Abstract
Objective
To study the influence of demographic and organizational factors to antibiotic utilization in dental implant surgery in Sweden.
Material and methods
Descriptive statistics regarding antibiotic prescription between 2009 and 2019 was retrieved from two national registers, the Swedish Prescribed Drug Register and the Dental Health register, both administered by the National Board of Health and Welfare.
Results
During the years 2009–2019 a significant decrease of the proportion of prescriptions of systemic antibiotics in conjunction with implant surgical procedures occurred in all patient groups where the most common procedure was the insertion of a single implant. The proportion of dental visits when implant surgical treatment was performed which resulted in a prescription of antibiotics decreased significantly from 1/3 to approximately 1/5. However, comparing Public and Private dental care providers, the reduction was significantly greater in Public dental care. Patients with low level of education in urban regions, treated in Private dental clinics were more likely to receive antibiotics in conjunction to implant surgery compared to other groups. Phenoxymethylpenicillin is the most widely used substance in conjunction with implant surgery.
Conclusion
There is still room for improvement in reduction of antibiotic prescriptions in conjunction to implant surgical procedures in Sweden.
Introduction
The rehabilitation of lost teeth using dental implantation is today a predictable treatment showing favourable long-term success rates [Citation1–4]. As a result, the global market for dental implants during the past 20 years has increased steadily and its market size was 2019 valued to 4.6 billion US$. By 2023, it is expected to have reached to about 13 billion US$ [Citation5]. Together with an ageing population with longer life expectancy, surgical implant interventions will most likely continue to increase.
Since there are still controversial views on the benefits of perioperative antibiotics/antibiotic prophylaxis in implant surgery, national recommendations in many countries are still missing or do not include a clear policy on the use of antibiotics during implant surgical interventions in otherwise healthy patients. Despite the publication of a large number of systematic reviews clinical guidelines that differentiate between cases and treatments are still missing [Citation6–13].
Attitudes and prescription habits in the use of antibiotics among dentists performing implant surgery has in recent years been published showing that the use of a single dose of preoperative amoxicillin is the most common intervention although great differences in dosage, compound and duration of treatment has been found. Although extended prophylaxis beyond the day of surgery in uncompromized/uncomplicated cases is considered an outdated approach recent studies show that this behaviour still is not uncommon [Citation14–16]. Since implant surgery will continue to grow it is likely to assume that the contribution of antibiotics prescribed by dentists in outpatient care will increase. Therefore, solid guidelines which in many countries are missing must be regarded as a major tool in the objective to optimize the use of antibiotics in dentistry including implant surgical procedures.
Today the correlation between antibiotic consumption and the increasing global development of antibiotic microbial resistance (AMR) is undisputed with serious consequences in medicine as well as in dentistry [Citation17,Citation18]. To counteract this development a global action plan has been adopted by the World Health Organization in which one of the most important objectives is to optimize the use of antimicrobial medicines in humans [Citation19].
In Sweden, a dental section of the Swedish strategic program against antibiotic resistance (STRAMA) was formed in 2007 (STRAMA Dent). In 2011, The Swedish Medical Products Agency together with The Swedish Institute of Communicable Disease Control was given the assignment to prepare national recommendations of the use of antibiotics in dentistry.
This action resulted in the publication of national recommendations of both antibiotic prophylaxis (2012), [Citation20] and treatment of dental infections (2014) [Citation21].
In Sweden, the sales of antibiotics in dentistry have decreased for several years and have been reduced by half from 2007. In 2019, Swedish dentists has been shown to account for around 6% of all antibiotics prescribed in outpatient care [Citation22]. These positive trends are most likely due to governmental actions taken during the years 2009–2017 although significant differences can still be found in antibiotic prescriptions comparing geographic regions, gender, and age among patients [Citation23].
Since antibiotic prescription by dentists in connection with implant surgery may be a notable part of the dentists' contribution in total antibiotic consumption and differentiated clear clinical guidelines are still missing, this area may show room for further improvement in the reduction of antibiotic utilization.
The aim of the present register-based study was thus to evaluate factors associated with the utilization of antibiotics in dental implant surgery in Sweden.
