Abstract
Objective
The aetiology of gingival recessions is not fully understood, and no evidence has yet emerged of a single predisposing factor that instigates this apical shift of the gingival margin. Nonetheless, both fixed retainers and orthodontic treatment have been cited as potential risk factors. The aim of this study was to assess the effects of orthodontic treatment and orthodontic fixed retainers on gingival recessions.
Subjects and methods
In total, 105 patients at the Department of Orthodontics at the University of Gothenburg who had undergone orthodontic treatment between 1995 − 2003 were included in this study. Intraoral photographs of the anterior segment and study casts acquired at baseline (pre-treatment), post-treatment and at the 10-year follow-up were used as recorded measurements of gingival recession and orthodontic treatment. At the 10-year follow-up, the patients were divided into two groups based on: long-term (10 years) presence of a fixed retainer [orthodontic treatment and retainer (OR) group; N = 76]; and short-term (<5 years) presence of a fixed retainer [orthodontic treatment (O) group; N = 57]. These groups were compared to a control group (C) of untreated subjects (N = 29).
Results
In the anterior segment, gingival recessions were not present at baseline and post-treatment between the two orthodontically treated groups. At the 10-year follow-up, there was no statistically significant difference between the two orthodontically treated groups and the controls.
Conclusions
Orthodontic treatment per se does not increase the risk for gingival recessions, nor does the use of fixed retainers following orthodontic treatment.
Introduction
Gingival recessions, which involve apical shifting of the gingival margin [Citation1], are common soft tissue defects that may cause a number of dental-related complications. These include increased risks for dentine hypersensitivity, root caries, and aesthetically related concerns [Citation2,Citation3]. The prevalence of gingival recessions is in the range of 7–40% [Citation4–7], and the severity of recessions has been shown to increase with age [Citation4–6].
While several aetiologic factors for gingival recession have been described in the literature, inappropriate tooth-brushing techniques along with tongue and lip piercings continue to be viewed as the most-frequent causative factors [Citation4,Citation8,Citation9]. Other risk factors of importance for gingival recessions include: periodontal disease, which may lead to a generalised apical dislocation of the gingival margin; overjets in combination with overbites; and orthodontic treatments [Citation10–12].
Orthodontic treatment is an effective clinical strategy to recover dental malfunctions and improve dental aesthetics. However, to preserve the obtained result, long-term retention is recommended after an orthodontic treatment. Commonly used retainers include: removable plates; positioners composed of flexible acrylic, and bonded retainers. Of these, bonded retainers have been widely used over the past decades.
Orthodontic treatment per se has been implicated as a risk factor for gingival recessions. This is related to the unfavourable forces generated by orthodontic appliances, which can move the tooth outside of the alveolar ridge and cause gingival recession [Citation11,Citation13]. In addition, although only studied to a limited extent, fixed retainers following orthodontic treatment have been discussed as a potential risk factor [Citation14–16].
There is an ongoing debate as to whether orthodontic treatment and/or fixed retainers can cause gingival recessions. Therefore, the aim was to determine whether orthodontic treatment causes gingival recession. Moreover, to determine whether retainers cause gingival recession, 10 years after orthodontic treatment.
Subjects and methods
Study design
This was a retrospective study carried out at the Department of Orthodontics, Institute of Odontology, The Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden. The medical records for patients who received orthodontic treatment in the period 1995 − 2003 were collected and analysed, with the aim of assessing the impact of orthodontic treatment on gingival recessions and the long-term effects of fixed orthodontic retainers on gingival recessions.
