Abstract
Objective
Assess the association between oral and general health related quality of life using oral impacts on daily performances (OIDP) and the quality of life tool EQ-5D-5L from EuroQoL among patients with substance use disorder (SUD) who receive opioid agonist therapy.
Method
609 patients with SUD completed the EQ-5D-5L. A dental sub-study of 167 patients completed OIDP and an oral examination when attending outpatient clinics in Western Norway for their opioid agonist therapy. The merged analytical sample consisted of 165 patients. The association between OIDP and EQ-5D-5L was assessed by Spearman’s rho and a linear multiple variable regression analysis. A line graph and a Pen’s parade displayed the distributions of OIDP sum scores and EQ-5D-5L index values.
Results
Overall mean summary- and index EQ-5D-5L scores were 9.97 (sd 3.25) and 0.69 (sd 0.22). Mean score for OIDP was 9.75 (sd 9.59). Spearman’s rho was 0.34 (p < .01) between OIDP and EQ-5D-5L summary scores. Linear regression revealed an association adjusted for sex and age of 0.12 (95% CI 0.07–0.17) and a coefficient of determination of 0.1460.
Conclusion
This study reveals a strong association between OIDP and EQ-5D-5L reflecting the importance of oral health to general health for patients with SUD. Health care professionals should pay attention to oral health. Effective interventions might improve patients’ oral and health related quality of life.
Introduction
According to national and international studies, patients with substance use disorder (SUD) suffer from increased health risks, such as a higher burden of mental health disorders, lung diseases, chronic infections including human immunodeficiency virus (HIV), tuberculosis, hepatitis C and B, overdoses and related mortalities compared to the general population [Citation1]. Specific oral diseases in terms of tooth loss, progressive caries, and periodontal disease are also more commonly observed among SUD patients than in the general population [Citation2]. These sequelae might affect patients’ quality of life [Citation3,Citation4]. Thus, oral and general health related quality of life are important outcome measures in clinical and epidemiological research to complement clinical effectiveness and monitor the burden of disease. Besides numerous health and oral health related problems, poor lifestyle, low awareness of oral health and use of dental health care services, social and environmental factors and the substances taken by SUD patients impact negatively on their oral status, well-being, and quality of life [Citation2,Citation5].
In accordance with international research, a recent Norwegian study concluded that patients in withdrawal rehabilitation experience a considerably higher prevalence of impaired oral health related quality of life (OHRQoL) than the general Norwegian adult population and that the degree of impairment increases with the severity of oral diseases and the number of missing teeth [Citation6,Citation7] The empirical data revealed that the patients were embarrassed about their mouth and teeth and felt their appearance of poor teeth negatively affected their social life [(Citation8,Citation9]. Further, considerably worse general healthrelated quality of life (HRQoL) has been observed among patients receiving opioid agonist therapy (OAT) compared with the general population [Citation10]. Nevertheless, studies of patients have provided equivocal findings and large variations in HRQoL scores [Citation11]. One study of patients with opioid addiction in Norway found that around 20% of patients had severe conditions and very low HRQoL while around 20% had similar or even better HRQoL scores compared to reference values in the general populations [Citation11].
Although OHRQoL measures include impacts from different oral diseases, they might be considered oral specific when compared with general HRQoL measures making them useful, particularly for economic evaluation [Citation12]. Many valid and reliable instruments are available for measuring OHRQoL and HRQoL. Oral Impact on daily performance (OIDP) is a commonly used OHRQoL measure that has been translated extensively and validated for use also in the context of the general Norwegian population [Citation13,Citation14]. A frequently used HRQoL instrument that has shown strong psychometrical properties across various national samples, including patients with SUD in Norway, is the 5-level EuroQol 5-dimensional questionnaire (EQ-5D-5L) [Citation4,Citation10,Citation15,Citation16]. Comparing groups with higher and lower dental anxiety, a recent study revealed that impacts assessed by oral specific- and generic healthrelated quality of life measures were greater in the anxiety than in a control group without dental anxiety [Citation12].
