugenol cement (Temp Bond; Kerr or Nobetec; Directa). Prior to permanent cementation, the marginal and internal adaptation of the post and core restoration were controlled radiographically and clinically (Fit Checker; GC was regularly used). All posts were cemented with zinc-phosphate cement (De Trey Zinc Phosphate Cement; Dentsply)
Teeth with post-core restorations are referred to as the ‘Endo-post’ group.
Teeth restored with crowns or fixed dental prostheses constituted the ‘Endo-crown’ group. All crowns and fixed dental prostheses included in this study were metal ceramic crowns made of cast gold alloys. The final impression material was polyether (Permadyne, Impregum Penta; 3M) combined with retraction cord. The entrance of the root canals was usually covered with IRM (Intermediate Restorative Material; Dentsply) and the cavity was filled with composite or glass-ionomer cement. Temporary restorations used were made in dimethylmethacrylate (Luxatemp Automix; DMG) or bismethylene-bismethacrylate (Protemp; Espe) using prefabricated celluloid, polycarbonate crown forms or alginate impressions taken before preparation procedures. Marginal adaptation of the crowns and fixed partial prostheses was verified both clinically and radiographically before final cementation.
Teeth that were restored with a coronal filling constituted the ‘Endo-filling’ group. All fillings were composite fillings (Filtek Supreme XTE; 3M), (Filtek Z250; 3M), (Tetric Ceram; Ivoclean Vivadent). The coronal entrance of the root canals was covered with either IRM or glass ionomer cement (Fuji II LC Caps; GC), (Fuji IX GP Caps; GC). For the composite fillings, adhesive protocol was followed using acid etching with 37% phosphoric acid (Total etch; Ivoclean Vivadent) and adhesive (Adper Scotchbond 1 XT; 3M).
Ethical considerations
Ethical acceptance was obtained from the Norwegian Centre for Research Data (NSD reference 18108 2008) and from the Regional Committees for Medical and Health Research Ethics (REC reference 64996 2021).
Statistical methods
A tooth was classified as either healthy or diseased based on its PAI score. Two separate outcome models with different cut-off points were considered:
Model 1. PAI 1 and PAI 2 combined were defined as healthy versus PAI 3 and PAI 4 combined as disease.
Model 2. PAI 1 considered as healthy, versus PAI 2 defined as mild diseased versus PAI 3 and PAI 4 combined as diseased.
In both models, PAI 1 was defined as a healthy state, whereas PAI 2 was considered a healthy state in Model 1 but a mild disease state in Model 2. Using these disease classifications, the following transitions were allowed:
A healthy tooth can deteriorate into the diseased state (Models 1 and 2 in and , respectively).
A healthy tooth can advance into a mild disease state or recover from it (Model 2).
A tooth in the mild state can advance into a diseased state (Model 2).
A tooth in the mild state can recover and move into the health state (Model 2).
Figure 2. Two-state Markov model with a transition table showing disease progression from a healthy state (Model 1). Twenty-two teeth transited from healthy state into the diseased state and the rest remained disease free. Since the diseased state is an absorption state, transitions out of the disease state into the healthy state (recovery) are not possible.
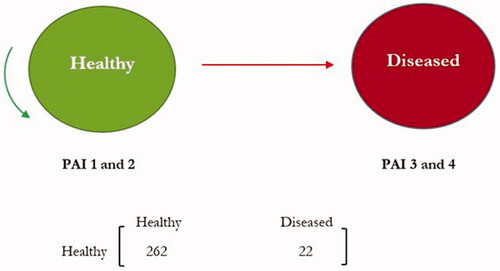
Figure 3. Three-state Markov model with a transition table showing disease progression from a healthy state and recovery from a mild state into a healthy state (Model 2). Twenty-one teeth were mildly diseased after one year, two were diseased and four recovered from the mild state.
