Abstract
Objective
The aims of this systematic review were to evaluate the clinical masticatory performance of implant-supported restorations, observe the occlusal force changes in the distribution of the implant restoration and reveal the positive and negative contributing factors of implant design and components based on the outcomes of digital occlusal measurement.
Material and methods
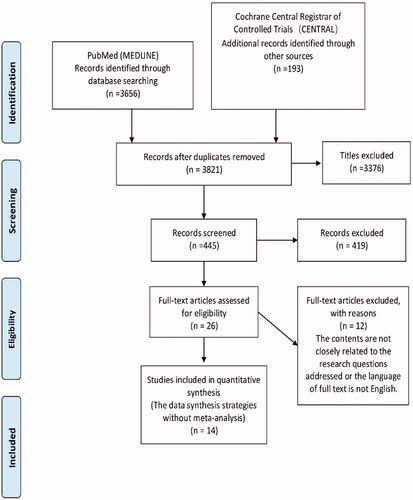
An extensive search was conducted through PubMed and CENTRAL to identify clinical trials on implant-retained restorations using digital occlusal analysis methods. Two researchers assessed the identified studies and data extraction independently, and the data synthesis strategies without meta-analysis that summarizes the effect estimates were adopted.
Results
The search screened 3821 titles and abstracts, then full-text analysis for 26 articles was performed, and 14 studies were included in the quantitative synthesis. Four of six studies for implant-retained overdenture showed statistically significant improved bite force when immediate loading (p = .00045, .00005, .00055, and .00005, respectively), and no statistically significant results in the other two studies (p = .225, .371, respectively.) However, the results of the favoured intervention were not statistically significant (p = .104, .166, respectively) in two studies of single posterior implant restorations. In all three studies, the bite force distributed on the implant prostheses of partially fixed implant-retained restoration increased statistically significantly (p = .013, .001, .05, respectively).
Conclusions
The edentulous restoration supported by implants seems to significantly improves bite force and chewing efficiency compared with conventional dentures. Regular quantitative occlusal measurement is recommended to avoid the possible risk of overload. Smaller implants size and relatively small and flexible attachment designs may be more conducive to the stability and retention of the restoration of atrophy of alveolar bone.
Introduction
Dental implant-supported restorations are extensively used for the oral reconstruction of partial and complete edentulism after evolving from experimental treatment to highly predictable alternative options of missing teeth in the past 50 years [Citation1–3]. Two primary goals of implant treatment are successful treatment results from the rehabilitation of normal oral physiological functions such as chewing, pronunciation, and aesthetics with high predictability and good long-term stability, in addition, it is crucial to reduce the occurrence of complications during healing and subsequent periods [Citation2,Citation4]. Various methods to evaluate the oral health-related outcomes include chewing efficiency, maximum bite force, patient satisfaction, and patient nutritional status [Citation5–8]. Each method has its advantages, but some indicators are subjective and lack comparability among the outcomes due to different observational contents.
Moreover, the clinical evidence is still insufficient because of inevitable limitations, such as selecting subjects, sample size setting, research purposes and significance, appropriate research methods, the objectivity of index evaluation, application of statistical methods, etc. Bite force and occlusal contact area are the critical factors used to evaluate chewing performance [Citation9,Citation10], so the digital presentation of these occlusal indicators could provide an effective way to evaluate the improvement of oral function quantitatively. Meanwhile, even with high success and survival rates (above 95%) [Citation11–14], implant-retained restorations are still not immune to complications [Citation4,Citation15,Citation16] due to physiological differences between the implant and natural tooth, such as displacement of the osseointegrated implant [Citation17,Citation18], tactile sensation of periodontal tissue [Citation19], the elastic modulus of root [Citation20]. Furthermore, the compressibility and deformability of periodontal ligament (PDL) in natural teeth can differ in force adaptation compared with osseointegrated implants under loading [Citation18]. Therefore, dental implants may be more prone to occlusal overloading. A considerable number of studies [Citation1,Citation21–24] reported the recommendations and considerations of occlusion in implant dentistry. However, this review mainly summarized the principles and strategies in implant restoration from the perspective of optimal occlusion and expounded the multiple factors that may cause overloading systematically. To the authors’ knowledge, no article focuses on the quantitative occlusal parameters, such as occlusal force applied on the implant-retained restorations or individual implant and changes in occlusal characteristics after placement implant-retained constructions in the views of clinical trials. Moreover, with the continuous advancement, quantitative analysis of occlusal parameters is essential objective clinical evidence for considering various designs and components of dental implants.
The primary objective of this systematic review was to evaluate the clinical masticatory performance of implant-supported restorations based on the outcomes of digital occlusal measurement; the secondary aims were to observe the occlusal force changes in the distribution of the implant restoration and reveal the positive and negative contributing factors of implant design and components in line of digital occlusal analysis. The null hypothesis is that no strong clinical evidence indicates that implant-supported restorations’ chewing performance is better than conventional rehabilitations.
Materials and methods
This review was registered at the National Institute for Health Research PROSPERO, International Prospective Register of Systematic Reviews (CRD42021236484).