Material and methods
Ethical considerations
Prior to beginning the study an approval was obtained from the regional ethical committee (ref 2018/1616-31/2) and complemented with an extension of the time period up to 2019 (ref 2021/01056).
Registers and study population
Data for the study derived from two Swedish national registers, the Swedish Prescribed Drug Register (SPDR) and the Swedish Dental Health Register (SDHR), both administered by the Swedish National Board of Health and Welfare in accordance with the law on health data registers (1998:543). Part of the data has been summarized in a report from The Swedish National Board of Health and Welfare composed by one of the authors (F.L.) and the other authors acting as external experts in the report (B.L., M.H. and A.C.) [Citation24].
Accordingly, SPDR hold a national register of all prescribed pharmaceutical compounds, and which are retrieved by patients from the pharmacies in Sweden since 2005 [Citation25,Citation26]. Each dispatched and from the health and/or dental care prescribed medication is registered. As of such, the non-retrieved prescriptions are not included in the statistics. Furthermore, medical products/compounds directly given to the patients seeking health care on site are not registered/covered by the SPDR. However, by Swedish regulation this accounts for a minimal amount of the total medication consumed. Data on all prescriptions by dentists from the period 2009 to 2019 regarding antibiotic agents, date of subscription, type of compound, dosage and duration were collected.
The SDHR started in 2008 and include all dental care subsided by public means. The register hereby accounts for more than 95% of the dental care given to the adult Swedish population [Citation27]. Since dental care given to children and adolescents is not included in the SDHR register the data collected for this study include all dental care registered for adults/individuals above 24 years of age during the study period (2009–2019). All treatments in SDHR are coded which connect the diagnosis and type of treatment to the economical subsidising system. This coding system was used to enable statistics to be performed on treatments with increased likelihood of being accompanied with an antibiotic prescription. Consequently, visits regarding any type of dental treatment during the period 2009 to 2019 were selected for the analyses. For the purpose of evaluating antibiotic prescriptions in conjunction with surgical implant treatments, procedure codes that identified any type of such implant surgical treatment given were selected during the study period.
Statistical analyses
Descriptive statistics have been performed, using the software SAS Enterprise Guide 7.1 (SAS Institute, Cary, NC). Non-standardized proportions were compared using t score test. Statistical significance was set at a p-value level of .05 in all analyses.
Age standardization was applied to alleviate the comparison between different regions and years, by eliminating the differences depending on inequalities in age distribution. Direct age standardization was calculated based on the total population in Sweden 2019.
Results
Demographic data
The total number of individuals who received surgical insertion of at least one dental implant increased significantly with more than 100% during the study period between the years 2009–2019 (). The proportional increase of implant surgical procedures was greatest among the group of 24–49 years where a more than 6-fold increase in the number of treated patients was seen during the study period. In total 37,633 individuals received installation of at least one dental implant in 2019 compared to 15,657 in 2009 with the majority of individuals treated among the 50–69 years of age. The most common treatment procedure among individuals in all age categories was the insertion of a single implant. In 2019, 26,530 single implant procedures were performed compared to 1254 in 2009 (). Notably, it was found that the number of procedures with the insertion of >4 implants had decreased during the study period (−19%) and was more pronounced in the age category of 50–69 years of age ().
Table 1. Demographic data. Number of individuals from 24 years and above in three age categories treated with the insertion of at least one dental implant during the study period 2009–2019. Data collected from the Swedish Dental Health Register (SDHR) where all dental procedures are coded which connect the diagnosis and/or type of treatment to the economical subsidising system.
Table 2. Number of treatment procedures among individuals from 24 years of age and above in different age categories during the study period 2009–2019 according to Swedish Dental Health Register (SDHR). Data from each treatment category; insertion of a single implant (SI), insertion of 2–3 implants (2–3), insertion of ≥4 implants is presented.
Antibiotic prescription in conjunction with surgical implant procedures
All data were analyzed to evaluate the influence of age, gender, type of caregiver (public or private) and educational level of individuals in the study population on the proportion of prescriptions of antibiotics dispensed at implant surgical treatment visits registered in SDHR and SPDR. Data was further evaluated after dividing the dispensed prescriptions according to geographic residence of individuals in the study population in relation to regional level of urbanization (i.e. big city, city town, small town, and rural area). The distribution of the major compounds of antibiotics used during the study period was also assessed.