Subjects
The subjects comprised 105 (39 men and 66 women) patients from the Department of Orthodontics, Institute of Odontology, The Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden, who were followed up for 10 years after orthodontic treatment. The control subjects were 29 healthy dental students (9 men and 20 women) with no previous orthodontic treatment. The controls were matched for age and gender to the remaining 105 subjects who had undergone orthodontic treatment. The subjects who had undergone orthodontic treatment had to meet the following inclusion criteria: i) willing and able to provide informed signed consent; ii) previous orthodontic treatment with fixed appliances in both the upper-, and lower jaw; and iii) available intraoral images of the anterior segment, and study casts obtained at baseline (pre-treatment), post-treatment (after orthodontic treatment) and at the 10-year follow-up. Eligible subjects were divided into three groups: long-term (10 years with fixed retainer) following orthodontic treatment [OR group, N = 76]; short-term (<5 years with fixed retainer) following orthodontic treatment [O group; N = 57]; and control subjects with no previous orthodontic treatment [C group; N = 29]. Out of the 105 subjects, 28 were included in both the OR and O group. For the C group, baseline data were not available, thus only 10-year data are presented in .
Table 1. Baseline- and 10-year characteristics for C group.
In total, 98 upper-, and 127 lower jaws were analysed during the course of this study. These were further divided into the OR group, 26 upper-, and 71 lower jaws; O group, 43 upper-, and 27 lower jaws; and C group, 29 upper-, and 29 lower jaws. provides a full description of the baseline characteristics.
Instruments
A Vernier calliper (Mitutoyo 530-122 Kanagawa, Japan) with an accuracy of 0.2 mm was used to calibrate and measure the gingival recessions on the study casts. A dental software platform for images with measuring tools (Planmeca Romexis ver. 4.0) was used to measure the gingival recessions on the intraoral images, which had been captured with a system camera (Canon Powershot G7X).
Procedures and data collection
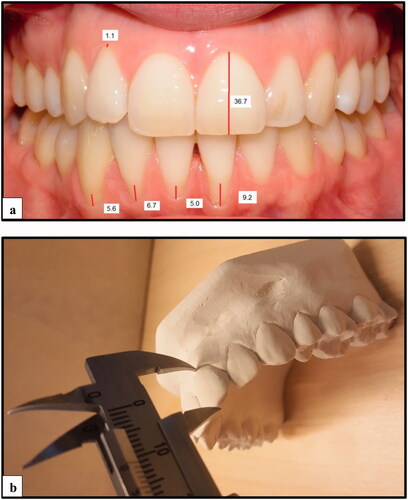
Patient records were screened for orthodontic treatments with fixed appliances and follow-up of fixed retainers in the period 1995 − 2003. For the control group, new study casts were prepared using alginate (Blueprint Xcreme) impressions with metallic trays. Intraoral images were acquired using a system camera (Canon Powershot G7X). Gingival recessions were measured in the anterior segment, i.e. canine to canine, for the upper-, and lower jaws respectively, using intraoral photographs of the anterior segment and study casts. Gingival recessions were measured in millimetres (mm) from the gingival margin on the mid-buccal surfaces to the cemento–enamel junction. The calibration of the intraoral photographs was done with the ratio of the mid-buccal length for tooth 21 from gingival margin to incisal edge measured on photograph and study cast, respectively.
The severity of each gingival recession was then calculated by multiplying this ratio with the length (mm) of the recession measured on the intraoral photograph, using Planmeca Romexis ver. 4.0 (,). This can be summarized as follows: gingival recession in the anterior segment = recession measured on photograph x (distance from gingival margin to incisal edge on model for tooth 21 ÷ distance from gingival margin to incisal edge on photograph for tooth 21) [Citation17]. Mean gingival recession was then calculated for each jaw by dividing the sum of the gingival recessions (canine to canine) by six. When the length of tooth 21 on the study casts were not appropriate for calibration, for reasons such as fractures or overhang, the width of the tooth 21 was used instead. All measurements were carried out by two blinded operators who had been previously calibrated on a subset of data to assure intra-examiner reliability (Dahlberg’s formula = 0.07 mm). The examiner measured tooth 21 in 20 randomly selected patients on 2 occasions 2 weeks apart. All collected data was continuously recorded in Microsoft Office Excel 2003 (Microsoft Corp., Redmond, WA, USA).