General search strategy
This systematic review was conducted according to the guidelines of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (http://www.prismastatement.org) [Citation25].
Population. Partial or completely edentulous patients.
Intervention. Partial or full implant-supported restorations.
Comparison. Conventional complete restorations or prior to placement of implant-retained restoration.
Outcome. Digital quantitative occlusal parameters, such as occlusal force, contact area, contact time and contact number.
Literature search methodology
All relevant works of literature of implant retained reconstructions using digital occlusal analysis methods were included. The search criteria were set from 1 January 2016 to 31 July 2021. An extensive search was conducted from two online databases: MEDLINE/PubMed and Cochrane library/Embase. The keyword search criteria were as follows: PubMed: ((((‘occlusion’ OR ‘occlusal’ OR ‘occlude’ OR ‘bite force’ OR ‘contact’ OR ‘pressure’ OR ‘loading’ OR ‘chew’ OR ‘masticatory’)) AND ((‘scan’ OR ‘scanning’ OR ‘scanner’ OR ‘sensor’ OR ‘transducer’ OR ‘digital’ OR ‘digitization’ OR ‘dynamic’ OR ‘computerised’ OR ‘advanced’ OR ‘quantitative’))) AND ((‘implant’ OR ‘implant retained’ OR ‘implant supported’ OR ‘implant fixed’))) AND ((‘crown’ OR ‘bridge ’ OR ‘reconstruct ’ OR ‘reconstruction ’OR ‘superstructure ’ OR ‘restoration ’ OR ‘restorative ’ OR ‘prosthesis ’ OR ‘prostheses ’ OR ‘denture ’)); Cochrane: ‘implant’ AND (‘occlusion’ OR ‘occlusal’ OR ‘contact’) AND (‘scan’ OR ‘digital’ OR ‘computerised’ OR ‘advanced’).
Inclusion criteria
The human study, more than 18 years old.
Partial or complete dental implant-supported restoration.
A study evaluating occlusal parameters by digital method solely or combined with other methods.
Study results presented as quantitative parameters, not qualitative ones. In addition, the quantitative data of each study included at least one occlusal indicator. Primary outcomes: occlusal force. Secondary outcomes: occlusal contact area, occlusal contact time, and occlusal contact number.
Studies including clinical trial, systematic review (with and without meta-analysis).
Written in English.
Both abstract and full article available.
Exclusion criteria
Laboratory research.
Case report, short commentary.
Selection of studies
The review team was divided into two groups: TZ and XXL, BM and PM. Two groups independently screened the titles derived from the initial search in consideration for inclusion. After title screening, the abstracts obtained were scanned for inclusion by groups 1 and 2, respectively. Based on the selection of abstracts, articles were then obtained in full text. Disagreements were resolved by discussion. Finally, the selection based on inclusion/exclusion criteria is made for the full‐text articles by the authors TZ and BM. For this purpose, materials and methods, results, and discussions of these studies were screened. BB then double-checked the selected articles. Any issues regarding the selection during the screening were discussed within the groups to reach a consensus.
Data extraction and method of analysis
Two researchers (TZ and BM) independently extracted the data of the selected articles using data extraction tables. For standardization purposes, each researcher extracted the data of the same three articles at the beginning of the literature analysis, and then any disagreements were discussed, aiming at a consensus to standardize the subsequent analyses. Finally, all extracted data were double-checked by one senior researcher (BB). Information on the following parameters was extracted: author(s); year of publication; study design; the number of patients; follow-up time; demographic information of patients; features of the implant-retained restorations (implant type and design, number, location, restoration material and design of implants); digital measurement methods; quantitative parameters of occlusal outcomes that obtained from complete denture and implant supported rehabilitation, respectively, or those from partial edentulous patients and patients rehabilitated with implant retained restorations, which including magnitude and distribution of occlusal force, occlusal contact number and area, occlusal time and other occlusal related indicators.
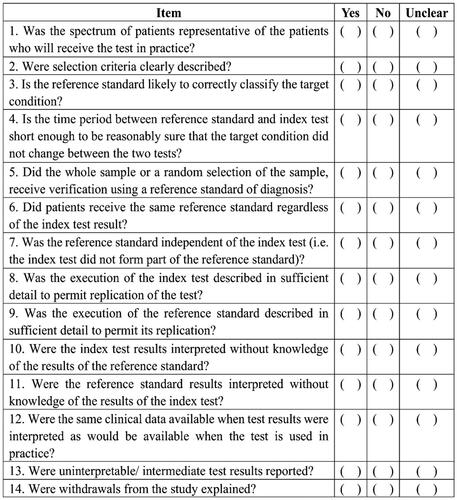
Bias risk assessment
Considering that different digital occlusal measurement tools obtained quantitative parameters, the Quality Assessment of Diagnostic Accuracy Studies (QUADAS) tool [Citation26] was implemented to measure the risk of bias of the included studies. It was achieved by asking 14 questions () for every study. For each question, a score of 1 was given if the answer was ‘yes’; a score of 0 was given if the answer was ‘no’ or ‘unclear’. Therefore, the highest possible score is 14, which indicates a lower risk of bias.