Influence of age and gender
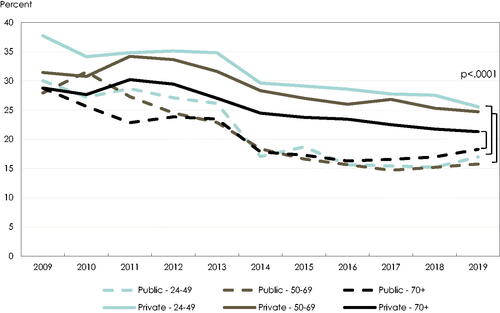
During the years 2009–2019 a significant decrease of the proportion of prescriptions of systemic antibiotics in conjunction with implant surgical procedures has occurred in the study population in all three age categories: 24–49 years (−12 percentage points), 50–69 years (−8 percentage points) and ≥70 years (−8 percentage points), (). The development in older age (≥70 years of age) was also evaluated by dividing the study population into six age groups (). These data showed that the greatest reduction of antibiotic prescriptions when implant surgical procedures was performed was found between the years 2013 to 2014 in all age categories except for the oldest age group of ≥80 years where this decrease (−17,5%) was seen already 2012–2013. The greatest proportional decrease in antibiotic prescriptions dispensed of 26,5% was seen among the group of 40–49 years of age between 2013–2014.
Figure 1. Proportion (%) of implant surgical treatment visits when an antibiotic prescription was despatched by the treating dentist registered in the Swedish Dental Health Register (SDHR) and the Swedish Prescribed Drug Register (SPDR) during the study period 2009–2019 in three different age categories. Source: the Swedish Dental Health Register and the Swedish Prescribed Drug Register.
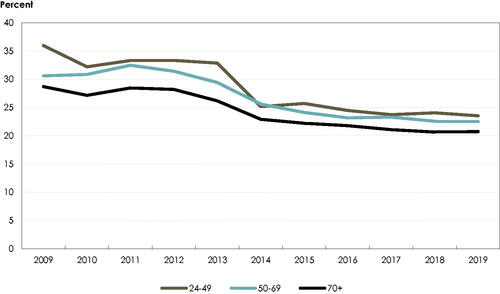
Table 3. Proportional (%) reduction in each year of the study period 2009–2019 of antibiotic prescriptions dispatched at visits to dental clinics when surgical implant treatment was performed. Individuals divided into six age categories to clearly illustrate change in older age (70–79 and 80+).
During the study period there was no significant difference in number of antibiotic prescriptions between men and women in combination with dental implant surgical procedures. The proportion of dental visits when implant surgical treatment was performed which resulted in a concomitant prescription of antibiotics decreased significantly in all age groups from 1/3 to approximately 1/5 ().
Influence of type of care giver (public or private)
When data of number of dispensed prescriptions of antibiotics at an implant surgical visit were compared between the two major categories of dental care providers in Sweden; Public and Private dental clinics, some major differences in the development during the 10 years could be observed. Although a major decrease in prescription rate in all age categories in both Public and Private dental care occurred between the years 2013–2014, the reduction was greater in Public dental care which resulted in a greater difference between the two types of caregivers than before. In 2019 the proportion slightly increased for Public dental care but there was still a significant difference compared to Private dental care, for all age categories (p < 0001). The difference between caregivers were most pronounced among the age group of 24–49 years in the year of 2014. Then the proportion of antibiotic prescription in Public dental care, for that age group, was 12 percentage points lower compared to the same age group in Private dental care. At the end of the study period, in 2019, there was still a difference of 9% points. Approximately 17% of implant surgical visits in the Public dental care among the age group of 24–49 years rendered an antibiotic prescription in 2019 compared to 26% in the Privat dental care. Throughout the entire study period individuals in the age group 24–49 years of age were more often given antibiotics in the Privat dental care compared with individuals in all age groups in Public dental care ().