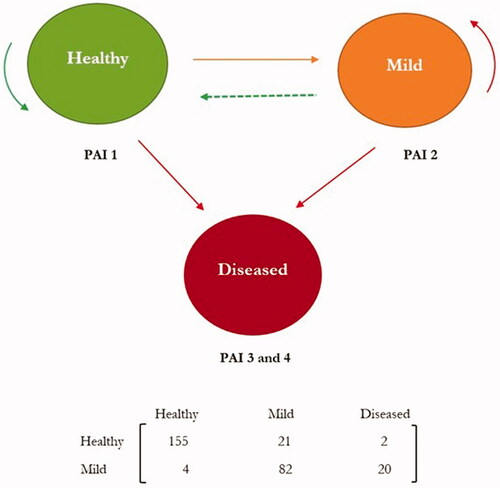
In reality, progression from the healthy state into the diseased state is probably through the mild disease state. However, this transition step cannot be observed since the assessment of patients is done at just one point in time. All the disease transitions allowed are represented in and for the two separate disease transition models respectively.
Multi-state Markov models
Multi-state Markov models were used to assess rates of disease progression in the form of transitions between different stages of periapical health states. In both Model 1 and Model 2, the diseased state was considered an absorption (end) state because there were no transitions out of this disease state. First, multi-state Markov models allowed for estimations of transition probabilities were obtained, which explained the probability of a tooth moving from one disease state into another disease state. Secondly, using a proportional intensity Markov model, we estimated the effects of treatment and other covariates on the transition intensities and obtained estimates of hazard ratios. However, because of very few transitions between disease states, we did not run the proportional intensity Markov models for the subgroups. All analyses were performed using the msm package (Jackson CH, 2011) in R (R Core Team, 2013, Vienna, Austria). The statistical significance level for all tests was set at α = 0.05. Hazard ratios are presented with their 95% confidence intervals (CI).
Results
A total of 284 teeth were included in the current study with 100 (35.2%) in the Endo-fill group, 82 (28.9%) in the Endo-crown group and 102 (35.9%) in the Endo-post group ().
Table 1. Distribution of patient factors by treatment group in the study sample.
Among the 20–40 and 41–60 age groups, the majority (47.8% and 35.8%, respectively) were in the Endo-fill group. Half of the patients above 60 years received Endo-post. The majority of the front teeth and premolars were treated with Endo-post, whereas the majority of the molars were treated with Endo-fill. The median observation time for teeth in the Endo-post, Endo-fill and Endo-crown groups was 12.5 months, 12 months and 11.5 months respectively.
Transition counts and probabilities
Based on Model 1, 22 (7.7%) teeth became diseased and the rest remained disease free (). The three-state disease model, Model 2, showed that 7.4% of the teeth transited from healthy state into a mild disease state, 0.7% of the teeth transited from healthy state into the disease state, 7% of the teeth transited from mild to disease state, whereas 28.9% remained in a mild disease state ().
Table 2. Counts (%) of teeth that transited between disease states and estimates of transition probabilities in each treatment group based on Model 1.
Table 3. Counts (%) of teeth that transited between disease states and estimates of transition probabilities in each treatment group based on Model 2.
The transition probabilities presented in and show a 7.5% and 11.6% chance that a tooth currently healthy will be diseased and mildly diseased after approximately one year based on the two models respectively. Model 2 also predicted an 18.6% chance of mild to disease transition and a 77.6% chance staying in the mild state.
Regression model for covariates
In the univariate analyses of treatment effect on disease progression based on Model 1 and Model 2, a period exceeding 8 months between the end of endodontic and prosthetic treatment was significantly associated with disease progression ([HR 2.84; 95%CI 1.16, 6.96] and [HR 2.48; 95%CI 1.01, 6.14] respectively). Based on Model 1, transitions from healthy to mild disease state were less likely in the Endo-fill group than in the Endo-post group [HR 0.33; 95%CI 0.12, 0.91] and for molars than front teeth [HR 0.33; 95%CI 0.12, 0.91] ().
Table 4. Hazard ratios with 95 % confidence intervals of the association between covariates and outcomes from the univariate analysis of Model 1 and Model 2.
