Abstract
Objective
Our retrospective register-based observational study evaluated age‐specific aspects and changes in volume and content of direct restorative procedures, pulp cappings and enhanced caries prevention measures given to adults.
Methods
Data included all treatments provided for 20- to 60-year-olds visiting the Helsinki City Public Dental Service (PDS) in 2012 and 2017. For both years, the data were aggregated into 5-year age groups. Data included means of DMFT indices, number and size of direct restorations, number of specific codes for pulp cappings and enhanced prevention.
Results
Around half of all patients received restorations, 39,820 (50.9%) in 2012 and 43,392 (45.9%) in 2017. The greatest increase in DMFT means by age cohort was found for the 2012 age cohort of 25- to 29-year-olds and the smallest for the 2012 age cohort of 45- to 49-year-olds. In each same-age group and each age cohort, the enhanced prevention in 2017 was less frequent than in 2012. The proportion of two-surface restorations accounted for 44.7% of procedures in 2012 and 45.9% in 2017, followed by an increasing proportion of one-surface restorations, from 28.3% in 2012 to 32.9% in 2017. Associations between restoration size and age group were highly significant (p < .001).
Conclusions
The volume of direct restorative procedures and enhanced prevention measures were strongly age-dependent. Restorative treatment procedures were more frequent in older age groups than in younger age groups, and vice versa for enhanced prevention and pulp cappings. The magnitude of restorative treatment decreased slowly from 2012 to 2017, and overall enhanced preventive treatment was limited.
Introduction
Direct restorations and preventive measures are common procedures at dental appointments [Citation1–3] although the F component of DMF has been in decline in some countries [Citation4–6]. On average, 57% of dentists’ worktime involves restorative treatment according to a questionnaire study among Public Dental Service (PDS) dentists in Norway [Citation1]. In Finland, restorative treatments for adults accounted for 26% of all treatment measures provided by the PDS in 2009 [Citation7] and for 36% of all reimbursed measures provided by the private sector in 2017 [Citation8]. In Australia, adults received a mean of 0.7–0.8 restorations during a dental visit in the previous 12 months in 2013 [Citation9].
Regarding professionally applied prevention, four-fifths out of the 73 million adults aged 24–65 years in the USA received at least one preventive procedure according to the Medical Expenditure Panel Survey [Citation10]. Another study based on a public insurance database from Ireland reports that preventive treatments are increasing; the mean number of provided prevention measures per patient was 1.0 [Citation11]. In Brazil, older patients (>65 years) were more likely to receive preventive procedures than younger adults [Citation2]. In Finland, enhanced preventive treatment measures among adults have been declining from 2001 to 2013 at PDS in southern Finland [Citation12].
The ongoing health and social services reform in Finland requires all available information when planning services for citizens. Hopefully this reform will provide equal preventive and restorative treatments and reduces oral health inequalities between e.g. social classes and access to services. Contemporary caries guidelines stress the low speed of caries progression, personalized prevention planning and tooth-preserving operative methods. To preserve pulpal vitality in deep caries lesions, stepwise excavation is indicated for both young and older patients [Citation13,Citation14]. In the private sector, a decrease in the volume of pulp cappings and direct restorations from 2012 to 2017 has been described in all adults [Citation15,Citation16]. There is currently no knowledge about the volumes of these treatment measures at PDS in Finland. Since the modification of health and social services in Finland is going on, planning services for citizens necessitates detailed information of contents of realized treatment on caries-based needs.
Our aim was to evaluate age‐specific aspects and changes in volume and content of direct restorative procedures (including pulp capping) and enhanced caries prevention measures provided for 20- to 60-year-olds visiting Helsinki City PDS in 2012 and 2017.
Our hypothesis was that age-related differences exist in volume and content of restorative and enhanced preventive treatment among adults attending PDS.
Materials and methods
Background
In Finland, oral health services for adults are provided in both the public and the private sector. At PDS adult patients pay fixed fees that are highly subsidized. In the private sector dentists are paid by fee-for-service. Oral health services at Helsinki City PDS are available for all adults and services are not restricted to special groups. PDS dentists receive fixed monthly salary and additional incents based on different types and numbers of treatments provided. Additional incents include e.g. restorations but not prevention. The population:dentist ratio was 1146:1 in 2004 and 1373:1 in 2018 in the whole country. In the metropolitan area there is neither shortage of dentists at PDS nor in the private sector – the population:dentist ratio being 2091:1 in 2018.