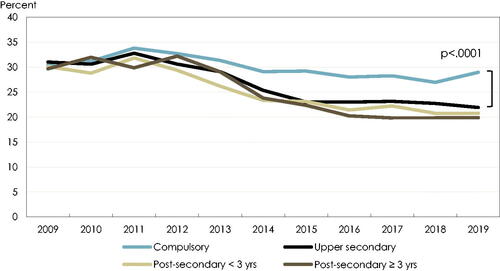
Influence of educational level
There was a difference of having antibiotics prescribed at an implant surgical visit by the treating dentist regarding the individual's level of education when the level of education was evaluated by dividing the population into four categories: compulsory/upper secondary/post-secondary <3 years, post-secondary >3 years. This difference was most pronounced among the age group of 50–69 years (). Although, a decrease was seen among the 50–69 years for all educational groups in 2014 the number of prescriptions among individuals with the lowest level of education (pre-secondary school) in conjunction with dental implant procedures did not decrease as much as the other educational groups. In 2019, the proportion with antibiotic prescriptions was significantly higher among individuals with the lowest level of education. Among the 50–69 years with compulsory level of education (lowest) 29% of the implant surgical visits was accompanied with a prescription of antibiotics compared to 20% of the visits for the individuals with the post-secondary >3 years level of education (highest).
Figure 3. Proportion (%) of implant surgical treatment visits when an antibiotic prescription was despatched by the treating dentist among individuals in the age group 50–69 years of age divided into four educational levels (compulsory/upper secondary/post-secondary <3 years, post-secondary >3 years).
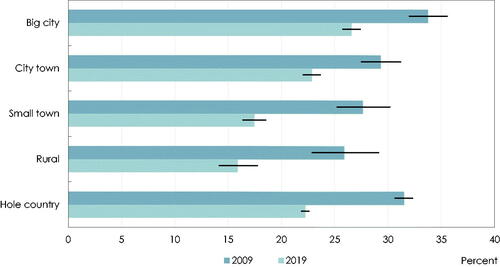
Influence of individuals residence in relation to level of urbanization
It was shown that it was more likely that antibiotics was prescribed at an implant surgical visit for patients living in a big city or in a city town when individuals residence was evaluated in relation to level of urbanization in Sweden (i.e. big city, city town, smaller town, and rural area). Although a substantial decline of antibiotic prescriptions in conjunction to implant surgical procedures has occurred in all geographic areas the total prescription is substantially higher for individuals treated in urban areas compared to rural regions ().
Distribution of major antibiotic compounds used during 2009–2019
The major antibiotic compounds prescribed at a visit to a dental clinic in association with implant surgical procedures were in declining order both in 2009 and in 2019; phenoxymethylpenicillin, amoxicillin, clindamycin, metronidazole, and tetracycline (). A significant proportional decrease in prescriptions was seen for phenoxymethylpenicillin, clindamycin and tetracycline together with a significant increase of prescriptions of amoxicillin and metronidazole during the study period (). Amoxicillin is the only compound showing an increase proportion throughout the study period. Between 2009 and 2019 the proportion of implant surgical procedures with amoxicillin prescribed to the patient increased with 43%. Although the proportional decrease of prescription of phenoxymethylpenicillin of 39% occurred during the study period this was still the most frequently used compound in conjunction to implant surgical procedures ().
Figure 5. Proportion (%) of implant surgical treatment visits when an antibiotic prescription was despatched by the treating dentist. Distribution of different antibiotic compounds during the study period 2009–2019 (data age standardized).
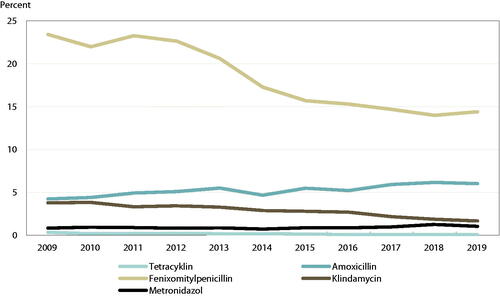
Table 4. Proportional distribution of prescriptions of antibiotic compounds per 1000 dental visits (n) in conjunction with implant surgical procedures (age-standardized data).
