Abstract
Background Several authors have found poorer outcome after hip replacement for osteonecrosis than after hip replacement for arthrosis. In a retrospective study we evaluated the performance of an uncemented femoral component in patients with osteonecrosis and arthrosis of the hip.
Patients and methods 31 patients operated for osteonecrosis, and 49 patients operated for osteoarthrosis were included. The median follow-up time was 6.1 (2–11) years for the patients with osteonecrosis, and 5.9 (4–8) for the arthrosis patients.
Results Migration analysis performed by the Einzel-Bild-Roentgen Analysis (EBRA) technique revealed a median stem migration of 1.5 (−8.8–0) mm in the patients with osteonecrosis, but only 0.6 (−2.8–0.7) mm in the patients with arthrosis (p < 0.001). Survivorship analysis with stem revision as endpoint for failure was 74% (95% CI: 55–94) in the osteonecrosis, and 98% (95% CI: 94–100) in the arthrosis group (p = 0.01).
Interpretation We suggest that the higher failure rate and stem migration of uncemented total hip replacement in the patients with osteonecrosis is a consequence of the disease. On the basis of these findings, we recommend close monitoring of the patients with osteonecrosis, which should include migration measurements.
In advanced osteonecrosis with collapsed femoral head and disabling pain, total hip replacement or femoral endoprosthesis remains the treatment of choice (Mont and Hungerford Citation1995, Hungerford et al. Citation1998). However, reported outcomes of total hip replacement in the osteonecrosis population have not been as good as in patients with arthrosis. Patients with osteonecrosis tend to be younger and more active than arthrosis patients, which may account for the discrepancy (Cornell et al. Citation1985, Saito et al. Citation1989, Brinker et al. Citation1994, Ortiguera et al. Citation1999). Alternatively, changes in the bone quality in the proximal femur seen in osteonecrosis may compromise the result (Arlot et al. Citation1983). For long-term stability of the femoral component, bony integration remains the key requirement. Instability and consequent subsidence may be a sign of aseptic loosening (Engh et al. Citation1987). However, no correlations between clinical symptoms or patient satisfaction and component loosening were found in a study by Iwase et al. (Citation2002). These authors thus emphasized precise and serial long-term radiographic follow-up as the only satisfactory method for detection of aseptic loosening of total hip arthroplasty. One possible measure of the quality of implant fixation is the rate of migration.
Although total hip replacement in patients with osteonecrosis has been reported to be less durable (Sarmiento et al. Citation1990, Lieberman et al. Citation2002), we are not aware of a study that has compared the rate of migration of the same femoral component in patients with osteonecrosis and osteoarthrosis of the hip. In this retrospective study, we analyzed the midterm results of uncemented total hip replacement in patients with arthrosis or osteonecrosis of the femoral head by using EBRA-Femoral Component Analysis (EBRA-FCA) in conjunction with the clinical data.
Patients and methods
From 1990 to 2000, 41 consecutive patients with advanced osteonecrosis (Ficat stage III and IV) (Ficat Citation1985) received uncemented total hip replacements at our institution. We used 5 prosthetic devices during this time. However, 31 of these patients (35 hips) were operated with the same uncemented stem design (Austria Hip System, Logimed) during this period, and were included in the study. These patients were compared with a control group of 49 consecutive patients (58 hips) who underwent total joint replacement for arthrosis using the same prosthesis with a comparable midterm follow-up interval. For inclusion in this retrospective study, the patients with arthrosis of the hip had to be aged 19–70 years. In patients with both hips operated, only the hip that was operated on firstly was included in the study.
Among the 31 patients with osteonecrosis, there were 12 women. The etiologies were alcohol abuse in 12, corticosteroid medication in 9, idiopathic in 5, posttraumatic osteonecrosis in 4, and sickle-cell-disease in 1 case. In the group with total hip arthroplasty following arthrosis of the hip, there were 49 patients (31 women). At the time of last follow-up, 4 patients (2 patients in each group) had died from causes unrelated to the index hip surgery. The remaining 29 patients in the osteonecrosis group and 47 patients in the osteoarthrosis group could be reached for follow-up examination. Demographic data including number of patients, age, body weight, follow-up interval, and the Harris hip score at the final follow-up are given in .