In the adjusted analyses, a period exceeding 8 months between the end of the endodontic treatment and prosthetic treatment increased the risk of disease progression 3.16 times than a period of ≤ 8 months based on Model 1 [HR 3.16; 95%CI 1.06, 9.42] and 3.22 times based on Model 2 [HR 3.22;95% CI 1.07, 9.71] (). Our findings based on Model 1 also showed that patients in Endo-fill group were 60% less likely to become diseased after one year compared with patients in Endo-post group [HR 0.40, 95% CI 0.12, 0.94].
Table 5. Hazard ratios with 95 % confidence intervals of the association between covariates and outcomes from the multivariate analysis of Model 1 and Model 2.
Discussion
This study investigated the association between different types of post-endodontic restorations and the periapical status transitions, when periapical lesions were measured by standardized scoring of dental periapical radiographs taken at the start of the endodontic treatment and at a follow up point.
Teeth in the group restored with post and core restoration showed a higher hazard for transition to a non-healthy apical status compared with teeth restored with composite fillings. Teeth restored with composite fillings were 60% less likely to become diseased after approximately one year compared with teeth treated with posts. We therefore rejected the null hypothesis that there is no difference between posted and non-posted teeth. Our findings also suggest that time between the end of the endodontic treatment and the final restorative treatment can be an important determinant to the success of the endodontic treatment.
Most studies on coronal restorations and periapical status after endodontic treatment have used a cross-sectional study design [Citation8–10,Citation12] and thus missed the key confounding factor which is apical periodontitis at the baseline. Cross sectional studies offer the advantage of large sample sizes and random selection but give little information on the dynamics of the disease since no information on the timing of the disease is available. It has been repeatedly documented that the most significant factor for endodontic treatment outcome is the preoperative apical status [Citation10,Citation18]. The microbiological status of root-filled teeth with pre-operative lesions after disinfection will always be uncertain [Citation1,Citation19]. Therefore, the selection of initially uninfected teeth (defined by the absence of a periapical lesion) is a better baseline for follow-ups than a population of teeth with mixed diagnosis.
In the current study, a total of 284 teeth with known endodontic and restorative treatment history were examined. On recall, 22 teeth (7.7%) of these teeth were associated with periapical lesions according to Model 1. Of note, none of the included teeth had periapical pathosis at baseline.
Follow-up studies of endodontic treatment on teeth with a preoperative radiographic lesion show success rate of 73–86% of cases, whereas cases without a preoperative lesion have over 90% success rate by criteria corresponding to our Model 1 [Citation19]. We found a 92.3% success rate, which corresponds well with these findings.
One possible limitation of this study is the retrospective design with a rather short follow-up time. The European Society of Endodontology suggests a clinical and radiographic follow-up after at least one year [Citation18]. Failures developing after more than one year and so-called late failures are infrequent and only marginally affect overall evaluation of the periapical health in a group of teeth [Citation20,Citation21]. Others have concluded that 6–9 months evaluation appears to be an indicator for the final outcome of primary root canal treatment both in the presence and absence of initial apical periodontitis [Citation22]. The minimum follow-up time in our study was 8 months from the definitive restorative treatment, which should be sufficient to register most apical changes associated with treatment procedures.
The clinical procedures applied in the present study were standardized according to prescribed protocols and closely supervised by calibrated faculty members. This provided control over intra-operative factors that may influence the periapical status of root-filled teeth [Citation18,Citation21]. In particular, clinical factors related to the quality of the endodontic treatment such as aseptic working conditions, adequate disinfection, precise canal length measurement, adequate canal preparation, irrigation, complete root canal obturation were monitored closely [Citation7,Citation18,Citation21]. In addition, clinical factors related to the quality of the restoration such as ferrule, length of the post and marginal adaptation of the crown were controlled by calibrated faculty members [Citation14].