Statistical analyses
The sample size for each group was calculated based on a α-significance level = 0.01 and power = 0.9. The projected sample size needed to detect a clinically meaningful difference of 2 mm (SD ± 1 mm) was N = 30 (G*power ver. 3.1.9.4; University of Düsseldorf, Germany). Normal distribution was assessed using the Kolmogorov-Smirnov test. The data were analysed using the Kruskal–Wallis test by ranks, followed by Dunn’s post hoc test for multiple comparisons. A p-value ≤.05 was considered statistically significant. The analyses were conducted with the IBM SPSS Statistics ver. 25 software package (IBM Corp., Armonk, NY, USA).
Ethical considerations
Ethical approval for the study was obtained from the Research Ethical Board at the University of Gothenburg (Dnr. 290-09). All participants received information regarding the study, and informed written consent was obtained from all the participants.
Results
In total, 119 case records for orthodontically treated patients were identified during the course of this retrospective study. Following a systematic evaluation of the collected records, 14 out of the 119 included patients were excluded, and the remaining 105 patients along with 29 controls were carried forward for the statistical analyses. All the subjects (N = 134) were healthy, with no signs of periodontal disease or dental caries. provides a full description of the baseline characteristics of the subjects.
At baseline and post-treatment, when the two orthodontically treated groups (OR and O groups) were assessed, no gingival recessions were observed in the anterior segment of any of the jaws. No data were available at baseline and post-treatment for the C group ().
Table 2. Gingival recessions in the anterior segment (canine to canine) at baseline (pre-treatment), post-treatment (after an orthodontic treatment) and at the 10-year follow-up for the upper and lower jaws.
At the 10-year follow-up, when the anterior segment was assessed for the upper jaw, no gingival recession was observed in the OR group, whereas the O group and C group presented a mean gingival recession (mm; mean ± SD) of 0.1 ± 0.2. This difference did not reach statistical significance (). In addition, when the lower jaw was assessed for the anterior segment at the 10-year follow-up, all three groups presented a mean gingival recession (mm; mean ± SD) of 0.1 ± 0.2 ().
Discussion
Orthodontically treated teeth are at high risk of relapse within the first 2 years following orthodontic treatment. Since long-term orthodontic stability cannot be predicted, a fixed bonded retainer is commonly applied after the orthodontic treatment. Although it is frequently used, the impact of a retainer on the gingiva in the long-term is not fully understood. Furthermore, it has been proposed (albeit investigated to only a limited extent) that retainers and/or orthodontic treatment per se cause gingival recessions. This was the rationale for conducting this retrospective study.
Gingival recessions could not be found in the anterior segments of the upper-, and lower jaw at baseline and post-treatment in the OR group and O group. The absence of gingival recession may be explained by the young age of the subjects in our study, as the gingiva of younger patients seem to adapt better to orthodontic tooth movement compared to older patients [Citation18]. Furthermore, although one study has found that labial gingival recessions were more frequently found in orthodontically treated patients compared to non-treated patients [Citation19], such correlation was not found in this study which is in line with previous studies [Citation20,Citation21].
Our findings are further supported by another study which showed that there was no increased risk for developing gingival recessions in a five-year perspective after orthodontic treatment with-, and without proclination [Citation22].
However, contradictory statements can be found in the literature as gingival recessions have been observed in orthodontically treated monkeys to a greater extent as compared to non-treated controls [Citation13]. The same experimental study also investigated the reaction of the periodontal tissue during orthodontic tooth movement and suggested that plaque-induced inflammation, and the thickness of the gingiva were factors that also affected the development of gingival recessions [Citation13].