Discussion
The results of this study suggest that the publication of Swedish national recommendations of antibiotic prophylaxis in dentistry most likely have had an important impact on the reduction of peri-operative antibiotic prescriptions in conjunction with implant surgical procedures. The decrease follows a similar pattern as the general reduction of antibiotics in dentistry in Sweden seen during the past decade which most likely can be attributed to the governmental strategies implemented during the same period [Citation22,Citation23]. The major decrease of antibiotic prescriptions in conjunction with implant surgery which was seen in 2013–2014 also support the effect of the publication of the Swedish national recommendations on the use of antibiotic prophylaxis in dentistry in 2012 [Citation20].
An interesting observation in the present study was the finding that there was a significant difference in the proportional reduction of number of antibiotic prescriptions in conjunction with implant surgical procedures comparing Public dental clinics and Private dental clinics. Although a decrease in 2013–2014 occurred in both Public and Private clinics the reduction seen in Public dental care was significantly greater and more streamlined during the following years 2014–2019. However, data in the present study, cannot explain the reason for this difference but merely speculate on possible causes. One plausible reason may be that Public dental clinics in Sweden are organized in the national regions into larger healthcare organizations (Folktandvården). As such there is a direct responsibility in the Public dental health care organizations to work with patient safety issues and quality management. Extensive resources have during the past decade been set aside in the Public health care organizations for continuous education of staff and to closely follow antibiotic prescription. Although similar educational efforts and quality management is found in larger private care companies, there is still a great number of clinics consisting of 1–2 dentists where the national recommendation may not be fully implemented. Several studies have shown that educational measures introduced parallel to the introduction of new recommendations are very important and have a significant effect in implementation and retention to clinical guidelines [Citation28,Citation29].
A limitation with our register-based study is that we have not been able to analyse prescribers' age and gender which of course also can influence prescription patterns. Since there are more younger dentists working in public dental care this may have affected the results. Older men working in private clinics may be more frequent antibiotic prescribers than younger women working in public clinics and as such less prone to follow recommendations. Unfortunately, this could not be analyzed in our register-based data.
In Sweden, clinics for specialist treatments are organized in the national regions in Public specialist clinics while Private specialist clinics mainly can be found in the metropolitan regions. For this reason, it may be assumed that most of the complex patients are treated within the specialist care in Public dental care in Sweden. Therefore, it is not likely that the higher rate of antibiotic prescriptions found in Private dental care is due to that the patients' degree of treatment complexity is higher in private care justifying the higher proportion of antibiotic prescriptions found in private care. As seen in general for antibiotics prescriptions dispatched by dentists in Sweden the proportion of prescriptions in conjunction to implant surgical treatment was higher in big cities and in city towns corresponding to the yearly reports on antibiotic prescription rates in dentistry [Citation22,Citation24].
An interesting observation was that individuals with a lower level of education more often received a prescription of antibiotics in conjunction to implant surgery than individuals with a higher education. This may be caused by a difference in general and or/oral health between the three educational categories evaluated. The correlation of oral health and general health to socioeconomic factors has been shown in several studies [Citation30,Citation31]. Since the number of intact teeth was lower among the individuals with the lowest degree of education this may indicate that general health and/or oral health was poorer among the individuals with the lowest level of education which may justify that a higher prescription of antibiotics was found among these patients.
Another observation in our study was that the use of phenoxymethylpenicillin still is the most widely used substance prescribed in conjunction with implant surgery. The recommendations in Sweden strongly promote that merely a single dose of antibiotic prophylaxis may be used if needed. The compound recommended is amoxicillin because of its more predictable absorption and longer half-life compared to phenoxymethylpenicillin.
Although the prescriptions of phenoxymethylpenicillin have declined considerably during the study period this finding shows that prolonged prophylaxis or longer antibiotic treatment during initial healing still is very common. Recent reviews have also questioned the benefit of antibiotic prophylaxis and/or extended treatment in uncomplicated implant surgery in otherwise healthy patients [Citation7,Citation32] which also have been confirmed in placebo-controlled studies [Citation33]. This finding shows that there is still room for improvement in reducing the rate of prescriptions of antibiotics in connection with implant surgery especially since a majority of treatments performed were placement of a single implant which in most cases are uncomplicated procedures compared to insertion of multiple implants. In order for recommendations to have viable legitimacy, regular audits and up-dates are needed based on latest scientific evidence and a multidisciplinary approach.