Table 1. Demographic data and results of patients with osteonecrosis and arthrosis of the hip
A modified anterolateral transgluteal approach was used in all hips (Bauer et al. Citation1979). The uncemented implant used in all cases was a straight, collarless stem (Ti-6Al-4Va) with a hydroxyapatite coating in the proximal two-thirds combined with a spherical press-fit cup (Ti-6Al-4Va), a polyethylene liner and a ceramic head ().
Figure 1. The uncemented total hip replacement device with a straight, collarless stem made of a titanium-alu-minium-vanadium alloy (Ti-6Al-4Va), with an additional coating of hydroxyapatite in the proximal two-thirds, which was combined with spherical press-fit cup (Ti-6Al-4Va), a polyethylene liner and a ceramic head.

The patients were mobilized with partial weight bearing during the first 6 weeks after the operation. The clinical outcome was rated according to the Harris (Citation1969) hip score. At scheduled postoperative visits, standardized radiographs were obtained which were compared to serial radiographs. Analysis of radiolucent lines (parallel lines of more than 1 mm and 50% of the different regions were considered positive), bone atrophy, hypertrophy, and osteolysis (any scalloping changes around the socket or in the femoral cortex) at the femoral and acetabular site were performed in the Gruen et al. (Citation1979) femoral regions, and the DeLee and Charnley (Citation1976) acetabular regions. The biological fixation of the stem was assessed by a modification of the criteria described by Engh et al. (Citation1990), using the overall score (fixation and stability score) for the degree of adequacy of biological fixation of the stem. Radiographic failure of the stem was defined as a complete radiolucent line or an overall Engh score of less than −10 points.
Anteroposterior radiographs of the hip were digitized using a resolution of 75 dpi. The Einzel-Bild-Roentgen Analysis-Femoral Component Analysis (EBRA-FCA) was utilized for analysis of migration (Biedermann et al. Citation1999). This method is known to have a specificity of 100% and a sensitivity of 78% compared to RSA for the detection of migration of over 1 mm (Krismer et al. Citation1995, Citation1999, Biedermann et al. Citation1999).
Statistics
Kaplan-Meier survival analysis applying stem revision and mechanical failure as the endpoint were performed with use of the NCSS 2004 statistics package (NCSS, Kaysville, UT, USA). Continuous variables were tested for significance with the Mann-Whitney U-test. Cox regression and multivariate linear regression analysis was done to determine any association between mechanical stem failure, migration and patient-related factors (age, sex, weight and diagnosis). A two-tailed p-value of less than 0.05 was considered to be statistically significant.
Results
Complications
At the latest follow-up visit, 3 patients in the osteonecrosis group complained about thigh pain. In one of these patients a stem subsidence of 2.8 mm, and progressive radiolucent lines were detected. An aseptic stem loosening was presumed and the patient was scheduled for revision operation. In the osteoarthrosis group 1 patient complained of thigh pain, but there were no signs of radiographic stem loosening. There were 3 postoperative hip dislocations. All dislocations were in the osteonecrosis group with alcohol abuse as the underlying disease. In 2 patients a closed reduction was done, and in 1 patient reoperation with change to a longer head and an antiluxation liner was performed. There were no dislocations in the arthrosis group.
3 patients in the osteonecrosis group (2 alco-hol-related, 1 corticoid-related) developed a peri-prosthetic femoral fracture after a trauma. They were reoperated with open reduction and internal fixation followed by revision of the femoral component in 2 of the cases. In 2 patients with osteonecrosis due to alcohol abuse, the polyethylene liner was changed because of excessive wear. The first patient, who was 70 years old at the time of the primary operation, was operated 8 years later. The second patient (40 years old) was reoperated 5 years after implantation. In the osteonecrosis group (2 alcohol-related, 2 corticoid-related, and 1 with sickle-cell disease) 5 patients had femoral component revision for aseptic loosening. 2 patients from the osteoarthrosis group had revision of the femoral component for aseptic loosening. No acetabular component revision had to be performed in either group.
Radiographic evaluation and migration analysis ( and )
According to the radiographic criteria for fixation and stability of the stem, the median overall Engh score was −3 (−26–16) points in the osteonecrosis group, and 21 (−14–26) points in the arthrosis group (p < 0.001).