The oral cavity has been described as a window to general health. Thus, the relationship between oral health and general health is of considerable interest to the health- and dental health community [Citation17,Citation18]. Improving health by intervening in oral problems might be a practical goal of dental professionals. From the point of view of patients’ perceptions, the interaction between oral and general health is of increasing importance. Previous cross-sectional and longitudinal studies have indicated that poor oral health compromises general health and quality of life [Citation17–20]. Also, a review of HRQoL and OHRQoL has shown positive associations between these measures, for instance, in a German general population, in patients treated for head and neck cancer, and in a Spanish study of patients treated for oral cancer [Citation17,Citation21,Citation22]. However, findings are inconclusive, and there is a general lack of studies investigating the association of oral- and general health-related quality of life among patients with specific diseases. It is also uncertain whether findings based on general populations and patients with some specific diseases can be generalised to patients with SUD who receive opioid agonist therapy.
This study aimed to assess the association between oral and general health related quality of life measured by the instruments OIDP and EQ-5D-5L among patients with SUDs who receive opioid agonist therapy in Norway.
Material and methods
A prospective observational study linked to the integrated treatment of hepatitis C (INTRO-HCV) study was conducted between 2017 and 2020 [Citation23,Citation24]. In 2017, the study sample included patients (aged 18 and above) diagnosed with opioid dependence syndrome according to International Classification of Disease version 10 (ICD-10) and currently enrolled in opioid agonist therapy in nine opioid agonist therapy outpatient clinics in Western Norway. From a target population of 901 patients, 186 were unavailable or and the remaining 715 were invited to participate, and 609 participated (68% of target group, 85% response among invited) completed a health assessment regarding their general HRQOL instrument, EQ-5D-5L, and socio-demographic data. Trained research nurses collected the data through structured interviews with patients. The interviews were conducted when patients were cooperative without being substantially affected by substances or other significant psychosocial conditions. A sub-study, focussing on oral health related issues was conducted in six of the nine outpatient clinics proving opioid agonist therapy [Citation6]. All patients who attended the clinics during the survey period from December 2017 to February 2018 were consecutively invited to participate and agreed to participate in the study. A total of 167 patients (median age 45 years, 77% male) completed structural interviews at the outpatient clinics when attending for their opioid agonist therapy, regarding the OIDP, an inventory validated for Norwegian patients with SUDs [Citation6]. In addition, all patients underwent a brief oral clinical examination in the opioid agonist therapy clinic before receiving their opioid agonist therapy medication. Trained and calibrated oral health care personnel administered structured interviews, counted the participants’ number of remaining natural teeth, and examined their oral mucosa. After merging data from the INTRO HCV and the oral health sub-study conducted in 2017, the analytical sample consisted of 165 patients having complete data of EQ-5D-5L and OIDP instruments, socio-demographic characteristics, and the number of remaining maxillary and mandibular teeth. Baseline was defined as the time of the OIDP measurement. Participants were asked for a follow-up assessment with approximately one year interval from the first assessment. In total, 69 out of 165 (42%) patients conducted a second measurement of EQ-5D-5L with a mean interval of 14 months (standard deviation [sd] 6 months) from the baseline. These measurements were included to investigate changes in EQ-5D-5L values from baseline.
Measurements
EQ-5D-5l
The EQ-5D-5L has been used in general populations as well as in a broad range of patient groups and has been validated among patients with opioid use disorders [Citation10,Citation25–27]. This generic HRQoL instrument consists of two components, one descriptive system evaluating five health dimensions (mobility, self-care, usual activities, pain/discomfort, anxiety/depression) along five category levels ranging from no problems (level 1) to extreme problems (level 5). A total of 3,125 possible health states are defined by combining one level from each dimension ranging from 11111 (full health) to 55555 (worst health). Responses from the above-mentioned dimensions can be combined in a single health state in a form of a five-digit number ranging from the best state meaning no problems at any dimension to the worst state meaning extreme problems at all five dimensions. EQ-5D-5L health states are converted into a single index value using scoring algorithm based on public preferences. In the INTRO-HCV study, the UK value set and scoring algorithm were used to calculate utility score [Citation27]. The index value represents how good or bad a health state is according to preferences of the general population, ranging from < 0 (dead) to 1 (full/perfect health). We also calculated an EQ-5D-5L sum score ranging from 5 (no problems) to 25 (extreme problems) by summarizing the five items’ values (1–5).