This retrospective register-based observational study utilized the Helsinki City PDS database from the years 2012 and 2017. No sampling was done since this study included all treatments in the above-mentioned years for adults aged 20–60 years. For both years, the data were aggregated into 5-year age groups from 20 to 60 years. Register-based data gathered for this study are aggregated and the observation unit is age group. Ethics approval was not required since this data included no information on patient’s identity.
In Finland, dental treatment codes are uniform for all service providers. The National Institute for Health and Welfare (THL) maintains these codes, ensuring that ordinary oral health prevention is provided at every dental visit. Specific codes for preventive measures are designated only for patients at moderate or high risk of oral diseases (e.g. caries, gingivitis and periodontitis) and this altered risk category must be documented in patient records. We use the umbrella term ‘enhanced prevention’ for these codes.
The aggregated data included means of DMFT-indices for the 5-year age groups, i.e. sums of decayed (D), missing (M) and filled (F) permanent teeth. Mean values of DT, MT and FT were not separately given. The classification of oral health care procedures maintained by the THL includes the subtitles, each with an individual prefix of three letters: SCA for preventive treatment, SFA for direct restorations, SFC for other restorative procedures and SGC for other pulpal treatments. Numbers and size of direct restorations were derived from THL codes with the prefix SFA recorded by tooth as follows: SFA00 minor restoration or small repair, SFA10 one surface, SFA20 two surface, SFA30 three surface, SFA40 four surface or crown. Each restoration code includes removal of old restoration material (when needed), cavity preparation, lining and base materials, finishing and polishing. In addition, SGC10 is defined as indirect and direct pulp capping, which can be used for stepwise excavation as well. Additional procedures necessary for restorative treatment have their own codes (SFC01 and SFC92) such as parapulpal pins or root canal posts. Restorative procedures were defined here as restorations combined with additional procedures. The aggregated data included no information on restored teeth by type of tooth. Codes for enhanced prevention (SCA01, SCA02, SCA03) include oral health and nutrition guidance, at-home oral care instructions, fluoride varnishes and prophylaxis cleaning and were combined into one prevention measure (tailored motivational communication).
A patient was defined as an actual user of Helsinki City PDS having a dental appointment the year in question. A patient provided with restoration was defined as one who has received at least one restorative treatment measure (including pulp capping) the year in question. A patient with enhanced prevention was defined as one who has received at least one enhanced preventive treatment measure.
Statistical analyses
Statistical analyses were carried out on the aggregated data instead of individual-based micro-level data. The data cover all patients aged between 20 and 60 years who attended Helsinki City PDS in 2012 and 2017 and the presented estimates are age group-based parameters. Comparisons are possible for both same-age groups (e.g. between 20- and 24-year-olds in 2012 and in 2017) and age cohorts (e.g. between 20- and 24-year-olds in 2012 and 25- and 29-year-olds in 2017). Descriptive statistics included proportions and means. Associations were evaluated by Pearson’s correlation coefficient and Chi-square tests. Data handling, analyses and graphics were performed with Survo MM software (version 3.4.1; Survo Systems, Helsinki, Finland).
Results
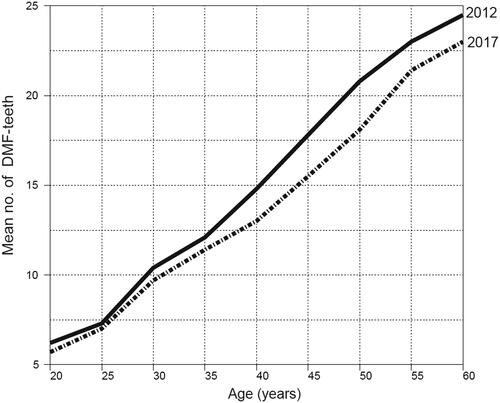
The shapes of mean DMFT values for patients aged 20–60 years attending Helsinki City PDS in 2012 and 2017 are shown in . Comparison between same-age groups revealed the greatest mean DMFT decrease for 50- to 54-year-olds, 2.7, as DMFT was 20.8 in 2012 and 18.1 in 2017. The smallest decrease, 0.3, was found for 25- to 29-year-olds, as DMFT was 7.3 in 2012 and 7.0 in 2017. Increase in DMFT means by age cohort fluctuated widely; the greatest increase, 2.4, was found for the 2012 age cohort of 25- to 29-year-olds and the smallest increase, 0.3, for the 2012 age cohort of 45- to 49-year-olds.