Table 2. Radiographical evaluation including femoral bone radiolucency, atrophy, hypertrophy and osteolysis in the seven Gruen zones
Table 3. Radiographical evaluation of the acetabular component including radiolucency, atrophy, and osteolysis in the DeLee and Charnley zones
For the migration analysis, 7 hips were excluded since the pictures did not meet set standards for comparability. There were too few pictures in 2 other cases. A complete migration analysis could be performed in 22 of the 29 hips in the osteonecrosis group and in 45 of the 47 hips in the arthrosis group. The median stem migration in the osteonecrosis group was 1.5 (−8.8–0) mm, and in the arthrosis group the median migration was 0.6 (−2.6–0) mm (p < 0.001) ().
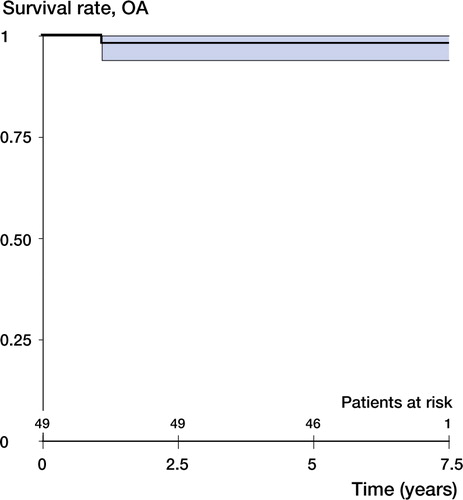
Survivorship analysis with stem revision as endpoint for failure was 74% (95% CI 55–94) in the osteonecrosis group, and 98% (CI: 94–100) in the arthrosis group (p = 0.01) ( and ). Survival with mechanical failure (radiographic failure and stem revision) was 54% (CI: 31–76) in the osteonecrosis group, and 98% (CI: 94–100) in the arthrosis group (p < 0.001) ( and ). Multivariate Cox regression analysis and multivariate linear regression analysis revealed the diagnosis to be the only statistically significant factor for the mechanical failure (p < 0.01), revision (p = 0.05), and migration of the femoral component (p < 0.001).
Figure 2. Kaplan-Meier life-table analysis with stem revision (for any reason) as the endpoint. Bold line: survival curve. Thin lines: 95% confidence limits. In the osteonecrosis group, the survival rate of the femoral component was 74% (95% CI: 55–34). The median follow-up time for the patients was 6.1 (2–11) years.
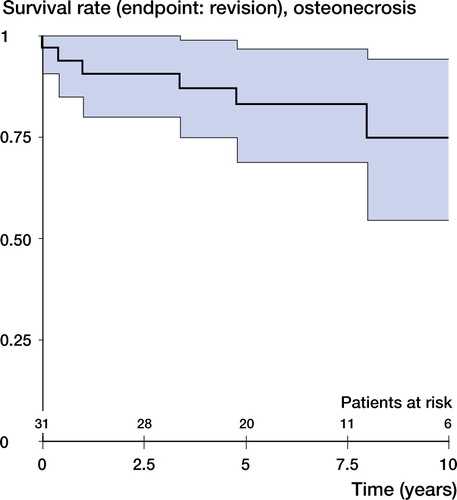
Figure 3. Kaplan-Meier life-table analysis with mechanical failure as the endpoint. Bold line: survival curve. Thin lines: 95% confidence limits. In the osteonecrosis group, the survival rate of the femoral component was 54% (CI: 31–76). The median follow-up time for the patients was 6.1 (2–11) years.
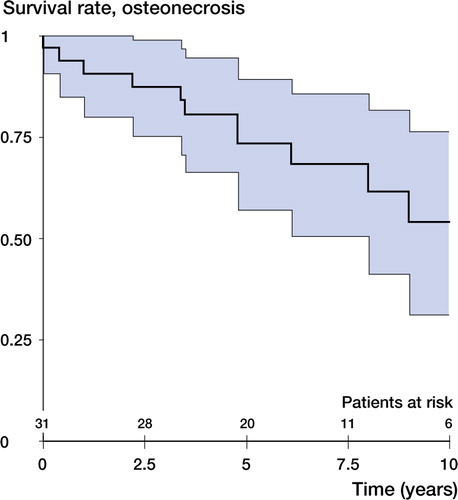
Figure 4. Kaplan-Meier life-table analysis with stem revision for any cause as the endpoint. Bold line: survival curve. Thin lines: 95% confidence limits. In the osteoarthrosis group, the survival rate of the femoral component was 98% (CI: 94–100). The median follow-up time for the patients was 5.9 (4–8) years.