Data synthesis and statistic calculation
The data synthesis strategies were adopted without meta-analysis because of the overly diversified characteristics of included studies in terms of research design, research purposes, intervention types and results [Citation27]. According to the hypotheses, the maximum bite force was selected as the main outcome due to the acceptance of an important indicator of masticatory performance [Citation9,Citation10]. At least one quantitative result can be extracted from the experimental group and the control group. Therefore, the mean and standard deviation of maximum bite force were calculated when summarizing effect estimates and calculating the p values. Besides, the changes in occlusal force distributed on the individual implant from the baseline (immediate) to the last follow-up were analysed because this indicator is directly related to overloading evaluation. In addition to the above, other digital-related occlusal outcomes, such as occlusal contact area, occlusal contact time and occlusal contact number were extracted and presented. The effect estimates were calculated by Reviews Manager version 5.4.1 (The Nordic Cochrane Centre, Copenhagen, Denmark), and the one sided p values were used, since these contain information about the direction of effect [Citation28]. If there were multiple subgroups of intervention within a study, summary statistics were obtained by combining multiple subgroups. The average bite force was calculated via a within-subgroup standard deviation when the maximum bite force was expressed as the left and right sides, respectively, for the same subjects [Citation29].
The extracted outcome of maximum bite force was the bite force value of the full arch or posterior segment directly obtained via the digital means in the included study.
The time points of the compared data were pre-treatment and immediate placement of the implant-supported restorations; the time of occlusal force changes in implant restoration was defined from the baseline (immediate placement) to the last follow-up (the longest follow-up point) during the whole observational period (the intervals in observational period was each year except for 3 and 6 months).
The intervention measures were divided into implant-supported complete dentures or partially fixed prostheses according to the research questions addressed when summary statistics were applied. If the control group contained multiple types of dentures, only the traditional standard method (complete removable denture) was selected as the control. For the partially fixed prostheses, the data of pre placement of implant-retained restoration was considered as control.
The minimum number of studies for synthesis is two studies for one subgroup (different implant-retained restoration types).
If there were discrepancies between the results stated in the article and the raw data provided, the mean and standard deviation were calculated based on the raw data.
Results
Included studies
Fourteen studies [Citation30–43] were included in the present systematic review (). A total of 3656 and 193 articles were provided from PubMed and Cochrane Central respectively according to the search strategy, 28 papers were duplicated among those. A total of 3795 papers were excluded in the first (title and abstract) and 26 articles assessed for eligibility in the second (full-text) screening. It should be emphasized that the 0.839 of Kappa agreement coefficient (p = .000, 95% CI: 0.811–0.868) was achieved between two groups when initial abstract screening and 90 articles had been discussed before the 26 articles were determined. The characteristics of included studies are summarized in . The intervention group in the study included a total of 278 subjects with 695 implants, age from 18 to 87 years old, at least 135 females and 104 males. The shortest and longest follow-up dates that provided in the text were the immediate placement of the implant support restoration and 8 years post-placement, respectively. There were no randomized clinical trials; five studies were designed as prospective cohort or comparative studies, three were retrospective clinical trials, four were cross-sectional, and two were crossover clinical trials. Among them, nine studies [Citation31–33,Citation36,Citation37,Citation39,Citation40,Citation42,Citation43] focussed on implant-supported overdentures (IODs) vs. full arch removable prostheses before the implant placement, and two studies [Citation32,Citation39] also contained complete dentures supported by all-on-four treatment concept. Five studies [Citation30,Citation34,Citation35,Citation38,Citation41] focussed on fixed partial implant‐supported prostheses, the details of implant (design) of those were summarized in . Four different digital occlusal measuring instruments were applied. Seven studies [Citation30,Citation33–35,Citation38,Citation40,Citation41] used the T-scan (Tekscan, Inc., South Boston, MA), one study [Citation31] adopted the force transducer (three axis force sensor USL06-H5-50N, Tec Gihan Co., Ltd, Kyoto, Japan), two studies [Citation32,Citation37] employed a force sensor (Bite Force Sensor, Hariom electronics, Vadodara, Gujarat, India), four studies [Citation36,Citation39,Citation42,Citation43] applied a digital force gauge (Occlusal Force-Metre GM 10, Nagano Keiki). Each study contained at least one item of the digital occlusal outcome.
Table 1. Characteristics of included studies.