Figure 1. Mean DMFT in 20- to 60-year-old patients in Helsinki City PDS in 2012 (n = 39,820) and in 2017 (n = 43,392). Correlation between DMFT and age (r = 0.986) and year (r= −0.121).
Around half of all patients aged 20–60 years received restorations: 39,820 (50.9%) in 2012 and 43,392 (45.9%) in 2017 (). In both years, the proportions were greater the older the age group, with the relationships with age being linear. Enhanced prevention was provided for 3141 patients, 7.9% of restoration patients in 2012 and for 2150 patients (5.0%) in 2017. Proportions showed linearly descending trends with strong inverse correlations in both years. In each same-age group and each age cohort, the enhanced prevention in 2017 was less frequent than in 2012.
Table 1. Description (numbers and proportions) of restoration and enhanced prevention patients by 5-year age groups attending Helsinki City PDS in 2012 and 2017.
Per all patients, the average number of restorations received was 1.1 in 2012 and 0.9 in 2017, the values in both years being higher the older the age group (). Per restoration patients, the average number of restorations was 2.2 in 2012 and 2.0 in 2017; a slightly descending trend from 2012 to 2017 was found both by same-age group and by age cohort.
Table 2. Numbers of restorations, mean number of restorations per patient (Pts) and mean number of restorations per restoration patient (RePts) according to 5-year age groups at Helsinki City PDS in 2012 and 2017.
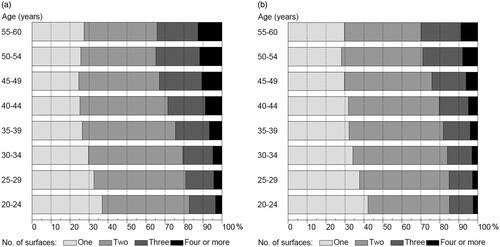
The proportion of two-surface restorations accounted for nearly half of all procedures in both years: 44.7% in 2012, 45.9% in 2017, followed by an increasing proportion of one-surface restorations, from 28.3% in 2012 to 32.9% in 2017. Restorations with size larger than two surfaces showed a decrease of around 3 percentage points from 2012 to 2017: for three-surface restorations from 18.9% to 16.1% and for the rest, from 8.1% to 5.1%. demonstrates the distributions by age group. Associations between restoration size and age group were highly significant (p < .001) in both years. Proportions of one-surface restorations showed a descending trend from the youngest to the oldest age group, and three- to four-surface restorations, an ascending trend.
Figure 2. Distributions (%) of restorations performed on 20- to 60-year-old patients at Helsinki City PDS in 2012 (n = 86,845) (a) and in 2017 (n = 86,438) (b). Restorations classified by size (no. of surfaces filled). Minor repairs are combined with the one-surface category.
Enhanced prevention was given to 11.1% of restoration patients in 2012 and to 5.8% in 2017 (). The volume of enhanced prevention showed descending values with strong inverse correlations with age group in both years. For each age cohort, a notable decrease in volume was found from 2012 to 2017. Pulp cappings were used to treat 3.6% of teeth restored in 2012 and 2.8% of teeth in 2017. In line with enhanced prevention, pulp cappings showed strong inverse correlations and followed similar changes in volume by age group and age cohort.
Table 3. Enhanced prevention measures provided for restoration patients (RePts) and pulp cappings made per 100 restored teeth (ReT) of Helsinki City PDS patients by 5-year age groups in 2012 and 2017.