Most studies investigating the association between the quality of coronal restoration and apical status have used radiographic data only, and our results were also based on radiographic scoring of the periapical status. Radiographic interpretation is subjective and can be influenced by a variety of factors, such as changes in beam angulation [Citation20]. There are studies that have combined radiographic and clinical data [Citation9,Citation23,Citation24], and while combination of data would be expected to improve the validity of the results, Hommez [Citation23] and Dugas [Citation9] have found that the correlation between clinical and radiographic data is poor. Determinants such as age, periodontal status, existing adjacent teeth, or teeth in the opposite jaw were not taken into account in the present study; however, except possibly for periodontal probing depth, these factors may not be of particular significance for endodontic treatment outcome [Citation21,Citation22]
Which type of radiographic examination is more accurate in detecting pathoses in periapical area has been a matter of dispute. The quality of digital panoramic radiographs has been described by some to be sufficient for detecting apical pathoses compared with periapical radiography even in the anterior region [Citation12], whereas others argue that apical periodontitis may be underestimated when using panoramic radiographs and suggest two-dimensional periapical radiography as the technique of choice for routine assessment of diagnosis and management of endodontic disease [Citation25]. Cone beam computed tomography (CBCT) is significantly more sensitive in detecting apical periodontitis compared with periapical radiography [Citation26,Citation27] but the radiation dose is too high for routine endodontic examination, and it was not available at the time the data for this study was collected. The PAI index is well established as an effective scoring system for apical periodontitis, providing a scale from 1 (no disease) through 5 (apical radiolucency with signs of spreading). The system is based on a quantitative rather than qualitative approach to treatment outcome, making it possible to use the hazard concept on collected data.
The use of a reference set of radiographs reduces observer bias; there are histological correlates and calibration of observers that can be made independent of time and place [Citation28].
In the present study, PAI 2 was considered a healthy state in Model 1 Markov analysis, giving the traditional cut-off between PAI 2 and PAI 3 for success and failure. Model 1 uses less strict criteria for diagnosis of apical periodontitis than Model 2. In Model 2, PAI 2 was not considered a healthy state, as in Model 1, but a mild disease state, thus moving the cut off for disease to PAI 1. Markov analysis takes into account the progression of disease and has shown higher number of transitions counts to the mild disease stage (PAI 2) for Endo-post group, compared with cumulative numbers of the mild disease stage for the other two treatment groups. The proportion of teeth in a mild disease state at follow-up was 53/102 for the Endo-post group, 37/82 for the Endo-crown group and 31/100 for the Endo-fill group.
There is a wide variation in results when presenting outcome data by tooth type in the literature. Generally, the location and type of tooth are not considered to influence the outcome of non-surgical endodontic treatment. The complex anatomy associated with molar teeth does not appear to negatively influence the outcome of root canal treatment [Citation19]. We found, in univariate analysis, that transition from healthy to mild disease was less likely for molars than for front teeth; however, the influence of tooth type was insignificant in the multivariate analysis.
Contradictory results have been reported by different studies investigating the association between periapical status, post-endodontic treatment and survival of root canal-treated teeth [Citation15,Citation29,Citation30]. Some studies found association between survival of endodontically treated teeth and permanent coronal restorations [Citation31]. We did not assess the quality of the root canal treatment and the prosthetic restoration, but the treatments took place in a controlled environment following generally accepted protocols. The hazard ratios showed that the group receiving composite filling restorations was 70% (according to the univariate analysis) and 60% (according to multivariate analysis) less likely to become diseased after one year compared with the group receiving post restorations. The risk of disease progression increased by a factor of three as the time between endodontic treatment and prosthodontic treatment became longer than 8 months. The fact that the type of restoration was found to be predictive of apical periodontitis may be the result of case selection for posts and crowns: teeth with little remaining coronal tooth substance may more frequently be selected for treatment with posts. Such teeth may be at greater risk for failure than teeth with more coronal tooth substance intact [Citation32]. A prospective study assessing the effect of coronal tooth structure loss on the outcome of root canal treatment showed that <30% volume of remaining coronal tooth structure had a significantly higher endodontic failure rate than teeth with residual tooth structure volume >30% [Citation33].