Bias risk assessment and details of outcomes
According to QUADAS guidelines, the quality scores ranged from 9 to 12 (out of 14). Due to the diversity of occlusal indicators, the quantitative indicators were classified into the following six categories according to different outcomes of the studies: maximum bite force (arch or segments), relative occlusal force distributed on the individual implant, the specific bite force measured at the moment during the chewing process, duration of the bite force and occlusal contact teeth number or occlusion time. All quantitative digital occlusal parameters and the clinical significance of each research are listed in . Two studies [Citation32,Citation37] focussed on the comparison of masticatory performance between implant overdentures and complete dentures. Four studies [Citation30,Citation34,Citation38,Citation41] observed the changes in occlusal force distribution after single crowns. Three studies [Citation33,Citation42,Citation43] observed the clinical manifestations of the occlusal force of implant-supported dentures of different designs or components. Four studies [Citation35,Citation36,Citation39, 0] analysed the factors influencing bite force or correlation between bite force and oral health, such as bone resorption, occlusal design and complications. One study [Citation31] measured the ability to adjust occlusal in implant-retained overdenture.
Table 2. Evaluation of risk bias and all quantitative parameters of outcome.
Summarizing the effect estimates of quantitative outcome
The available value of bite force selected from eight studies was analysed to evaluate the chewing efficiency of both experiment and control groups. Six studies [Citation19,Citation32,Citation36,Citation37,Citation40,Citation42] belonged to the implant-retained complete denture and two studies [Citation30,Citation41] to partially fixed implant restorations. The baseline and final data of the occlusal force distributed on the implant restoration from three studies [Citation30,Citation34,Citation38] were obtained and analysed.
Summarizing effect estimates of maximum bite force
From , 95% confidence intervals were seen because of the use of different units of the digital methods. Six studies compared the maximum occlusal force of implant-retained overdentures (1 study contained all-on-four implant-retained restoration) and conventional complete dentures. Among these six studies, the statistically significant favoured intervention results were found in four studies [Citation32,Citation37,Citation40,Citation42], and there was evidence of the benefit of improved bite force for implant-retained overdenture in the above four studies (p = .00045, .00005, .00055, .00005, respectively). No statistically significant results in the other two studies [Citation33,Citation36], and the p value was .225 and .371, respectively. Meanwhile, for the two studies [Citation30,Citation41] of single posterior implant restoration, no statistically significant results of the favoured intervention was found, there was no sufficient evidence of masticatory performance benefit for single implant posterior restoration in these two studies (p = .104, .166, respectively). The data synthesis strategies were adopted without meta-analysis because of the overly diversified characteristics of included studies in terms of research design, research purposes, intervention types and results [Citation27].
Table 3. Summary statistics of available data for the representative outcomes from each study.
Summarizing effect estimates of changes in occlusal force applied on the individual implant
Statistically significant changes of bite force distributed on the implant restoration were observed in three studies (p = .013, .001, .05, respectively).
Discussion
Although four studies performed the benefit of improved bite force for implant-retained overdenture (p = .00045, .00005, .00055, .00005, respectively) among six studies in comparison with the conventional complete denture, however, there was no sufficient evidence of masticatory performance benefit for single implant posterior restoration in the two include studies (p = .104, .166, respectively). Besides, substantial evidence of increased bite force distributed on the implant prostheses of partially fixed implant-retained restoration in all three studies (p = .0065, .0005, .025, respectively). As a proper meta-analysis cannot be performed, there are too many potential biases, including the timing of loading, implant-supported configuration and different populations, so there is no sufficient evidence to reject the null hypothesis.
Digital occlusal measurement device
The digital occlusal measurement tools used in fourteen studies mainly include:
A T-scan (Tekscan, Inc., South Boston, MA).
A force transducer (3 axis force sensor USL06-H5-50N, Tec Gihan Co., Ltd, Kyoto, Japan).
A force sensor (Bite Force Sensor, Hariom electronics, Vadodara, Gujarat, India).
A digital force gauge (Occlusal Force-Metre GM 10, Nagano Keiki).
Obvious advantages were recognized, such as directly obtaining the quantitative value of the bite force, the visible distribution of bite force in different arch segments (or calculation from the ratio through the measurement results), and the correlation between force and time to make it possible for in-depth study. However, in addition to the different measurement units, the outcomes are also limited by the thickness of the instruments, material sensitivity, as well as the accuracy and precision of mechanical characteristics of the bite force recording system, especially under the clinical oral operating environment [Citation44–46]. Therefore, the summarized effect results from 10 studies () also reflected these characteristics of different methods. It can be noticed that quantitative occlusal parameters represented multiple meanings, not only for comparison of chewing performance but also to reveal the correlations between occlusal features of implant restoration and oral related health according to the outcomes of all 14 studies. Hence, it is not difficult to infer that the appropriate choice of digital occlusion measurement method is mainly determined by the purpose and significance of the research or actual clinical conditions.