OIDP
Oral health related quality of life was measured with the commonly used 8-item oral impact on daily performances, OIDP frequency inventory [Citation13], validated for use in the general Norwegian population as well as among patients with opioid use disorders in Norway [Citation6,Citation14]. OIDP consists of the following dimensions, ‘During the past six months how often have problems with your mouth and teeth caused you any difficulty with: (1) eating and enjoying food, (2) speaking and pronouncing clearly, (3) cleaning teeth, (4) sleeping and relaxing, (5) smiling and showing teeth without embarrassment, (6) maintaining usual emotional state, (7) enjoying contact with people and (8) carrying out major daily work’. Each item was scored on a five-point Likert scale, (0) never affected, (1) less than once a month, (2) once or twice a month, (3) once or twice a week, (4) every/nearly every day. A sum frequency unweighted OIDP score was constructed by adding each item as scored originally on a 4-point Likert scale (range 0–32). The OIDP frequency inventory has demonstrated satisfactory cross-sectional as well as longitudinal psychometric properties when applied in population-based surveys in Norway and other countries worldwide [Citation6].
Statistical methods
We used Stata/SE 17.0 (StataCorp, TX, USA) for the descriptive and linear regression analysis, and for creating line graphs. Microsoft Excel was used to create a bar chart and expectation-maximization algorithm was run by using the IBM SPSS version 26.0 (SPSS Inc, Chicago, IL, USA). Unless otherwise stated, the threshold for statistical significance was set to p < .05 for all analyses. We dealt with any missing values concerning the OIDP items and EQ-5D-5L dimensions as ‘missing at random’ when running expectation-maximization algorithm. We identified missing values in 10% in these items/dimensions and all were replaced with estimated values. A total of 1.4% of OIDP items and 20% of EQ-5D-5L items were replaced by estimated data.
Summary statistics revealed percentages and number of patients in each dimension of EQ-5D-5L- and OIDP. Spearman’s rho was used to assess the bivariate correlations between OIDP and EQ-5D-5L sum scores and the bivariate correlations between each of the 5 and 8 dimensions for EQ-5D-5L and OIDP, respectively. The association of OIDP with EQ-5D-5L was assessed in linear multiple variable analysis, adjusted for age and sex. A line graph and a Pen’s parade were created to display the distributions of OIDP sum scores and EQ-5D-5L index values when patients were listed chronologically (lowest to highest values/scores) at baseline. The Pen’s parade presenting the EQ-5D-5L index values also included the second measurement illustrated by spikes.
Ethics approval and consent to participate
The study is reviewed and approved by the Regional Ethical Committee for Health Research West, Norway (REK Vest 2017/51 and 2017/2264). Each patient provided written informed consent prior to enrolling in the study.
Results
Sample profile
As depicted in , among 165 patients with SUDs receiving opioid agonist therapy, the majority were males (76%), and 31% and 36% were in the age range 30–40 and 40–50 years, respectively. About half of the participants (48%) confirmed having completed primary school. The most commonly used substances during the past year were cannabis (62%) and benzodiazepines (50%). About half the participants (42%) had hepatitis C infection, and the mean number of remaining maxillary and mandibular teeth were respectively, eight and nine teeth.
Table 1. Basic characteristics of 165 patients with substance use disorders (numbers (n) and percentages (%).
EQ-5D-5L and OIDP scores
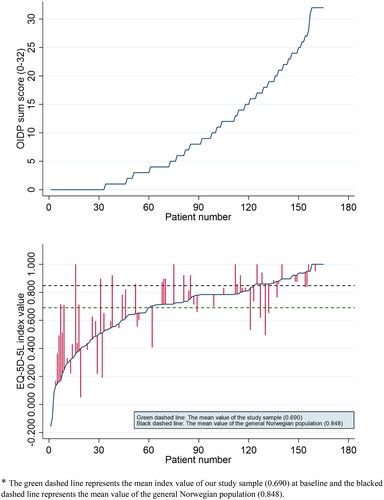
, displays the distribution of OIDP sum scores ranging from 0 (not affected) to 32 (extremely affected daily) when patients are ranged categorically from lowest to highest sum score. , displays a Pen’s parade of EQ-5D-5L index values (ranging from 0: dead to 1: perfect health) at baseline and the second measuring point (∼1 year later) when patients are listed in order from lowest to highest index score at baseline. The blue line represents the distribution of index values at baseline, and the red spikes (furthest from the blue line) demonstrate the changes in the index score from baseline to the second measuring point if completed two measurements. The green dashed line represents the mean index value for EQ-5D-5L of our study sample 0.690 (sd 0.222) (<0 = dead and 1 = perfect health) at baseline with a tendency towards higher index values in the second measuring point (0.708, sd 0.236).