Discussion
As hypothesized, our results show that the volume and content of direct restorative procedures and enhanced prevention measures were strongly age-dependent among 20- to 60-year-olds attending Helsinki City PDS in 2012 and 2017. Restorative treatment procedures were more frequent in older age groups than in younger age groups, and vice versa for enhanced prevention and pulp cappings, the relationships with age being linear. The proportions of one- and two-surface restorations decreased with age, while those of three- and four-surface restorations increased. Changes regarding volume of restorative treatment were minor between same-age groups and age cohorts in 2012 and 2017, probably due to replacement of restorations, since the observable decrease found in the means of DMFT indices speaks for improvement in dental health. Numbers of patients among same-age groups and age cohorts were not equal in 2012 and 2017, but there was no dramatic change in treatment procedure ratios. However, a clear decrease in the proportion of enhanced preventive treatments was apparent between same-age groups and age cohorts in 2012 and 2017.
Volume and content of restorative procedures
Around half of all patients received restoration procedures at Helsinki City PDS. This is significantly more than in the study by Linden et al. [Citation12], where restorative procedures among adults accounted for 20% of all dental procedures in 2013 at five other PDSs in southern Finland. In their study, however, caries-related treatments altogether accounted for as much as 60% of dentists’ worktime. One can speculate that Helsinki City PDS, responsible for 600,000 inhabitants, could be under-resourced and caries-related emergency-type appointments are more easily available than routine check-ups with comprehensive dental care compared with mid-sized PDSs having better resources, but no evidence has been published to confirm this view.
Surprisingly, the total proportion of restoration patients was lower in Helsinki City PDS (45.9% in 2017) than in the Finnish private sector (61.1% in 2017) [Citation16], where patients with a higher socio-economic status predominate. Widström et al. [Citation17] showed a similar pattern in southern Finland among adults: at PDS 1467 restorative procedures per 1000 patients and in the private sector 1807 per 1000 patients, but these statistics are from the year 2009. Such imbalance may indicate undertreatment in the public sector or overtreatment in the private sector or is just a sign of lacking resources due to recently reported [Citation18] patients’ flow to the public sector. Differences in treatment patterns between sectors have been reported from Norway as well, where PDS dentists preferred more often less invasive treatments and restoration repairs than private dentists [Citation19].
In our study, the share of one-surface restorations increased across the five years observed, which could be interpreted as either a sign of repair of restorations or minimal invasive dentistry. In addition, the decrease of large restorations in younger population (those under 40 years), can partly be explained by the introduction of fluoride toothpaste in the 1970s. In Finland, caries affected and missing teeth were seen less often among 30- to 4-year-olds compared to older age groups in the early 2000s [Citation20]. According to an epidemiological study, about 1 in 6 women and 1 in 3 men over 30 years of age had untreated tooth decay; on average, women had 0.3 and men 0.7 decayed teeth in Finland and the need for restorative treatment showed practically no difference from 2000 to 2011 [Citation21]. Previous studies using nationwide representative samples of adults’ dental health revealed a considerable change in caries findings; the mean number of decayed teeth (DT) decreased from 2.5 in 1980 to 0.8 in 2000 [Citation20], which may, however, be a weak projection of the need for restorative treatment. Notably, in northern Finland, half of patients aged 45 years had a restorative treatment need according to a cohort study with 2000 patients [Citation22]. A much lower need for restorative treatment has been reported in Canada, where 6.9% of patients had a restorative treatment need according to a cross-sectional epidemiological clinical investigation involving nearly 6000 participants [Citation23]; nearly 20% of participants were under 20 years of age, but the difference is still considerable. In Finland, 1.49 million restorative procedures were performed, 1.22 million (65%) of which were for 18- to 64-year-olds, at PDS in 2009 [Citation7], but there was no information on reasons for restoration. Nevertheless, according to the latest clinical recommendations for caries treatment, direct restoration should be done with minimal intervention techniques [Citation13,Citation24,Citation25], which may lead to one-surface restorations more often.
Number of restorations provided per patient
The mean number of restorations received per patient was 1.1 in 2012 and 0.9 in 2017. These figures are smaller than in the recent research from Finland in the private sector, where approximately one million adult patients aged 20 years and older received on average 1.42 restorations per patient in 2017 [Citation16]. In line with this, nearly 2000 patients aged about 45 years had a mean of 1.4 teeth needing restorative treatment in northern Finland [Citation22]. In contrast, significantly lower numbers of restorative procedures were published in USA; based on insurance claims, approximately 0.8 restorations were placed for adults in 2007 [Citation26], and in Australia, 0.7–0.8 restoration procedures per dental visit [Citation9]. According to a study based on public insurance database from Ireland, 1.7 restorations per patient in 1997 had declined to 1.2 restorations in 2008 [Citation11].