At the 10-year follow up, nonsignificant gingival recessions were observed in the anterior segments of the upper-, and lower jaw in OR group, O group and C group, respectively. This could be explained by normal ageing effects on gingiva since the prevalence and the severity increases with age [Citation4,Citation5]. These results are in line with one study that showed no detrimental effects on the mandibular anterior gingiva after having a bonded retainer for more than 20 years [Citation23]. Moreover, another study revealed minor differences in gingival recessions between orthodontically treated patients with and without fixed retention [Citation14].
The accumulation of plaque and poor dental hygiene have been observed in patients with long-term fixed retainers and have been proposed to exert negative effects on the periodontal tissues, resulting in gingival recessions [Citation15]. However, there are periodontal studies that have demonstrated that factors such as plaque and calculus accumulation are not automatically correlated with periodontal disease [Citation24–26]. Plaque and calculus were however not registered as part of this study, hence its potential impact on gingival recessions remains to be elucidated. Based on the above, it appears that the aetiology of this condition constitutes a complex interaction between several factors, and that orthodontic treatment and fixed retainer in themselves are not sufficient to predict the development of gingival recessions. For such reasons factors, e.g. plaque, calculus, abrasions, gingiva characteristics and type of orthodontic tooth movement are of importance to analyse in follow-up studies [Citation4,Citation27,Citation28].
This study has several strengths. First, the long follow-up time of 10 years post-treatment allowed us to analyse the long-term impact of a fixed retainer on gingival recessions. Second, the use of intraoral images and study casts provides accurate measurements of gingival recessions. Using both images and study casts of the width of the keratinised tissue is more reliable than using clinical measurements alone [Citation29], indicating the value of our method of registration. A limitation of this study that should be acknowledged is that the control group consisted of dental students with optimal oral hygiene [Citation4,Citation30], which may not be representative of the general population. In addition, the control group lacked baseline records, which meant that the assessment of potential gingival recessions over time was not possible for this group.
Conclusion
Orthodontic treatment per se and the use of fixed retainer does not increase the risk for gingival recessions. Prospective, randomised studies are needed to confirm these results.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Wennström J, Pini Prato G. Mucogingival therapy: periodontal plastic surgery. In Lindhe J, Karring T, Lang N, editors. Clinical periodontology and implant dentistry. 4th ed. Copenhagen: Munksgaard; 2008. p. 576–649.
- Teixeira DNR, Zeola LF, Machado AC, et al. Relationship between noncarious cervical lesions, cervical dentin hypersensitivity, gingival recession, and associated risk factors: a cross-sectional study. J Dent. 2018;76:93–97.
- Merijohn GK. Management and prevention of gingival recession. Periodontol. 2016;71(1):228–242.
- Serino G, Wennstrom JL, Lindhe J, et al. The prevalence and distribution of gingival recession in subjects with a high standard of oral hygiene. J Clin Periodontol. 1994;21(1):57–63.
- Albandar JM, Kingman A. Gingival recession, gingival bleeding, and dental calculus in adults 30 years of age and older in the United States, 1988–1994. J Periodontol. 1999;70(1):30–43.
- Loe H, Anerud A, Boysen H. The natural history of periodontal disease in man: prevalence, severity, and extent of gingival recession. J Periodontol. 1992;63(6):489–495.
- Khocht A, Simon G, Person P, et al. Gingival recession in relation to history of hard toothbrush use. J Periodontol. 1993;64(9):900–905.
- Plastargias I, Sakellari D. The consequences of tongue piercing on oral and periodontal tissues. ISRN Dent. 2014;2014:876510.
- Fukumoto Y, Horibe M, Inagaki Y, et al. Association of gingival recession and other factors with the presence of dentin hypersensitivity. Odontology. 2014;102(1):42–49.
- Bjornaas T, Rygh P, Boe OE. Severe overjet and overbite reduced alveolar bone height in 19-year-old men. Am J Orthod Dentofacial Orthop. 1994;106(2):139–145.