Figure 1. (a + b) Pen’s parade figure presenting distribution of Oral Impact on daily performance sum score (0: not affected to 32: extremely affected) ordered from lowest to highest (a). Correspondingly, EQ-5D-5L index value (0: dead to 1: perfect health) at baseline is presented (b) with lines indicating change to value at second measuring point (∼1 year later). *The green dashed line represents the mean index value of our study sample (0.690) at baseline and the blacked dashed line represents the mean value of the general Norwegian population (0.848).
According to , the percentages reporting no problems for each of the five EQ-5D-5L dimensions were in descending order, 78% (self-care), 61% (mobility), 38% (usual activities), 26% (pain/discomfort), and 16% (anxiety/depression). According to , percentages of patients reporting never problems were in descending order, 67% (sleeping/relaxing), 65% (speaking), 65% cleaning teeth), 63% (enjoy social contact), 62% (emotional stability), 58% (carrying out work), 46% (showing teeth without embarrassment), and 41% (eating).
Figure 2. (a) Percentage distribution of eight OIDP dimensions among 165 patients with substance use disorder. (b) Percentage distribution of five EQ-5D-5L dimensions among 165 patients with substance use disorder.
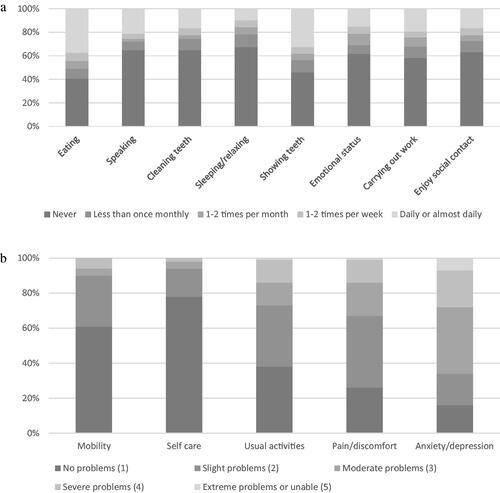
Table S1 (Supplementary) depicts the mean distribution of the five EQ-5L-5D (1–5) and the eight OIDP (0–4) dimensions for the total study group, according to gender and age groups. Overall mean summary EQ-5D-5L score amounted to 9.97 (range 5–25, sd 3.25). Overall mean summary OIDP score was 9.75 (range 0–32, sd 9.59) and 80% had sum scores above 0 (>0). Overall mean scores for the single EQ-5D-5L dimensions (1 = no problems to 5 =extreme problems) ranged from self-care (1.30, sd 0.66) to anxiety/depression (2.84, sd 1.14). Overall mean scores for the single OIDP items (0 = never problems to 4 = problems daily or almost daily) ranged from (0.80, sd 1.34) regarding sleeping/relaxing to (1.92, sd 1.81) regarding eating. Across most of the EQ-5L-5D dimensions, the mean values were higher (worse) among females than males and tended to increase with increasing age., Across the OIDP items, mean frequency tended to be higher (worse impacts) among females than males and tended to become lower with increasing age group implying less frequent impacts among older than among younger patients.
The OIDP summary score (range 0–32) and single item scores were significantly correlated with almost all dimensions and the summary score of EQ-5D-5L (range 5–25). Spearman’s rho was 0.34 (p < .01) for the unadjusted association between OIDP and EQ-5D-5L total sum scores. As depicted in , associations of EQ-5D-5L mobility dimension with OIDP items ranged from 0.11 (speaking) to 0.26 (cleaning teeth). Corresponding ranges of associations of EQ-5D-5L self- care-, usual activities-, pain/discomfort- and anxiety/depression dimensions are depicted in .