In our study, mean values of DMFT were in each same-age group smaller in 2017 than in 2012; the differences were most prominent from the age of 40 years onwards. These changes indicate improvement in dental health, but do not correspond to the volume of restoration procedures. An earlier study from Helsinki City PDS reported that replacement or repair of restorations accounted for 10% of all procedures among under 20-year-olds and 59% among those aged over 36 years, showing that replacements of restoration are strongly age-dependent [Citation27]. These replacements and repairs notably have no influence on DMFT-indices. Together with the large volume of restoration procedures in our study, moderate mean DMFT change in same-age groups can imply repair of initial restoration instead of treatment of new primary caries lesions. According to a recent comparison of the European indices of caries prevalence (DMFT), there is significantly more ‘F’ (filled) teeth in Finland than in other European countries [Citation28]. Generally, between-country comparison of oral health care services is difficult due to differences in coding systems and health care policies, but it reasonable to state that restorative procedures in permanent dentition are common in both PDS and the private sector in Finland.
Enhanced preventive measures
Targeting preventive treatment to restoration patients decreased from 7.9% in 2012 to 5.0% in 2017. This is in line with five other PDS units in southern Finland, where preventive measures accounted for 3.9% of all treatment measures in 2001–2013 and the actual quantity of preventive measures showed a 4.9% decrease across the 12 years; preventive treatment measures were 42 per 100 patients in 2001 and 13 per 100 patients in 2013 [Citation12]. These numbers are consistent with our results showing a decreasing trend in enhanced prevention procedures: 11.1 per 100 patients in 2012 and 5.8 per 100 patients in 2017. At the PDS in the city of Espoo, the low users of dental services had as many preventive measures as the heavy users [Citation29]. Linden et al. [Citation12] also found that preventive treatment procedures were not equally distributed in patients with low treatment need and those with need of restorative treatment at PDS in Finland. In the private sector in Finland in 2017, preventive measures provided to adults were rare accounting only for 2.3% of all treatment measures [Citation8]. Unfortunately, aggregated data in our study do not enable comparisons with caries risk groups or treatment needs; the reasons underlying the discrepancies between restorative procedures and preventive measures warrant further research.
An international expert group suggests a fluoride varnish every 3–6 months for caries risk patients [Citation25]. Scientific literature on the effect of the caries prevention used at the dental office for adult patients and its cost-effectiveness is scarce [Citation30]. According to Moller et al. [Citation31], however, patients with preventive dental care appointments had fewer operative dental visits in USA. In comparison with the early 2000s and the situation in Finland, higher levels of diagnostic and preventive treatments have been recently reported in Ireland and in Australia [Citation11,Citation32], but between-country comparison of preventive measures is especially difficult because of ways of recording all or only selected preventive measures.
Pulp capping
At Helsinki City PDS, a clear decrease in the volume of pulp cappings was seen in all same-age groups and age cohorts between 2012 and 2017. In the private sector in Finland, this same decreasing trend was shown in all age cohorts, the overall decrease being 26.2% across 5 years [Citation15]. The contemporary recommendation for treatment of deep caries lesion being partial caries removal or stepwise excavation [Citation13] together with the rising numbers of remaining teeth in the ageing population should cause an escalation in these treatment procedures. Since the opposite has occurred, the reasons for the declining trend can only be speculated. At Helsinki PDS, the code for pulp capping has been used for stepwise excavation as well as for direct or indirect pulp capping. Dentists may not be familiar with the current care guidelines, there might be a gap or delay before the guidelines reach them, or the incentive paid for pulp capping, stepwise excavation and preventive treatment may be negligible relative to the incentive paid for direct restorations or root canal treatment.
Strengths and limitations
The main strength of the study is that the data include all patients visiting Helsinki City PDS in the two years 2012 and 2017; a 5-year interval was selected to obtain an interval sufficiently long to demonstrate changes in practices, if any. Patients in same-age groups and age cohorts belong to different 5-year age groups, and therefore, comparisons between same-age groups and age cohorts are valid. In addition, our study includes a variety of descriptions and indicators used to assess the reality of restorative and preventive treatments in a selected population. Dentists were not aware of the forthcoming evaluation of recordings, and in electronic patient files the treatment codes are linked to paid incentives, strengthening the reliability of data.
