Abstract
Background There is no consensus regarding the best treatment for children with late diagnosis of congenital hip dislocation.
Patients and methods This retrospective study involved 29 hips in 22 children (19 girls) with an age range of 3–14 years, who had been operated with various techniques for congenital hip dislocation between 1998 and 2002. 6 patients had right, 9 patients had left, and 7 patients had bilateral congenital hip dislocation. The mean length of follow-up was 3 (1–5) years.
Results While the mean acetabular index was 53°(35–65) preoperatively, at the last follow-up it was 30° (15–50). 27 hips were type 4 and 2 hips were type 3 by Tönnis criteria. Satisfactory reduction (Severin Class I) had been achieved in 19 hips at the follow-up radiography, and they developed no osteonecrosis. The outcome was successful in children under 7 years of age, but problems encountered in those over 7 increased unless sufficient reduction had been achieved.
Interpretation Age at treatment of late-diagnosed congenital hip dislocation appears to be important for outcome.
Although congenital dislocation (CDH) of the hip is a well-researched topic and treatment of the newborn is often successful, it is sometimes diagnosed first in children in early childhood (Ashley et al. Citation1972, Browne Citation1979, Herold and Daniel Citation1979, Kalamchi and MacEven Citation1980, Ryan et al. Citation1998). Soft tissue contractures and dysplastic changes in these cases may lead to avascular necrosis and early osteoarthrosis (Wedge and Wasylenko Citation1979, Ryan et al. Citation1998). However, a definitive treatment protocol has not been established for CDH cases with delayed diagnosis (Massie and Howorth Citation1951, Wilkinson and Carter Citation1960, Gage and Winter Citation1972, Salter and Dubos Citation1974, Schoenecker and Strecker Citation1984, Ryan et al. Citation1998).
The principles of treatment of CDH in childhood differ from those pertaining to infants (Ashley et al. Citation1972, Coleman Citation1978, Berkeley et al. Citation1984, Ryan et al. Citation1998). Muscle contractures around the joint and soft tissue pathology hinder the reduction, and prevent the normal development of the head of the femur by infiicting pressure (Bucholz and Ogden Citation1978, Kalamchi and MacEven Citation1980, Thomas et al. Citation1982, Schoenecker and Strecker Citation1984, Ryan et al. Citation1998). In spite of the attempts to reduce the ischemic changes through various traction methods, there is no definite evidence to support this treatment modality (Wilkinson and Carter Citation1960, Gage and Winter Citation1972, Salter et al. Citation1974, Herold and Daniel Citation1979, Schoenecker and Strecker Citation1984, Ryan et al. Citation1998). Some studies claim that femoral shortening can facilitate reduction and reduce the risk of osteonecrosis (Browne Citation1979, Schoenecker and Strecker Citation1984, Galpin et al. Citation1989, Ryan et al. Citation1998). Schoenecker and Strecker (Citation1984) compared 13 hips with femoral shortening preoperatively with 26 hips that received preoperative traction. 14 of the hips with preoperative traction developed osteonecrosis, while the hips with preoperative femoral shortening did not develop osteonecrosis. Galphin et al. (Citation1989) showed that children who did not receive traction had no risk of osteonecrosis by a one-stage operation. Some authors have claimed that besides open reduction, a one-stage operation must sometimes also include capsuloraphy, femoral shortening, and pelvic osteotomies in the cases that require these types of treatment (Klisic et al. Citation1988, Galpin et al. Citation1989, Karakas et al. Citation1995, Ryan et al. Citation1998). There is limited information available on the long-term functional and radiographic results of these types of operations, however.
We present our functional and radiographic findings in 22 children with delayed diagnosis of CDH who were treated by various acetabuloplasty techniques.
Patients and methods
This study involved 29 hips in 22 children (19 girls) with mean age 8 (3–14) years who were treated for CDH between 1998 and 2002. 6 patients had right CDH, 9 patients had left CDH, and 7 patients had bilateral CDH. The average follow-up time was 38 (12–60) months.
8 patients had preoperative hip pain, and the average fiexion of the hip was 100o (40–110); abduction 35° (10–75); internal rotation 55° (0–105), and external rotation 36° (10–65). All the patients were limping and had positive Trendelenburg finding.