Discussion
Osteonecrosis of the femoral head is said to be the reason for about 10% of primary hip arthroplasties (Hungerford et al. Citation1998). Usually, this disease occurs in male patients aged less than 50 years, who tend to be more active than patients with arthrosis undergoing total hip replacement. Patients with osteonecrosis of the femoral head are at a higher risk of some specific postoperative complications such as postoperative dislocation (Chiu et al. Citation1997), which was also observed by us. The periprosthetic femoral fractures in our patients seemed to be related to severe alcoholism.
Two factors are known to strongly influence the outcome of the procedure in patients with osteonecrosis. Survivorship analysis of the Swedish, Danish, and the Finnish hip arthroplasty population showed that the results were disappointing in patients below the age of 55 (Malchau et al. Citation1993, Lucht Citation2000, Puolakka et al. Citation2001). Secondly, higher revision rates after total hip replacement for end-stage osteonecrosis than for patients with arthrosis have been reported (Dorr et al. Citation1983, Cornell et al. Citation1985, Saito et al. Citation1989, Mont and Hungerford Citation1995, Ortiguera et al. Citation1999). Modern cementation techniques have improved the results of total hip arthroplasty in patients with osteonecrosis (Kantor et al. Citation1996, Garino and Steinberg Citation1997, Ritter et al. Citation1997). Satisfactory results with uncemented implants encouraged several authors to recommend uncemented implants in these relatively young patients (Lins et al. Citation1993, Phillips et al. Citation1994, Piston et al. Citation1994, Hartley et al. Citation2000, Xenakis et al. Citation2001, Capello et al. Citation2003, Reikeras and Gunderson Citation2003).
Apart from the age of this patient population, the reason for implant failure may be poor bone quality associated with the underlying diagnosis (Sarmiento et al. Citation1990, Brinker et al. Citation1994, Chiu et al. Citation1997). We support this notion. In a histomorphometric study in 77 adult patients with aseptic osteonecrosis, transiliac bonebiopsy showed a significant reduction in bone volume. The thickness of the osteoid seems to indicate that a systemic bone disease, either osteoporosis or osteomalacia, may co-exist with aseptic osteonecrosis in most patients (Arlot et al. Citation1983). It is easy to speculate that this deficiency may compromise bony ingrowth of the implant, which could be the reason for early instability and subsequent stem subsidence seen in our patients. These observations are similar to the findings of Mjöberg (Citation1997) who postulated that early loosening of hip prostheses is either a consequence of insufficient initial fixation or early loss of fixation. The most frequent secondary causes of osteoporosis in men are corticosteroid use and alcohol abuse, thus closely following the most commonly associated conditions of the osteonecrosis (Binkley and Krueger Citation2002). The clinical relevance of the extension of the osteonecrosis in the proximal femur was shown by Saito et al. (Citation1989). Most of the hips with component loosening presented histological evidence of extensive bone necrosis (Saito et al. Citation1989). Thus, it seems likely that both extension of osteonecrosis and secondary osteoporosis in the osteonecrosis population may influence the bony ingrowth of the prosthetic device.
A reliable method of assessing the stability of the prosthetic device is to measure the migration. Radiostereometric analysis (RSA) has become the golden standard for measuring implant migration (Ornstein et al. Citation2000), but the EBRA technique, although less accurate, has also proven to be reliable and effective (Krismer et al. Citation1999). Several studies have demonstrated clearly that early migration can predict implant failure with high accuracy (Kärrholm et al. Citation1994, Walker et al. Citation1995, Kobayashi et al. Citation1997, Biedermann et al. Citation1999).
The significant difference in the subsidence and survival of the femoral component in the patients with osteonecrosis and arthrosis of the hip supports the notion that the results of total hip replacement are strongly influenced by the osteonecrosis. Our study suggests—but cannot prove—the assumption that the bone around the prosthesis may be influenced by the osteonecrosis. However, this hypothesis should be the subject of further prospective studies including DEXA scan to assess the local bone quality. The increased stem subsidence emphasizes the need for close monitoring in the osteonecrosis patients, which should include accurate migration measurements.
No competing interests declared.