In a review article, the proportion of teeth with post-retained restoration developed apical pathology was slightly lower than that of teeth without a post, but the difference was not statistically significant, and the heterogeneity of the studies reviewed substantial [Citation30]. A recent observational study showed that placing a post increased the odds of periapical health for 85%, attributing this to the tight seal provided by posts and the bactericidal corrosive deposits sealing the canal interface in the cases of metallic posts and core restorations [Citation12]. Differences in case selection may explain why the favourable results for posted teeth presented by Kielbassa and co-workers differed from the results of the current study [Citation12]. Poor cementation of temporary crowns or temporary posts, temporary restorations over long periods can lead to coronal leakage especially in cases of delayed permanent restorations [Citation31,Citation32]. On the other hand, post preparation procedures may disrupt the apical seal and microorganisms may invade the post space between appointments, whereby the treatment itself becomes the risk factor for a negative endodontic outcome. Based on the results of this study, it seems reasonable to suggest shortening the time between the end of endodontic treatment and the final restorative treatment, in cases where prosthetic restorations are indicated.
Conclusions
We found that 7.7% of 284 root-filled teeth without apical periodontitis at baseline developed clear apical pathology within a minimum of 8-month observational period. Teeth without radiographic lesions at baseline and restored with posts had higher hazard to transit from a healthy to a diseased periapical status compared with teeth restored with composite restorations. Controlled clinical trials with longer follow-up periods are needed to validate these findings.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
References
- Sjögren U, Hagglund B, Sundqvist G, et al. Factors affecting the long-term results of endodontic treatment. J Endod. 1990;16(10):498–504.
- Kirkevang LL, Vaeth M, Wenzel A. Ten-year follow-up of root filled teeth: a radiographic study of a Danish population. Int Endod J. 2014;47(10):980–988.
- Swanson K, Madison S. An evaluation of coronal microleakage in endodontically treated teeth. Part I. Time periods. J Endod. 1987;13(2):56–59.
- Khayat A, Lee SJ, Torabinejad M. Human saliva penetration of coronally unsealed obturated root canals. J Endod. 1993;19(9):458–461.
- Ricucci D, Bergenholtz G. Bacterial status in root-filled teeth exposed to the oral environment by loss of restoration and fracture or caries – a histobacteriological study of treated cases. Int Endod J. 2003;36(11):787–802.
- Ray HA, Trope M. Periapical status of endodontically treated teeth in relation to the technical quality of the root filling and the coronal restoration. Int Endod J. 1995;28(1):12–18.
- Moreno JO, Alves FR, Gonçalves LS, et al. Periradicular status and quality of root canal fillings and coronal restorations in an urban Colombian population. J Endod. 2013;39(5):600–604.
- Siqueira JF Jr., Rôças IN, Alves FR, et al. Periradicular status related to the quality of coronal restorations and root canal fillings in a Brazilian population. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100(3):369–374.
- Dugas NN, Lawrence HP, Teplitsky PE, et al. Periapical health and treatment quality assessment of root-filled teeth in two Canadian populations. Int Endod J. 2003;36(3):181–192.
- De Moor RJ, Hommez GM, De Boever JG, et al. Periapical health related to the quality of root canal treatment in a Belgian population. Int Endod J. 2000;33(2):113–120.
- Kirkevang LL, Orstavik D, Hörsted-Bindslev P, et al. Periapical status and quality of root fillings and coronal restorations in a Danish population. Int Endod J. 2000;33(6):509–515.
- Kielbassa AM, Frank W, Madaus T. Radiologic assessment of quality of root canal fillings and periapical status in an Austrian subpopulation – an observational study. PLoS One. 2017;12(5):e0176724.
- Eckerbom M, Magnusson T, Martinsson T. Prevalence of apical periodontitis, crowned teeth and teeth with posts in a Swedish population. Endod Dent Traumatol. 1991;7(5):214–220.