Maximum bite force and masticatory efficiency
Masticatory efficiency is defined academically as ‘the effort required for achieving a standard degree of comminution’ [Citation44]. The cumulative contribution of multiple factors such as bite force, the severity of malocclusion, occlusal contact area, loss of tooth body, type of posterior restoration, craniomaxillofacial morphology, and other functional activities bite force is one of the key factors [Citation9,Citation45]. Among six studies, the result of four studies indicated that the bite force of implant overdentures was significantly higher than conventional complete dentures when immediate placement [Citation32,Citation37,Citation40,Citation42], the other two studies [Citation33,Citation36] failed to demonstrate effects on chewing efficiency. An important reason for the former study [Citation33] was that the selected time point was immediate placement instead of the 1-year follow-up in the original study; the possible reason for the latter study [Citation36] was that the performance of bite force was greatly determined by the characteristics of the subjects due to a cross-sectional study design. The following views could explain the results of improved bite force: first, the ability of wear to comminute food during chewing is determined by the increment of retention and stability of the mandibular denture [Citation46,Citation47] rather than the degree of retained by implants or alveolar mucosa; in addition, the loss of teeth in elderly patients usually accelerate atrophy of the jaw closure muscles [Citation48] leading to pain and instability during chewing, the usage of implants has a positive training effect [Citation5,Citation49] on masseter so that stabilizing the mandibular denture by reducing vertical and horizontal denture movement and lowering the pain threshold during biting and chewing. Although the index of maximum bite force was not presented in AbeM’s study [Citation31], the implanted overdenture displayed a significantly shorter duration (the required time to split test foods) than the conventional full mouth denture during the chewing process (). This result was also consistent with the above viewpoints due to the differences in mucosal movement and stability between the two dentures. On the contrary, none of the studies [Citation30,Citation41] supported the significant improvement of bite force for partially fixed implant prostheses included, even if the actual research results indicated that the occlusal force changes of pre-and post-treatment were statistically significant via corresponding statistical methods. On the one hand, this indicated that the few numbers of missing teeth might have only a slight effect on chewing performance. On the other hand, only two partial dentures that single posterior implant restorations were analysed, and the primary purposes of these studies were to evaluate the redistribution of bite force in the prothesis and each segment. Therefore, the maximum bite force data for comparison were only before and after immediate treatment. T-scan was used to measure the percentage of bite force rather than the absolute value of bite force. It might be challenging to achieve both sides’ equality because the individual bite force of the patient was still regarded as a fixed whole and measured by a percentage even though the actual bite force value has increased.
Risk factors of overloading and complications
Overloading refers to stress around the implant components and bone–implant interface that is not both technically and biologically acceptable, which is often regarded as one of the potential causes for peri-implant bone loss and failure of the implant/implant prosthesis [Citation50–52], as well as the range of overload that biologically acceptable is also unknown [Citation53–55]. Three include studies [Citation30,Citation34,Citation38] reported the changes in the occlusal force distribution on implants prostheses, the results from those showed the tendency of a significantly increased occlusal force of prostheses, which suggested that implants may face the risk of overloading over time. It has been reported that a variety of contributing factors including the wear of natural teeth and occlusal surface of restorations, extrusion of the opposing occluding teeth and craniomaxillofacial growth [Citation56–58], recurring bone remodelling [Citation59,Citation60], the geometry and design of occlusal surface [Citation61,Citation62] could result in the changes of occlusal force distributed on implant restorations over time. For other included studies, Huang et al. [Citation35] revealed that occlusal force on each implant prosthesis could be reduced with increased crown-implant ratio to avoid potential overloading. The study of Alzoubi et al. [Citation39] found that the distribution of anterior segmental occlusal force was proportional positively to the occurrence of complications such as incisal acrylic teeth chipping. Similarly, Khuder et al. [Citation40] pointed out that for each 1% increase in bite force distribution, the increased bone resorption of the maxillary anterior and the posterior mandibular ridges increased by 0.3% and 0.2%, respectively. These factors have been described and emphasized as possible overloading factors in the relevant review of occlusion [Citation1,Citation18,Citation22–24]. These data may have vital guiding significance for clinical research because the quantitative correlations between the influencing factors and the changes for individualized subjects were presented intuitively.
Consideration of occlusal design and component
The essential considerations of occlusal design and components for edentulous implant-retained restoration are sufficient stability and retention, especially in ageing patients with alveolar ridge atrophy. A better choice is mini-implant-retained mandibular overdenture for the elderly with alveolar ridge absorption, chronic diseases, fear of surgery and economical choice. Mini implants have apparent advantages such as more accessible access to sufficient bone–implant width, lesser surgical invasion and pain, and shorter healing time than the standard implants [Citation63,Citation64]. Kabbua et al. [Citation33] demonstrated an average of 5.63% significant improvement in occlusal force post-1-year treatment using mini-IODs. It also did not impair the balancing occlusion, which has been designed, and better clinical performance was obtained with an increase in the number of occlusal contact teeth and patient satisfaction for 1-year follow-up (). However, it must be noticed that disintegration of the mini-dental implants could result from excessive occlusal forces, such as using the anterior part of the denture only. Besides, in the included study [Citation43] of lower complete prostheses supported with four interforaminal NDIs (narrow dental implants), the results showed the maximum bite force improved from 46.6 N (pre-treatment) to 56.6 N (immediate post-treatment) and finally to 103.9 N (1 year follow up). Hence, the authors inferred that a lower complete prosthesis retained with four interforaminal NDIs could be a minimally invasive and economical approach to improve oral function, especially in elderly patients with limited bone support ().