In conclusion, antibiotic prescription was generally common even though most of the implant procedures undertaken were insertion of a single implant. Patients with low level of education, in urban regions, treated in a private dental clinic were more likely to receive antibiotics in conjunction to dental implant surgery compared to other patient groups.
Consequently, the data support that there is room for improvement in the reduction of antibiotic prescriptions in conjunction to implant surgical procedures in Sweden
Author contributions
Conceptualisation: Margareta Hultin, Bodil Lund, Andreas Cederlund, Frida Lundgren; Methodology: Margareta Hultin, Bodil Lund, Andreas Cederlund, Frida Lundgren; Software: Andreas Cederlund, Frida Lundgren; Validation: Frida Lundgren; Formal analysis: Margareta Hultin, Frida Lundgren; Investigation: Margareta Hultin, Frida Lundgren; Data Curation: Frida Lundgren; Writing – original draft preparation: Margareta Hultin, Bodil Lund, Andreas Cederlund; Writing – review and editing: Margareta Hultin, Bodil Lund, Andreas Cederlund, Frida Lundgren; Visualisation: Margareta Hultin, Frida Lundgren; Supervision: Bodil Lund; Project administration: Margareta Hultin, Bodil Lund
Disclosure statement
The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this manuscript.
Additional information
Funding
References
- Buser D, Mericske-Stern R, Bernard JP, et al. Long-term evaluation of non-submerged ITI implants. Part 1: 8-year life table analysis of a prospective multi-center study with 2359 implants. Clin Oral Implants Res. 1997;8(3):161–172.
- Ekelund JA, Lindquist LW, Carlsson GE, et al. Implant treatment in the edentulous mandible: a prospective study on Brånemark system implants over more than 20 years. Int J Prosthodont. 2003;16(6):602–608.
- Lekholm U, Grondahl K, Jemt T. Outcome of oral implant treatment in partially edentulous jaws followed 20 years in clinical function. Clin Implant Dent Relat Res. 2006;8(4):178–186.
- Jemt T. Implant survival in the edentulous jaw: 30 years of experience. Part II: a retro-prospective multivariate regression analysis related to treated arch and implant surface roughness. Int J Prosthodont. 2018;31(6):531–539.
- Alghamdi HS, Jansen JA. The development and future of dental implants. Dent Mater J. 2020;39(2):167–172.
- Esposito M, Grusovin MG, Maghaireh H, et al. Interventions for replacing missing teeth: different times for loading dental implants. Cochrane Database Syst Rev. 2013;2013(3):Cd003878.
- Lund B, Hultin M, Tranaeus S, et al. Complex systematic review - perioperative antibiotics in conjunction with dental implant placement. Clin Oral Impl Res. 2015;26(Suppl11):1–14. År nr 11)
- Rodríguez Sánchez F, Rodríguez Andrés C, Arteagoitia I. Which antibiotic regimen prevents implant failure or infection after dental implant surgery? A systematic review and meta-analysis. J Craniomaxillofac Surg. 2018;46(4):722–736. Är med som nr 12)
- Braun RS, Chambrone L, Khouly I. Prophylactic antibiotic regimens in dental implant failure: a systematic review and meta-analysis. J Am Dent Assoc. 2019;150(6):e61–e91.
- Romandini M, De Tullio I, Congedi F, et al. Antibiotic prophylaxis at dental implant placement: which is the best protocol? A systematic review and network meta-analysis. J Clin Periodontol. 2019;46(3):382–395.
- Jain A, Rai A, Singh A, et al. Efficacy of preoperative antibiotics in prevention of dental implant failure: a meta-analysis of randomized controlled trials. Oral Maxillofac Surg. 2020;24(4):469–475.
- Canullo L, Troiano G, Sbricoli L, et al. The use of antibiotics in implant therapy: a systematic review and meta-analysis with trial sequential analysis on early implant failure. Int J Oral Maxillofac Implants. 2020;35(3):485–494.
- Roca-Millan E, Estrugo-Devesa A, Merlos A, et al. Systemic antibiotic prophylaxis to reduce early implant failure: a systematic review and meta-analysis. Antibiotics (Basel). 2021;10(6):698.