Table 2. Spearman’s correlations, rs, between each EQ-5D-5L of five dimensions (5 levels) and OIDP eight items (5 levels) among 165 patients with substance use disorder.
Association between EQ-5D-5L and OIDP adjusted for sex and age
Linear regression of the association between EQ-5D-5L sum score (5–20) and OIDP sum score (range 0–32) () and between EQ-5D-5L index value (0-1) and OIDP (scaled 0-1) () adjusted for age and sex revealed an associations amounting to 0.12 (95% confidence interval (CI) 0.07–0.17) and a coefficient of determination (R2) of 15% and an association of −0.23 (95% CI −0.34 to −0.12) with R2 of 12% indicating that the models explained about 14% and 12% of the variance in EQ-5D-5L sum score.
Table 3. Linear regression of the association between EQ-5D-5L sum score (5–20) and OIDP sum score (0–32) at baseline, sex, and age (n = 165).
Table 4. Linear regression of the association between EQ-5D-5-L index value (0-1) and OIDP (scaled 0-1) at baseline, sex, and age.
Discussion
Oral and general health related quality of life are multidimensional constructs that provide information of the oral and the overall health conditions in individuals and populations [Citation18,Citation28]. The latter includes dimension of functional, mobility, cognitive, mental health, and pain. Focussing on patients with SUD receiving opioid agonist therapy, this study aimed to assess associations between oral and general health related quality of life. The findings revealed substantial associations between oral- and health related quality of life, both summary- and single item/dimension scores, and in unadjusted and adjusted analyses. A similar summary score correlation coefficient has been reported in Germany among dental attendees [Citation28]. Almost all OIDP single items correlated significantly with each EQ-5D-5L dimension. Problems with eating were most strongly correlated with the EQ-5D-5L mobility and pain/discomfort dimensions. Problems carrying out work were strongly associated with all EQ-5D-5L dimensions, except the anxiety dimension and problems cleaning teeth were most strongly correlated with the mobility-, self-care, and usual activity dimensions. A review by Haag and co-workers [Citation29] confirmed that problems with mastication, swallowing, speech, and smile aesthetics due to oral diseases subsequently affected health related quality of life of general populations in various countries. The coefficient of determination (r2), describes the amount of variance to which oral health and health related quality of life overlaps, indicating the amount of health-related quality of life that might be affected in dental treatment. Overall, the present findings suggest that SUDs patients’ perception of oral health characterizes, at least to a certain degree, perceived general health and vice versa, thus being accordant with studies in the general population as well as in groups with various systemic diseases [Citation30–33].
The percentages reporting no problems were least for the anxiety/depression- and largest for the self-care dimensions of the EQ-5L-5D, meaning that a majority and minority of the participating SUD patients confirmed problems related to anxiety and self-care, respectively. Correspondingly, the percentages reporting having never problems according to the OIDP inventory were smallest regarding eating (41%) and largest for problems with sleeping and relaxing (67%), speaking (65%), and cleaning teeth (65%). In contrast, a previous study revealed that about 90% of the general Norwegian population was without problems across all OIDP items [Citation14]. The average EQ-5D-5L index value indicated that the health related quality of life among SUD patients was worse (0.690) than the reference value (0.848) estimated in the general Norwegian adult population [Citation34]. Moreover, SUD patients seemed to be disadvantaged regarding oral health related quality of life. Whereas 80% of the SUD patients reported impacts according to the OIDP sum score, the corresponding value for the general Norwegian population has been estimated to 18% [Citation14]. This is consistent with previous research showing that patients with SUDs have inferior health- and oral health related quality of life compared with controls and the general populations [Citation6,Citation35].
Mean impact scores across the five EQ- and eight OIDP domains were in general higher among females than males indicating sex differences in perceived oral and general health related problems. Except for the anxiety dimension, the mean EQ-5D-5L dimensions were lower among the younger than the older SUD patients. This accords with previous studies in several countries indicating that perceptions of health problems seem to be more moderate among younger than older individuals [Citation36]. Similar findings regarding the age distribution of the anxiety/depression dimension have also been reported in studies from Slovenia, China, Indonesia, and Italy [Citation36], suggesting further research into this dimension. Across all OIDP items, the mean scores were higher in the youngest than the oldest age group – indicating that younger patients have poorer oral health perceptions than their older counterparts. Several factors have been suggested to contribute to this unexpected trend with a plausible explanation being that oral problems such as tooth loss are seen as a normal consequence of ageing and that greater initiative regarding healthy lifestyle might contribute to increase younger peoples’ expectations to oral health.