Furthermore, the attachment system of implant-retained overdentures was highly concerned [Citation65,Citation66] because the type of attachment system influences the retention and stability of the complete denture. In the present review, one study [Citation33] used the Equator® attachment and emphasized the advantages, including its smaller size than other attachment systems and fewer prosthetic complications than ball attachments. One study [Citation42] concluded that resilient telescopic attachment was associated with increased chewing efficiency and maximum bite force compared to bar attachments when used to retain overdentures to the implants in patients with atrophic mandibles.
The limitations of this systematic review are as follows:
The studies' diversities in terms of research purposes, design, and multiple outcomes bring about the heterogeneity and the limited effect summarized methods among the studies.
The low level of evidence of the included studies is a bias, for the reasons of no randomized clinical trials, five prospective cohort or comparative studies, three retrospective, four cross-sectional and two crossover clinical trials.
The quality assessment used in this study is closely related to the results reporting, so well-conducted research may be scored lowly in the quality assessment if the methods and results are not reported in sufficient detail.
The study only retrieved the data of published papers but did not collect and analyse the results from unpublished articles.
The partial denture analysed in this review was the single fixed posterior restoration only. The reasonably narrow inclusion of partially fixed prostheses significantly increased the bias of result judgement based on the null hypothesis.
Conclusion
Given the limitations of this study, the following conclusions can be drawn:
Based on the limited evidence, the edentulous restoration supported by implants seems to significantly improve bite force and chewing efficiency when compared with the conventional dentures; however, the limitations of type and number included in this study might conceal the effect of improved chewing efficiency of partial fixed implant prostheses. With the continuous advancement that designs and components of dental implants, the research findings could supply strategies and considerations for reference from the perspective of how to maximize oral function. For the further studies, the sample size should be increased and the randomized controlled trials should be considered, and in addition to the time of immediate loading, at least 1 year or long-term observational time points are required.
Regularly quantitative occlusal measurement is recommended because potential overload factors such as increased occlusal force distributed on the restoration and excessive occlusal force applied in the anterior were observed.
The less dimensional implant and relatively small and elastic attachment design may be more beneficial to the stability and retention of the restoration for edentulous with alveolar bone atrophy.
Disclosure statement
The authors declare no conflicts of interest.
Additional information
Funding
References
- Koyano K, Esaki D. Occlusion on oral implants: current clinical guidelines. J Oral Rehabil. 2015;42(2):153–161.
- Buser D, Sennerby L, De Bruyn H. Modern implant dentistry based on osseointegration: 50 years of progress, current trends and open questions. Periodontol 2000. 2017;73(1):7–21.
- Amornvit P, Rokaya D, Bajracharya S, et al. Management of obstructive sleep apnea with implant retained mandibular advancement device. World J Dent. 2014;5(3):184–189.
- Rokaya D, Srimaneepong V, Wisitrasameewon W, et al. Peri-implantitis update: risk indicators, diagnosis, and treatment. Eur J Dent. 2020;14(4):672–682.
- Boven GC, Raghoebar GM, Vissink A, et al. Improving masticatory performance, bite force, nutritional state and patient’s satisfaction with implant overdentures: a systematic review of the literature. J Oral Rehabil. 2015;42(3):220–233.
- Müller F, Hernandez M, Grütter L, et al. Masseter muscle thickness, chewing efficiency and bite force in edentulous patients with fixed and removable implant-supported prostheses: a cross-sectional multicenter study. Clin Oral Implants Res. 2012;23(2):144–150.
- Kroll P, Hou L, Radaideh H, et al. Oral health-related outcomes in edentulous patients treated with mandibular Implant-Retained dentures versus complete dentures: systematic review with meta-analyses. J Oral Implantol. 2018;44(4):313–324.
- Khoury-Ribas L, Ayuso-Montero R, Willaert E, et al. Do implant-supported fixed partial prostheses improve masticatory performance in patients with unilateral posterior missing teeth? Clin Oral Implants Res. 2019;30(5):420–428.
- Koc D, Dogan A, Bek B. Bite force and influential factors on bite force measurements: a literature review. Eur J Dent. 2010;4(2):223–232.
- Varga S, Spalj S, Lapter Varga M, et al. Maximum voluntary molar bite force in subjects with normal occlusion. Eur J Orthodont. 2011;33(4):427–433.
- Fischer K, Stenberg T. Prospective 10-year cohort study based on a randomized controlled trial (RCT) on implant-supported full-arch maxillary prostheses. Part 1: sandblasted and acid-etched implants and mucosal tissue. Clin Implant Dent Relat Res. 2012;14(6):808–815.
- Gotfredsen K. A 10-year prospective study of single tooth implants placed in the anterior maxilla. Clin Implant Dent Relat Res. 2012;14(1):80–87.
- Adell R, Eriksson B, Lekholm U, et al. Long-term follow-up study of osseointegrated implants in the treatment of totally edentulous jaws. Int J Oral Maxillofac Implants. 1990;5(4):347–359.
- Goh EXJ, Lim LP. Implant maintenance for the prevention of biological complications: are you ready for the next challenge? J Invest Clin Dent. 2017;8(4):e12251.