- Khalil D, Hultin M, Andersson Fred L, et al. Antibiotic prescription patterns among Swedish dentists working with dental implant surgery: adherence to recommendations. Clin Oral Impl Res. 2015;26(9):1064–1069.
- Rodríguez Sánchez F, Arteagoitia I, Rodríguez Andrés C, et al. Antibiotic prophylaxis prescribing habits in oral implant surgery in the Netherlands: a cross-sectional survey. BMC Oral Health. 2019;19(1):281. PMID: 31830979
- Aragoneses JM, Aragoneses J, Brugal VA, et al. Antimicrobial prescription habits of dentists performing dental implant treatments in Santo Domingo, Dominican Republic. Antibiotics (Basel). 2020;9(7):376. PMID: 32635270
- Clatworthy AE, Pierson E, Hung DT. Targeting virulence: a new paradigm for antimicrobial therapy. Nat Chem Biol. 2007;3(9):541–548.
- Livermore DM, Minimising antibiotic resistance. Lancet Infect Dis. 2005;5(7):450–459.
- WHO. 2015. Global Strategy for Containment of Antimicrobial Resistance. Geneva, Switzerland. http://www.who.int/drugresistance/WHO_Global_Strategy.pdf. World Health Organization 2015
- Allander A, Aronsson B, Baecklund E, et al. Indikationer för antibiotikaprofylax i tandvården. (publication in Swedish). Info Läkemedelsverket. 2012;5:22–35.
- Skogh Andrén A, Aronsson B, Aust-Kettis A, et al. Rekommendationer för antibiotikabehandling i tandvården. (publication in Swedish). Info Läkemedelsverket. 2014;25:19–30.
- Swedres-Svarm 2019. Sales of antibiotics and occurrence of resistance in Sweden. Solna/Uppsala ISSN1650-6332. Available from: https://www.folkhalsomyndigheten.se/contentassets/fb80663bc7c94d678be785e3360917d1/swedres-svarm-2019.pdf.
- Lund B, Cederlund A, Hultin M, et al. Effect of governmental strategies on antibiotic prescription in dentistry. Acta Odontol Scand. 2020;78(7):529–534.
- Antibiotikaförskrivning inom tandvården. Statistikrapport baserad på uppgifter från läkemedels- och tandhälsoregistret 2009-2017. Socialstyrelsen 2019. https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/statistik/2019-4-14.pdf.
- Wettermark B, Hammar N, Fored CM, et al. The new swedish prescribed drug register–opportunities for pharmacoepidemiological research and experience from the first six months. Pharmacoepidemiol Drug Saf. 2007;16(7):726–735.
- Ludvigsson JF, Almqvist C, Bonamy A-KE, et al. Registers of the Swedish total population and their use in medical research. Eur J Epidemiol. 2016;31(2):125–136.
- Ljung R, Lundgren F, Appelquist M, et al. The swedish dental health register - validation study of remaining and intact teeth. BMC Oral Health. 2019;19(1):116.
- Gjelstad S, Høye S, Straand J, et al. Improving antibiotic prescribing in acute respiratory tract infections: cluster randomised trial from Norwegian general practice (prescription peer academic detailing (Rx-PAD) study). BMJ. 2013;347:f4403.
- Ferrat E, Le Breton J, Guéry E, et al. Effects 4.5 years after an interactive GP educational seminar on antibiotic therapy for respiratory tract infections: a randomized controlled trial. FAMPRJ. 2016;33(2):192–199.
- Hakeberg M, Wide Boman U. Self-reported oral and general health in relation to socioeconomic position. BMC Public Health. 2017;18(1):63.
- Dörfer C, Benz C, Aida J, et al. The relationship of oral health with general health and NCDs: a brief review. Int Dent J. 2017;67(Suppl 2):14–18.
- Bernabeu-Mira JC, Peñarrocha-Diago M, Peñarrocha-Oltra D. Prescription of antibiotic prophylaxis for dental implant surgery in healthy patients: a systematic review of survey-based studies. Front Pharmacol. 2020;11:588333.
- Momand P, Becktor JP, Naimi-Akbar A, et al. Effect of antibiotic prophylaxis in dental implant surgery: a multicenter placebo-controlled double-blinded randomized clinical trial. Clin Implant Dent Relat Res. 2022;24(1):116–124.