A strength of this study is that we employed two commonly used quality of life instruments validated for the Norwegian context [Citation6,Citation34]. However, since both instruments are generic, they might not be highly sensitive for impairments [Citation12]. For instance, an orofacial aesthetics scale might be more sensitive for aesthetic impairment than the OIDP inventory [Citation35]. Substantial correlations between the two constructs could be attributed to the cross-sectional study design and the generic nature of the measurement instruments. On the other hand, we did not consider measurement errors that might have weakened the correlations observed. Seculic and co-workers [Citation31] in a study of dental patients, reported on much higher correlations estimated with a statistical technique that allows modelling variables directly, and thus eliminating measurement errors occurring during data analysis. Also due to the cross-sectional design of our study and in spite of the substantial correlations observed, no causal inference can be made regarding the relationship between the two quality of life measures. In addition, unmeasured confounding variables might have biased our data and since our study as based entirely on self-report data, social desirability and recall biases cannot be ruled out. Another study limitation worthwhile of being noted is the majority of males in the study group which may have resulted in insufficient statistical power to detect an effect in females.
It is well documented that oral diseases, such as dental caries and tooth loss, are prevalent among patients with illicit substance use [Citation2,Citation7]. Published reviews have shown that these patients suffer from more severe oral diseases than the general population – however, with a substantial range in frequency and severity [Citation36,Citation37]. National and international studies have reported that in addition to an increased oral disease burden, a range of adverse health consequences of substance use have been reported, such as mental disorders and pulmonary and infectious diseases (tuberculosis and hepatitis) [Citation1,Citation10]. Moreover, oral diseases impact both oral health- and health related quality of life, as reported by most available evidence [Citation33]. Several explanations might be suggested for the relationship between oral health-and health related quality of life observed in this study. Oral diseases affect the local oral area but might also impact other organ systems directly and indirectly, for instance, oral cancer, temporomandibular disorder, and tooth loss that evoke distal metastases and mental disorders, respectively [Citation17]. Thus, impaired oral health could have substantial impact on general quality of life. Oral- and systemic diseases have common risk factors and are reflected by oral – and overall health related quality of life that might evoke associations between the two constructs. It is also likely that some of the associations are related to common risk factors. Substantial correlation between oral- and overall health related quality of life observed in this study could have suggested that SUD patients suffered oral disease with systemic manifestations or systemic diseases with oral manifestations.
Conclusion
The substantial correlation between summary OIDP and EQ-5D-5L scores estimated in this study reflects the importance of oral health to the general health for patients with SUDs receiving opioid agonist therapy. Poor oral health could impact negatively on general quality of life and could also be an indicator of the presence of common risk factors that needs attention. This should be considered in the development of preventive strategies suggesting that health care professionals should pay attention to oral health. Effective preventive and therapeutic interventions by dentists and other health professionals might improve patients’ oral and general health related quality of life. Knowing the magnitude of the relationship could facilitate a more patient-centered treatment approach for patients with SUDs receiving opioid agonist therapy.
Author contributions
ANÅ: had the idea of this study and wrote the manuscript. ANÅ, LTF, JHV, CFAA and KAJ designed the study. CFA and JHV performed data management and conducted statistical analyses. All authors contributed to writing of the manuscript and confirmed its final version.