Generally, literature on the numbers of restorative treatment has utilized individual data on patients or teeth or surfaces, forming the level where clinical actions take place. Our macro-level data (here: age groups) combined such information from lower-level observations (here: patients), thus being exposed to a potential aggregation bias when analysing the data and interpreting the results. Accordingly, the present findings should not lead to suggestions that assumed relationships at an aggregated level also apply at an individual level.
Conclusion
In conclusion, at Helsinki City PDS the magnitude of restorative treatment decreased slowly from 2012 to 2017 and overall enhanced preventive treatment was limited. The volume of direct restorative procedures and enhanced prevention measures revealed strong age-dependence. Restorative treatment procedures were more frequent in older than in younger age groups, while enhanced prevention and pulp cappings were more frequent in younger than in older age groups. A worrisome finding was the outstanding decrease in the share of enhanced preventive treatment in each same-age group as well as in each age cohort. Within the limitations of this study, we conclude that restorative and preventive treatments at Helsinki City PDS should be studied further and include more precise oral health status and dentist’s background information in the future.
Ethical approval
Study approval statement: The City of Helsinki Department of Social Services and Healthcare approved the study protocol. No ethics approval was needed because the data are a register-based entity with no connection to an individual patient’s identity.
Author contributions
UP contributed to conception, design, interpretation and drafted the manuscript. MMV contributed to conception, design, data acquisition and analysis, and critically revised the manuscript. SV contributed to conception, design and critically revised the manuscript. All the authors gave final approval and agree to be accountable for all aspects of the work.
Acknowledgement
The authors thank Tuomo Maisala from the City of Helsinki Department of Social Services and Healthcare, Helsinki, Finland, for gathering the data for our study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data that support the findings of this study are available from The City of Helsinki Department of Social Services and Healthcare. Restrictions apply to the availability of these data, which were used under licence for this study. Such dataset may be requested from The City of Helsinki Department of Social Services and Healthcare.
Additional information
Funding
References
- Staxrud F, Tveit AB, Rukke HV, et al. Repair of defective composite restorations. A questionnaire study among dentists in the Public Dental Service in Norway. J Dent. 2016;52:50–54.
- da Silva Tagliaferro EP, da Silva SRC, Rosell FL, et al. Methods for caries prevention in adults among dentists from a Brazilian community: adult' caries prevention among Brazilian dentists. Braz J Oral Sci. 2020;19:e206624.
- Maillet C, Decup F, Dantony E, et al. Selected and simplified FDI criteria for assessment of restorations. J Dent. 2022;122:104109.
- Jordan RA, Krois J, Schiffner U, et al. Trends in caries experience in the permanent dentition in Germany 1997-2014, and projection to 2030: morbidity shifts in an aging society. Sci Rep. 2019;9(1):5534.
- Edman K, Öhrn K, Nordström B, et al. Prevalence of dental caries and influencing factors, time trends over a 30-year period in an adult population. Epidemiological studies between 1983 and 2013 in the county of Dalarna, Sweden. Acta Odontol Scand. 2016;74(5):385–392. Jul
- Holtfreter B, Berg MH, Kocher T, et al. Change in FS-T index in adults in the German national oral health surveys between 1989 and 2005. Community Dent Oral Epidemiol. 2013;41(3):251–260.
- Widström E, Linden J, Tiira H, et al. Treatment provided in the Public Dental Service in Finland in 2009. Community Dent Health. 2015;32(1):60–64. Mar
- Vehkalahti M. Regional differences in subsidized private dental care in Finland in 2006–2017. Finnish Dent J. 2018;25(14):22–30.
- Oral health and dental care in Australia: key facts and figures 2015. Canberra: Australian Institute of Health and Welfare; 2016 [cited 2022 May 2]. Available from: https://apo.org.au/node/61181
- Manski RJ, Brown E. Dental Procedures, United States, 1999 and 2009. MEPS statistical brief: Agency for Healthcare Research and Quality; 2012.
- Guiney H, Felicia P, Whelton H, et al. Analysis of a payments database reveals trends in dental treatment provision. J Dent Res. 2013;92(7 Suppl):63S–69S.