- Buser D, Janner SF, Wittneben JG, et al. 10-year survival and success rates of 511 titanium implants with a sandblasted and acid-etched surface: a retrospective study in 303 partially edentulous patients. Clin Implant Dent Relat Res. 2012;14(6):839–851.
- Degidi M, Nardi D, Piattelli A. 10-year follow-up of immediately loaded implants with TiUnite porous anodized surface. Clin Implant Dent Relat Res. 2012;14(6):828–838.
- Schulte W. Implants and the periodontium. Int Dent J. 1995;45(1):16–26.
- Kim Y, Oh TJ, Misch CE, et al. Occlusal considerations in implant therapy: clinical guidelines with biomechanical rationale. Clin Oral Implants Res. 2005;16(1):26–35.
- Isidor F. Histological evaluation of peri-implant bone at implants subjected to occlusal overload or plaque accumulation. Clin Oral Implants Res. 1997;8(1):1–9.
- Sarfaraz H, Paulose A, Shenoy KK, et al. A three-dimensional finite element analysis of a passive and friction fit implant abutment interface and the influence of occlusal table dimension on the stress distribution pattern on the implant and surrounding bone. J Indian Prosthodont Soc. 2015;15(3):229–236.
- Gross MD. Occlusion in implant dentistry. A review of the literature of prosthetic determinants and current concepts. Aust Dent J. 2008;53(1):S60–S8.
- Sheridan RA, Decker AM, Plonka AB, et al. The role of occlusion in implant therapy: a comprehensive updated review. Implant Dent. 2016;25(6):829–838.
- Rilo B, da Silva JL, Mora MJ, et al. Guidelines for occlusion strategy in implant-borne prostheses. A review. Int Dent J. 2008;58(3):139–145.
- Graves CV, Harrel SK, Rossmann JA, et al. The role of occlusion in the dental implant and peri-implant condition: a review. Open Dent J. 2016;10:594–601.
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and Meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
- Whiting P, Rutjes AW, Reitsma JB, et al. The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol. 2003;3:25.
- Campbell M, McKenzie JE, Sowden A, et al. Synthesis without Meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ. 2020;368:l6890.
- McKenzie JE, Brennan SE. Synthesizing and presenting findings using other methods. Cochrane handbook for systematic reviews of interventions. Hoboken (NJ): John Wiley & Sons; 2019. p. 321–347.
- Higgins JP, Li T, Deeks JJ. Choosing effect measures and computing estimates of effect. Cochrane handbook for systematic reviews of interventions. Hoboken (NJ): John Wiley & Sons; 2019. p. 143–176.
- Zhou T, Wongpairojpanich J, Sareethammanuwat M, et al. Digital occlusal analysis of pre and post single posterior implant restoration delivery: a pilot study. PLoS One. 2021;16(7):e0252191.
- Abe M, Wada M, Maeda Y, et al. Ability to adjust occlusal force in implant-supported overdenture wearers. J Prosthodont Res. 2021;65(1):106–114.
- Soni R, Yadav H, Pathak A, et al. Comparative evaluation of biting force and chewing efficiency of all-on-four treatment concept with other treatment modalities in completely edentulous individuals. J Indian Prosthodont Soc. 2020;20(3):312–320.
- Kabbua P, Aunmeungtong W, Khongkhunthian P. Computerised occlusal analysis of mini-dental implant-retained mandibular overdentures: a 1-year prospective clinical study. J Oral Rehabil. 2020;47(6):757–765.
- Luo Q, Ding Q, Zhang L, et al. Analyzing the occlusion variation of single posterior implant-supported fixed prostheses by using the T-scan system: a prospective 3-year follow-up study. J Prosth Dent. 2020;123(1):79–84.
- Huang YF, Chang CT, Muo CH, et al. The association of variables of fibular reconstructed mandible and bite force in oral cancer patients with dental implant rehabilitation. J Craniomaxillofac Surg. 2018;46(11):1979–1983.
- Schimmel M, Memedi K, Parga T, et al. Masticatory performance and maximum bite and lip force depend on the type of prosthesis. Int J Prosthodont. 2017;30(6):565–572.
- Sharma AJ, Nagrath R, Lahori M. A comparative evaluation of chewing efficiency, masticatory bite force, and patient satisfaction between conventional denture and implant-supported mandibular overdenture: an in vivo study. J Indian Prosthodont Soc. 2017;17(4):361–372.
- Madani AS, Nakhaei M, Alami M, et al. Post-insertion posterior single-implant occlusion changes at different intervals: a T-Scan computerized occlusal analysis. J Contemp Dent Pract. 2017;18(10):927–932.
- Alzoubi F, Bedrossian E, Wong A, et al. Outcomes assessment of treating completely edentulous patients with a fixed Implant-Supported profile prosthesis utilizing a graftless approach. Part 1: clinically related outcomes. Int J Oral Maxillofac Implants. 2017;32(4):897–903.