Supplemental Material
Download MS Word (17.7 KB)Acknowledgements
Authors appreciate contribution from OMT patients and oral health care workers in Bergen. We thank the patients, devoted clinical staff, and INTRO-HCV Study Group (see list below) for their help during the project. We also thank Nina Elisabeth Eltvik and Christer Kleppe for valuable help and input during the planning and preparation phases. The INTRO-HCV Study Group participating investigators are the following: Bergen: Christer Frode Aas, Vibeke Bråthen Buljovcic, Fatemeh Chalabianloo, Jan Tore Daltveit, Silvia Eiken Alpers, Lars T. Fadnes (principal investigator), Trude Fondenes Eriksen, Rolf Gjestad, Per Gundersen, Velinda Hille, Kristin Holmelid Håberg, Kjell Arne Johansson, Rafael Alexander Leiva, Siv-Elin Leirvåg Carlsen, Martine Lepsøy Bonnier, Lennart Lorås, Else-Marie Løberg, Mette Hegland Nordbotn, Maria Olsvold, Christian Ohldieck, Lillian Sivertsen, Hugo Torjussen, Jørn-Henrik Vold, and Jan-Magnus Økland; Stavanger: Tone Lise Eielsen, Nancy Laura Ortega Maldonado, and Ewa Joanna Wilk; proLAR: Ronny Bjørnestad, Ole Jørgen Lygren, and Marianne Cook Pierron; Oslo: Olav Dalgard, Håvard Midgard, and Svetlana Skurtveit; Bristol: Aaron G. Lim and Peter Vickerman (in alphabetical order of surname).
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Data upon which this study is based is available from the authors upon request.
Additional information
Funding
References
- United Nations. Drug use and health consequences. World drug report. 2020; [cited 2020 Sep 08]. Available from: https://wdr.unodc.org/wdr2020/en/exsum.html.
- Pedersen AM. Rusmidler og mundhulen. Aktuell Nordisk Odontologi. 2016;41(1):98–111.
- ] Rodriguez-Miguez E, Casal B, Rivera B. Measuring health related quality of life in patients treated for substance dependence: differences among instruments and methods of eliciting preferences. Expert Rev Pharmacoecon Outcomes Res. 2021;21(4):683–690.
- Bray J, Aden B, Eggman AA, et al. Quality of life as an outcome of opioid use disorder treatment: a systematic review. J Subst Abuse Treat. 2017;76:88–93.
- Shekarchizadeh H, Khami MR, Mohebbi SZ, et al. Oral health status and its determinants among opiate dependents: a cross sectional study. BMC Oral Health. 2019;19(1):5.
- Åstrøm AN, Virtanen J, Ozkaya F, et al. Oral health related quality of life and reasons for non-dental attendance among patients with substance use disorders in withdrawal rehabilitation. Clin Exp Dent Res. 2022;8(1):68–75.
- Amiri S, Shekarchizadeh H. Oral health related quality of life among a group of patients with substance use disorder in rehabilitation treatment: a cross sectional study. BMC. 2021;21(1):409.
- Leirvaag Carlsen SE, Åstrøm AN, Fadnes LT. Facilitators for use of oral health care services among people with substance use disorders: a qualitative study in Norway. Acta Odontol Scand. 2022;24:1–9.
- Leirvaag Carlsen SE, Isaksen K, Fadnes LT, et al. Non-financial barriers in oral health care: a qualitative study of patients receiving opioid maintenance treatment and professionals’ experiences. Subst Abuse Treat Prev Policy. 2021;16(1):44.
- Aas CF, Vold JH, Skurtveit S, et al. Health related quality of life of long-term patients receiving opioid agonist therapy: a nested prospective cohort study in Norway. Subst Abuse Treat Prev Policy. 2020;15(1):68.
- Barrios R, Bravo M, Gil-Montoya JA, et al. Oral and general health related quality of in patients treated for oral cancer compared to control group. Health Qual Life Outcomes. 2015;13:9.
- Vermaire JH, van Houtem CMHH, Ross JN, et al. The burden of disease of dental anxiety: generic and disease specific quality of life in patients with and without extreme levels of dental anxiety. Eur J Oral Sci. 2016;124(5):454–458.
- Adulyanon S, Sheiham A. Oral impact on daily performances. In: Measuring oral health and quality of life. Edited: Chapter Hill: university of North Carolina; 1997. p. 151–160.
- Astrom AN, Haugejorden O, Skaret E, et al. Oral impacts on daily performances in Norwegian adults: validity, reliability and prevalence estimates. Eur J Oral Sci. 2005;113(4):289–296.
- McCaffrey N, Kaambwa B, Currow DC, et al. Health related quality of life measured using the EQ-5D-5L: South Australian population norms. Health Qual Life Outcomes. 2016;14(1):133.