- Linden J, Widström E, Sinkkonen J. Adults' dental treatment in 2001-2013 in Finnish public dental service. BMC Oral Health. 2020;20(1):121.
- Schwendicke F, Frencken JE, Bjørndal L, et al. Managing carious lesions: consensus recommendations on carious tissue removal. Adv Dent Res. 2016;28(2):58–67.
- Caries management. Current care guidelines. Working group set up by the Finnish Medical Society Duodecim and the Finnish Cardiac Society. Helsinki: The Finnish Medical Society Duodecim; 2020 [cited 2022 Jan 8]. Available from: www.kaypahoito.fi
- Vehkalahti MM, Palotie U, Valaste M. Age-specific findings on endodontic treatments performed by private dentists in Finland in 2012 and 2017: a nationwide register-based observation. Int Endod J. 2020;53(6):754–763.
- Vehkalahti MM, Palotie U, Valaste M. Age-related variation in volume and content of restorative private dental care for adults in Finland in 2012-2017: a nationwide register-based observation. J Dent. 2021;104:103537.
- Widström E, Linden J. Treatment provided in the public dental service and by private dentists in Finland. Oral Health Dent Manage. 2018;17(3):1–6.
- Suominen AL, Helminen S, Lahti S, et al. Use of oral health care services in Finnish adults - results from the cross-sectional health 2000 and 2011 surveys. BMC Oral Health. 2017;17(1):78. Apr 24
- Kopperud SE, Staxrud F, Espelid I, et al. The post-amalgam era: Norwegian dentists’ experiences with composite resins and repair of defective amalgam restorations. IJERPH. 2016;13(4):441.
- Vehkalahti M. Changes in oral health and health behaviour 1980-2000. In: Suominen-Taipale L, Nordblad A, Vehkalahti M, editors. Oral health in the Finnish adult population. Health 2000 survey. Publications of the National Public Health Institute, B25. Helsinki: Hakapaino Oy; 2008. p. 73–91 [cited 2022 Jan 13]. Available from: https://www.julkari.fi/bitstream/handle/10024/103030/2008b25.pdf
- Suominen AL, Varsio S, Helminen S, et al. Dental and periodontal health in Finnish adults in 2000 and 2011. Acta Odontol Scand. 2018;76(5):305–313.
- Laajala A, Karhatsu P, Pesonen P, et al. Association of indirect restorations with past caries history and present need for restorative treatment in the Northern Finland Birth Cohort 1966. Clin Oral Invest. 2018;22(3):1495–1501.
- Ramraj C, Azarpazhooh A, Dempster L, et al. Dental treatment needs in the Canadian population: analysis of a nationwide cross-sectional survey. BMC Oral Health. 2012;12:46.
- Momoi Y, Hayashi M, Fujitani M, et al. Clinical guidelines for treating caries in adults following a minimal intervention policy-evidence and consensus based report. J Dent. 2012;40(2):95–105.
- Martignon S, Pitts NB, Goffin G, et al. CariesCare practice guide: consensus on evidence into practice. Br Dent J. 2019;227(5):353–362.
- Eklund SA. Trends in dental treatment, 1992 to 2007. J Am Dent Assoc. 2010;141(4):391–399.
- Palotie U, Vehkalahti M. Restorative treatment and use of local anesthesia in free and subsidized public dental services in Helsinki, Finland. Acta Odontol Scand. 2003; 61(4):252–256.
- Carvalho JC, Schiffner U. Dental caries in European Adults and Senior Citizens 1996-2016: ORCA Saturday Afternoon Symposium in Greifswald, Germany - Part II. Caries Res. 2019;53(3):242–252.
- Nihtilä A, Widström E, Elonheimo O. Adult heavy and low users of dental services: treatment provided. Swed Dent J. 2016;40(1):21–32.
- Fontana M, Gonzalez-Cabezas C. Evidence-based dentistry caries risk assessment and disease management. Dent Clin North Am. 2019;63(1):119–128.
- Moeller JF, Chen H, Manski RJ. Investing in preventive dental care for the Medicare population: a preliminary analysis. Am J Public Health. 2010;100(11):2262–2269.
- Brennan DS, Chrisopoulos S, Luzzi L, et al. Dental services provided by dentists in Australia. Aust Dent J. 2020;65(1):90–95.