- Arlot M E, Bonjean M, Chavassieux P M, Meunier P J. Bone histology in adults with aseptic necrosis. Histomorphometric evaluation of iliac biopsies in seventy-seven patients. J Bone Joint Surg (Am) 1983; 65: 1319–27
- Bauer R, Kerschbaumer F, Poisel S, Oberthaler W. The transgluteal approach to the hip joint. Arch Orthop Trauma Surg 1979; 95: 47–9
- Biedermann R, Krismer M, Stockl B, Mayrhofer P, Ornstein E, Franzen H. Accuracy of EBRA-FCA in the measurement of migration of femoral components of total hip replacement. Einzel-Bild-Rontgen-Analyse-femoral component analysis. J Bone Joint Surg (Br) 1999; 81: 266–72
- Binkley N, Krueger D. Osteoporosis in men. WMJ 2002; 101: 28–32
- Brinker M R, Rosenberg A G, Kull L, Galante J O. Primary total hip arthroplasty using noncemented porous-coated femoral components in patients with osteonecrosis of the femoral head. J Arthroplasty 1994; 9: 457–68
- Capello W N, D'Antonio J A, Feinberg J R, Manley M T. Ten-year results with hydroxyapatite-coated total hip femoral components in patients less than fifty years old. A concise follow-up of a previous report. J Bone Joint Surg (Am) 2003; 85: 885–9
- Chiu K H, Shen W Y, Ko C K, Chan K M. Osteonecrosis of the femoral head treated with cementless total hip arthroplasty. A comparison with other diagnoses. J Arthroplasty 1997; 12: 683–8
- Cornell C N, Salvati E A, Pellicci P M. Long-term follow-up of total hip replacement in patients with osteonecrosis. Orthop Clin North Am 1985; 16: 757–69
- DeLee J G, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop 1976, 121: 20–32
- Dorr L D, Takei G K, Conaty J P. Total hip arthroplasties in patients less than forty-five years old. J Bone Joint Surg (Am) 1983; 65: 474–9
- Engh C A, Bobyn J D, Glassman A H. Porous-coated hip replacement. The factors governing bone ingrowth, stress shielding, and clinical results. J Bone Joint Surg (Br) 1987; 69: 45–55
- Engh C A, Massin P, Suthers K E. Roentgenographic assessment of the biologic fixation of porous-surfaced femoral components. Clin Orthop 1990, 257: 107–28
- Ficat R P. Idiopathic bone necrosis of the femoral head. Early diagnosis and treatment. J Bone Joint Surg (Br) 1985; 67: 3–9
- Garino J P, Steinberg M E. Total hip arthroplasty in patients with avascular necrosis of the femoral head: a 2- to 10year follow-up. Clin Orthop 1997, 334: 108–15
- Gruen T A, McNeice G M, Amstutz H C. “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop 1979, 141: 17–27
- Harris W H. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg (Am) 1969; 51: 737–55
- Hartley W T, McAuley J P, Culpepper W J, Engh C A, Jr., Engh C A, Sr. Osteonecrosis of the femoral head treated with cementless total hip arthroplasty. J Bone Joint Surg (Am) 2000; 82: 1408–13
- Hungerford M W, Mont M A, Scott R, Fiore C, Hungerford D S, Krackow K A. Surface replacement hemiarthroplasty for the treatment of osteonecrosis of the femoral head. J Bone Joint Surg (Am) 1998; 80: 1656–64
- Iwase T, Wingstrand I, Persson B M, Kesteris U, Hasegawa Y, Wingstrand H. The ScanHip total hip arthroplasty: radiographic assessment of 72 hips after 10 years. Acta Orthop Scand 2002; 73: 54–9
- Kantor S G, Huo M H, Huk O L, Salvati E A. Cemented total hip arthroplasty in patients with osteonecrosis. A 6- year minimum follow-up study of second-generation cement techniques. J Arthroplasty 1996; 11: 267–71
- Kärrholm J, Borssen B, Lowenhielm G, Snorrason F. Does early micromotion of femoral stem prostheses matter? 4-7-year stereoradiographic follow-up of 84 cemented prostheses. J Bone Joint Surg (Br) 1994; 76: 912–7
- Kärrholm J, Herberts P, Hultmark P, Malchau H, Nivbrant B, Thanner J. Radiostereometry of hip prostheses. Review of methodology and clinical results. Clin Orthop 1997, 344: 94–110