- Pernet F, Vento C, Pandis N, et al. Long-term evaluation of lower incisors gingival recessions after orthodontic treatment. Eur J Orthod. 2019;41(6):559–564.
- Bernhardt O, Krey KF, Daboul A, et al. New insights in the link between malocclusion and periodontal disease. J Clin Periodontol. 2019;46(2):144–159.
- Wennstrom JL, Lindhe J, Sinclair F, et al. Some periodontal tissue reactions to orthodontic tooth movement in monkeys. J Clin Periodontol. 1987;14(3):121–129.
- Levin L, Samorodnitzky-Naveh GR, Machtei EE. The association of orthodontic treatment and fixed retainers with gingival health. J Periodontol. 2008;79(11):2087–2092.
- Pandis N, Vlahopoulos K, Madianos P, et al. Long-term periodontal status of patients with mandibular lingual fixed retention. Eur J Orthod. 2007;29(5):471–476.
- Bin Bahar BSK, Alkhalidy SR, Kaklamanos EG, et al. Do orthodontic patients develop more gingival recession in anterior teeth compared to untreated individuals? A systematic review of controlled studies. Int Orthod. 2020;18(1):1–9.
- Morris JW, Campbell PM, Tadlock LP, et al. Prevalence of gingival recession after orthodontic tooth movements. Am J Orthod Dentofacial Orthop. 2017;151(5):851–859.
- Renkema AM, Fudalej PS, Renkema A, et al. Development of labial gingival recessions in orthodontically treated patients. Am J Orthod Dentofacial Orthop. 2013;143(2):206–212.
- Slutzkey S, Levin L. Gingival recession in young adults: occurrence, severity, and relationship to past orthodontic treatment and oral piercing. Am J Orthod Dentofacial Orthop. 2008;134(5):652–656.
- Djeu G, Hayes C, Zawaideh S. Correlation between mandibular Central incisor proclination and gingival recession during fixed appliance therapy. Angle Orthod. 2002;72:238–245.
- Artun J, Grobety D. Periodontal status of mandibular incisors after pronounced orthodontic advancement during adolescence: a follow-up evaluation. Am J Orthod Dentofacial Orthop. 2001;119(1):2–10.
- Renkema AM, Navratilova Z, Mazurova K, et al. Gingival labial recessions and the post-treatment proclination of mandibular incisors. EORTHO. 2015;37(5):508–513.
- Booth FA, Edelman JM, Proffit WR. Twenty-year follow-up of patients with permanently bonded mandibular canine-to-canine retainers. Am J Orthod Dentofacial Orthop. 2008;133(1):70–76.
- Kornman KS, Page RC, Tonetti MS. The host response to the microbial challenge in periodontitis: assembling the players. Periodontol 2000. 1997;14:33–53.
- Arn ML, Dritsas K, Pandis N, et al. The effects of fixed orthodontic retainers on periodontal health: a systematic review. Am J Orthod Dentofacial Orthop. 2020;157(2):156–164 e17.
- Ayilavarapu S. Fixed orthodontic retainers Do not seem to adversely affect periodontal health. J Evid Based Dent Pract. 2021;21(1):101522.
- Melsen B, Allais D. Factors of importance for the development of dehiscences during labial movement of mandibular incisors: a retrospective study of adult orthodontic patients. Am J Orthod Dentofacial Orthop. 2005;127(5):552–561.
- Rasperini G, Acunzo R, Cannalire P, et al. Influence of periodontal biotype on root surface exposure during orthodontic treatment: a preliminary study. Int J Periodontics Restorative Dent. 2015;35(5):665–675.
- Trentini CM, Moriarty JD, Phillips C, et al. Evaluation of the use of orthodontic records to measure the width of keratinized tissue. J Periodontol. 1995;66(6):438–442.
- Matas F, Sentis J, Mendieta C. Ten-year longitudinal study of gingival recession in dentists. J Clin Periodontol. 2011;38(12):1091–1098.