- Garratt AM, Furunes H, Hellum C, et al. Evaluation of the EQ-5D-3L and 5L versions in low back pain patients. Health Qual Life Outcomes. 2021;19(1):155.
- Reissman DR, John MT, Schierz O, et al. Association between perceived oral and general health. J Dent. 2013;41(7):581–589.
- Zimmer S, Bergmann N, Bagrun E, et al. Association between oral health related and general health related quality of life in subjects attending dental offices in Germany. J Public Health Dent. 2010;70:167–170.
- Locker D, Clarke M, Payne B. Self perceived oral health status, psychological well being and life satisfaction in an older adult population. J Dent Res. 2000;79(4):970–975.
- Sagtani RA, Thapa S, Sagtani A. Smoking, general and oral health related quality of life- a comparative study from Nepal. Health Qual Life Outcomes. 2020;18(1):257.
- Barrios R, Montero J, González-Moles M-A, et al. Levels of scientific evidence of quality of life in patients treated for oral cancer. Med Oral Patol Oral Cir Bucal. 2013;18(4):e578-84.
- Barrios R, Tsakos G, Gil-Montoya JA, et al. Association between general and oral health related quality of life in patients treated for oral cancer. Med Oral Patol Oral Cir Bucal. 2015;20(6):e678-84.
- Fadnes LT, Aas CF, Vold JH, et al. Integrated treatment of hepatitis C virus infection among people people who inject drugs: study protocol for a randomized controlled trial (INTRO.HCV). BMC Infect Dis. 2019;19(1):943.
- Fadnes LT, Aas CF, Vold JH, et al. Integrated treatment of hepatitis C virus infection among people who inject drugs: a multicenter randomized controlled trial (INTRO-HCV). PLoS Med. 2021;18(6):e1003653.
- Rabin R, de Charro F. EQ-5D: a measure of health status from the EuroQol group. Ann Med. 2001;33(5):337–343.
- Lamu AN, Björkman L, Hamre HJ, et al. Validity and responsiveness of EQ-5D-5L and SF-6D in patients with health complaints attributed to their amalgam fillings: a prospective cohort study of patients undergoing amalgam removal. Health Qual Life Outcomes. 2021;19(1):125.
- Devlin NJ, Shah KK, Feng Y, et al. Valuing health related quality of life: an EQ-5D-5Lvalue set for England. Health Econ. 2018;36:645–661.
- Tran TD, Krausch-Hofman Duyck J, deAlmeida Mello J, et al. Association between oral health and general health indicators in older adults. Sci Rep. 2018;8(1):8871.
- Haag DG, Peres KG, Balasubramanian M, et al. Oral conditions and health related quality of life: a systematic review. J Dent Res. 2017;96(8):864–874.
- Zucoloto ML, Maroco J, Campos JADB. Impact of oral health on health related quality of life: a cross-sectional study. BMC Oral Health. 2016;16(1):55.
- Sekulic S, John MT, Davey C, et al. Association between oral health related and health related quality of life. Zdr Varst. 2020;59(2):65–74.
- Mohamed N, Saddki N, Yusoff A, et al. Association among oral symptoms, oral health related quality of life and health related quality of life in a sample of adults living with HIV/AIDS in Malaysia. BMC Oral Health. 2017;17(1):119.
- da Costa Vieira V, Lins L, Sarmento VA, et al. Oral health and health related quality of life in HIV patients. BMC Oral Health. 2018;18(1):51.
- Stavem K, Augestad LA, Kristiansen IS, et al. General population norms for the EQ-5D-3L in Norway: comparisons of postal and web surveys. Health Qual Life Outcomes. 2018;16(1):204.
- John MT, Larsson P, Nilner K, et al. Validation of the orofacial esthetic scale in the general population. Health Qual Life Outcomes. 2012;10:135.
- Griffin ML, Bennett HE, Fitzmaurice GM, et al. Health related quality of life among opioid-dependent patients: results from a multi center study. Am J Addict. 2015;24(4):308–314.
- Baghaie H, Kisely S, Forbes M, et al. A systematic review and meta- analysis of the association between poor oral health and substance abuse. Addiction. 2017;112(5):765–779.