- Khuder T, Yunus N, Sulaiman E, et al. Association between occlusal force distribution in implant overdenture prostheses and residual ridge resorption. J Oral Rehabil. 2017;44(5):398–404.
- Roque MA, Gallucci GO, Lee SJ. Occlusal pressure redistribution with single implant restorations. J Prosthodont. 2017;26(4):275–279.
- Elsyad MA, Khairallah AS. Chewing efficiency and maximum bite force with different attachment systems of implant overdentures: a crossover study. Clin Oral Implants Res. 2017;28(6):677–682.
- Enkling N, Saftig M, Worni A, et al. Chewing efficiency, bite force and oral health-related quality of life with narrow diameter implants - a prospective clinical study: results after one year. Clin Oral Impl Res. 2017;28(4):476–482.
- The glossary of prosthodontic terms. J Prosth Dent. 1999;81(1):39–110.
- Hatch JP, Shinkai RS, Sakai S, et al. Determinants of masticatory performance in dentate adults. Arch Oral Biol. 2001;46(7):641–648.
- Geertman ME, Slagter AP, van Waas MA, et al. Comminution of food with mandibular implant-retained overdentures. J Dent Res. 1994;73(12):1858–1864.
- Fontijn-Tekamp FA, Slagter AP, Van Der Bilt A, et al. Biting and chewing in overdentures, full dentures, and natural dentitions. J Dent Res. 2000;79(7):1519–1524.
- Newton JP, McManus FC, Menhenick S. Jaw muscles in older overdenture patients. Gerodontology. 2004;21(1):37–42.
- Müller F, Duvernay E, Loup A, et al. Implant-supported mandibular overdentures in very old adults: a randomized controlled trial. J Dent Res. 2013;92(12):154S–160s.
- Schwarz MS. Mechanical complications of dental implants. Clin Oral Implants Res. 2000;11(1):156–158.
- Hsu YT, Fu JH, Al-Hezaimi K, et al. Biomechanical implant treatment complications: a systematic review of clinical studies of implants with at least 1 year of functional loading. Int J Oral Maxillofac Implants. 2012;27(4):894–904.
- Misch CE, Bidez MW. Implant-protected occlusion: a biomechanical rationale. Compendium 1994;15(11):1330.
- Duyck J, Vandamme K. The effect of loading on peri-implant bone: a critical review of the literature. J Oral Rehabil. 2014;41(10):783–794.
- Naert I, Duyck J, Vandamme K. Occlusal overload and bone/implant loss. Clin Oral Implants Res. 2012;23(6):95–107.
- Chang M, Chronopoulos V, Mattheos N. Impact of excessive occlusal load on successfully-osseointegrated dental implants: a literature review. J Investig Clin Dent. 2013;4(3):142–150.
- Mundhe K, Jain V, Pruthi G, et al. Clinical study to evaluate the wear of natural enamel antagonist to zirconia and metal ceramic crowns. J Prosth Dent. 2015;114(3):358–363.
- Palaniappan S, Elsen L, Lijnen I, et al. Nanohybrid and microfilled hybrid versus conventional hybrid composite restorations: 5-year clinical wear performance. Clin Oral Invest. 2012;16(1):181–190.
- Daftary F, Mahallati R, Bahat O, et al. Lifelong craniofacial growth and the implications for osseointegrated implants. Int J Oral Maxillofac Implants. 2013;28(1):163–169.
- Piattelli A, Artese L, Penitente E, et al. Osteocyte density in the peri-implant bone of implants retrieved after different time periods (4 weeks to 27 years). J Biomed Mater Res B Appl Biomater. 2014;102(2):239–243.
- Albrektsson T, Chrcanovic B, Östman PO, et al. Initial and long-term crestal bone responses to modern dental implants. Periodontol 2000. 2017;73(1):41–50.
- Rezende CE, Borges AF, Gonzaga CC, et al. Effect of cement space on stress distribution in Y-TZP based crowns. Dent Mater. 2017;33(2):144–151.
- De Jager N, Pallav P, Feilzer AJ. The influence of design parameters on the FEA-determined stress distribution in CAD-CAM produced all-ceramic dental crowns. Dent Mater. 2005;21(3):242–251.
- de Souza RF, Ribeiro AB, Della Vecchia MP, et al. Mini vs. Standard implants for mandibular overdentures: a randomized Trial. J Dent Res. 2015;94(10):1376–1384.
- Aunmeungtong W, Kumchai T, Strietzel FP, et al. Comparative clinical study of conventional dental implants and mini dental implants for mandibular overdentures: a randomized clinical trial. Clin Implant Dent Relat Res. 2017;19(2):328–340.
- Heckmann SM, Winter W, Meyer M, et al. Overdenture attachment selection and the loading of implant and denture-bearing area. Part 2: a methodical study using five types of attachment. Clinical Oral Implants Research. 2001;12(6):640–647.
- Heckmann SM, Winter W, Meyer M, et al. Overdenture attachment selection and the loading of implant and denture-bearing area. Part 1: in vivo verification of stereolithographic model. Clin Oral Implants Res. 2001;12(6):617–623.