- Kobayashi A, Donnelly W J, Scott G, Freeman M A. Early radiological observations may predict the long-term survival of femoral hip prostheses. J Bone Joint Surg (Br) 1997; 79: 583–9
- Krismer M, Bauer R, Tschupik J, Mayrhofer P. EBRA: a method to measure migration of acetabular components. J Biomech 1995; 28: 1225–36
- Krismer M, Biedermann R, Stockl B, Fischer M, Bauer R, Haid C. The prediction of failure of the stem in THR by measurement of early migration using EBRA-FCA. Einzel-Bild-Roentgen-Analyse-femoral component analysis. J Bone Joint Surg (Br) 1999; 81: 273–80
- Lieberman J R, Berry D J, Aaron R K, Mont M A, Callaghan J J, Rayadhyaksha A, Urbaniak J R. Osteonecrosis of the Hip: Management in the Twenty-first Century. J Bone Joint Surg (Am) 2002; 84: 834–53
- Lins R E, Barnes B C, Callaghan J J, Mair S D, McCollum D E. Evaluation of uncemented total hip arthroplasty in patients with avascular necrosis of the femoral head. Clin Orthop 1993, 297: 168–73
- Lucht U. The Danish Hip Arthroplasty Register. Acta Orthop Scand 2000; 71: 433–9
- Malchau H, Herberts P, Ahnfelt L. Prognosis of total hip replacement in Sweden. Follow-up of 92,675 operations performed 1978–1990. Acta Orthop Scand 1993; 64: 497–506
- Mjöberg B. The theory of early loosening of hip prostheses. Orthopedics 1997; 20: 1169–75
- Mont M A, Hungerford D S. Non-traumatic avascular necrosis of the femoral head. J Bone Joint Surg (Am) 1995; 77: 459–74
- Ornstein E, Franzen H, Johnsson R, Sundberg M. Radiostereometric analysis in hip revision surgery–opti-mal time for index examination. 6 patients revised with impacted allografts and cement followed weekly for 6 weeks. Acta Orthop Scand 2000; 71: 360–4
- Ortiguera C J, Pulliam I T, Cabanela M E. Total hip arthroplasty for osteonecrosis: matched-pair analysis of 188 hips with long-term follow-up. J Arthroplasty 1999; 14: 21–8
- Phillips F M, Pottenger L A, Finn H A, Vandermolen J. Cementless total hip arthroplasty in patients with steroid-induced avascular necrosis of the hip. A 62-month follow-up study. Clin Orthop 1994, 303: 147–54
- Piston R W, Engh C A, De Carvalho P I, Suthers K. Osteonecrosis of the femoral head treated with total hip arthroplasty without cement. J Bone Joint Surg (Am) 1994; 76: 202–14
- Puolakka T J, Pajamaki K J, Halonen P J, Pulkkinen P O, Paavolainen P, Nevalainen J K. The Finnish Arthroplasty Register. Report of the hip register. Acta Orthop Scand 2001; 72: 433–41
- Reikeras O, Gunderson R B. Excellent results of HA coating on a grit-blasted stem. 245 patients followed for 8–12 years. Acta Orthop Scand 2003; 74: 140–5
- Ritter M A, Helphinstine J., Keating E M, Faris P M, Meding J B. Total hip arthroplasty in patients with osteonecrosis. The effect of cement techniques. Clin Orthop 1997, 338: 94–9
- Saito S, Saito M, Nishina T, Ohzono K, Ono K. Long-term results of total hip arthroplasty for osteonecrosis of the femoral head. A comparison with osteoarthritis. Clin Orthop 1989, 244: 198–207
- Sarmiento A, Ebramzadeh E, Gogan W J, McKellop H A. Total hip arthroplasty with cement. A long-term radiographic analysis in patients who are older than fifty and younger than fifty years. J Bone Joint Surg (Am) 1990; 72: 1470–6
- Walker P S, Mai S F, Cobb A G, Bentley G, Hua J. Prediction of clinical outcome of THR from migration measurements on standard radiographs. A study of cemented Charnley and Stanmore femoral stems. J Bone Joint Surg (Br) 1995; 77: 705–14
- Xenakis T A, Gelalis J, Koukoubis T A, Zaharis K C, Soucacos P N. Cementless hip arthroplasty in the treatment of patients with femoral head necrosis. Clin Orthop 2001, 386: 93–9