- Salvi GE, Siegrist Guldener BE, Amstad T, et al. Clinical evaluation of root filled teeth restored with or without post-and-core systems in a specialist practice setting. Int Endod J. 2007;40(3):209–215.
- Guldener KA, Lanzrein CL, Siegrist Guldener BE, et al. Long-term clinical outcomes of endodontically treated teeth restored with or without fiber post-retained single-unit restorations. J Endod. 2017;43(2):188–193.
- Orstavik D, Kerekes K, Eriksen HM. The periapical index: a scoring system for radiographic assessment of apical periodontitis. Endod Dent Traumatol. 1986;2(1):20–34.
- Kirkevang LL, Orstavik D, Wenzel A, et al. Prognostic value of the full-scale periapical index. Int Endod J. 2015;48(11):1051–1058.
- Quality guidelines for endodontic treatment: consensus report of the European society of Endodontology. Int Endod J. 2006;39(12):921–930.
- Kirkevang LL, Vaeth M. Epidemiology, treatment outcome, and risk factors for apical periodontitis. In: Orstavik D, editor. Essential endodontology: prevention and treatment of apical periodontitis. Oxford: Wiley; 2019. p. 143–178.
- Orstavik D. Time-course and risk analyses of the development and healing of chronic apical periodontitis in man. Int Endod J. 1996;29(3):150–155.
- Ng YL, Mann V, Rahbaran S, et al. Outcome of primary root canal treatment: systematic review of the literature – part 2. Influence of clinical factors. Int Endod J. 2008;41(1):6–31.
- Pirani C, Chersoni S, Montebugnoli L, et al. Long-term outcome of non-surgical root canal treatment: a retrospective analysis. Odontology. 2015;103(2):185–193.
- Hommez GMG, Coppens CRM, De Moor RJG. Periapical health related to the quality of coronal restorations and root fillings. Int Endod J. 2002;35(8):680–689.
- Frisk F, Hugosson A, Kvist T. Is apical periodontitis in root filled teeth associated with the type of restoration? Acta Odontol Scand. 2015;73(3):169–175.
- Dawson VS, Petersson K, Wolf E, et al. Periapical status of root-filled teeth restored with composite, amalgam, or full crown restorations: a cross-sectional study of a Swedish Adult Population. J Endod. 2016;42(9):1326–1333.
- Lopez FU, Kopper PM, Cucco C, et al. Accuracy of cone-beam computed tomography and periapical radiography in apical periodontitis diagnosis. J Endod. 2014;40(12):2057–2060.
- Kanagasingam S, Lim CX, Yong CP, et al. Diagnostic accuracy of periapical radiography and cone beam computed tomography in detecting apical periodontitis using histopathological findings as a reference standard. Int Endod J. 2017;50(5):417–426.
- Brynolf I. A histological and radiological study of the periapical region of human upper incisors [dissertation]. Stockholm (Sweden): Stockholm University; 1967.
- Dammaschke T, Steven D, Kaup M, et al. Long-term survival of root-canal-treated teeth: a retrospective study over 10 years. J Endod. 2003;29(10):638–643.
- Ng YL, Mann V, Gulabivala K. Tooth survival following non-surgical root canal treatment: a systematic review of the literature. Int Endod J. 2010;43(3):171–189.
- Lynch CD, Burke FM, Riordain RN, et al. The influence of coronal restoration type on the survival of endodontical treated teeth. Eur J Prosthodont Restor Dent. 2004;12(4):171–176.
- Al-Nuaimi N, Ciapryna S, Chia M, et al. A prospective study on the effect of coronal tooth structure loss on the 4-year clinical survival of root canal retreated teeth and retrospective validation of the dental practicality index. Int Endod J. 2020;53(8):1040–1049.
- Al-Nuaimi N, Patel S, Austin RS, et al. A prospective study assessing the effect of coronal tooth structure loss on the outcome of root canal retreatment. Int Endod J. 2017;50(12):1143–1157.