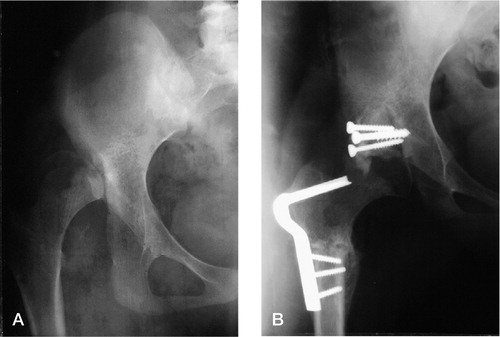
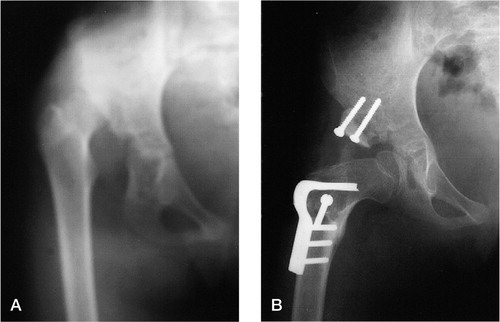
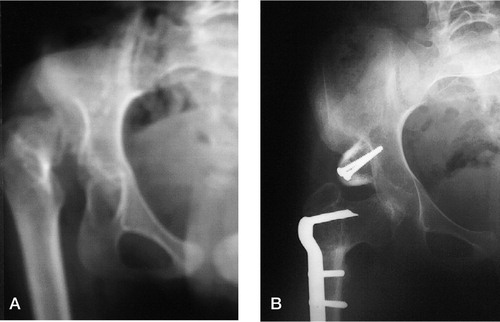
None of the patients had experienced preoperative traction before our treatment. At the beginning of the study, all children were subjected to open reduction and capsuloraphy under general anesthesia in supine position by the Smith Petersen approach. In all cases, following intertrochanteric osteotomy, femoral shortening and derotation were performed by adding varization in those 22 hips requiring it. Taking the state of the acetabulum and the height of the femur into consideration, either Salter′s innominate osteotomy (12 hips) (), extra-articular grafting acetabuloplasty (12 hips) (), Dega osteotomy with extraarticular grafting (4 hips), or Chiari osteotomy (1 hip) was applied. After partial capsule resection and plication, the femoral head was fixed to the acetabulum by a pin in the cases with suspected instability.
Figure 1 Case 10. A girl who was 6 years old at the index operation for bilateral hip dislocation. A. At the initial examination (bilateral hip dislocation). B. 1 year after open reduction, capsulorrhaphy, femoral shortening, and Salter innominate osteotomy, showing adequate reduction. C. After removal of implant.

Figure 2 Case 2. A 12.5-year-old girl at the index operation (A) for dislocation of the right hip and postoperatively (B) after open reduction, capsulorhaphy, extraarticular grafting arthroplasty and femoral shortening, showing adequate reduction.
For all the children, a hip spica cast was applied after the operation. In the fourth week after surgery, the pin was removed. The casts, however, were not removed for an average of 8 weeks. Following the removal of casts, active and passive motion was carried out to increase muscle strength and the movements of the joints. This was done for 6 weeks, during which a Dennis Brown brace was applied. At the end of this procedure, the patients were able to walk by controlled weight bearing. In 15 children, the plates and screws were then removed.
The patients were evaluated functionally and radiographically in the first month, third month, and the sixth month after operation, and at the end of the first year depending on their osseous maturation. Preoperative films were used to determine the degree of depletion of the femoral head with respect to Tönnis (Citation1976) criteria, position of the hip, the acetabular index, and the regularity of the Shenton line. Acetabular index, CE angle of Wiberg, Shenton line, and CCD angle were evaluated on the postoperative radiographs. The limb length discrepancy was assessed on anteroposterior radiographs with the patients in standing position.
The hips were classified into 6 categories according to the Severin (Citation1941) scale. Accordingly, a hip with a center-edge angle of Wiberg (Citation1939) of more than 20 degrees in adults (14 years old or more), and more than 15 degrees in children (6–13 years old) was classified as class 1, which was normal. Class-II hips had a mild deformity of the femoral head or neck, but they were concentrically reduced. The center-edge angle of class II hips was the same as that of class I hips. Class-III hips were dysplastic without subluxation. In class III hips, the center-edge angle was lower than 20 degrees in adults and lower than 15 degrees in children. Class-IV hips were subluxed, and the center-edge angle was 0 degrees or lower. In class-V hips, the femoral head articulated within a neo-acetabulum, whereas class-VI hips were dislocated.
When the hip had a CE angle of greater than 15 degrees, an acetabular index lower than 28 degrees, and an intact Shenton line, it was classified as not dislocated. At least 8 degrees of correction of the dysplastic acetabulum, or an acetabular index lower than 20 degrees on the last radiograph was regarded as sufficient acetabular reconstruction (Ryan et al. Citation1998) ().
Figure 3 Case 7. A 12-year-old girl at the index operation (A) for dislocation of the right hip and after open reduction, capsulorrhaphy, extraarticular grafting arthroplasty and femoral shortening (B), showing adequate reduction.
Degenerative changes were classified according to Boyer et al. (Citation1981) as grade 0 (no degenerative changes), grade I (no more than one cyst or osteophyte, no bone sclerosis, and a normal joint space), grade II (one or few subchondral cysts as well as osteophytes, minimum subchondral sclerosis, and slight narrowing of the joint space), and grade III (multiple subchondral cysts and osteophytes, marked subchondral sclerosis, and moderate to severe narrowing of the joint space). The patients were evaluated according to the Iowa hip score at the last follow-up (Larson Citation1963).
Statistics
Statistical analysis was done to determine the relationship of preoperative, intraoperative and postoperative variables with the final outcome variables. Several factors such as age, postoperative reduction, postoperative Severin grade, Boyer degenerative changes, and osteonecrosis were analyzed statistically in relation to final Iowa score by linear regression analysis. Furthermore, age and functional Iowa score relationship analysis was performed by Mann-Whitney U test.
Results ()
At follow-up all patients were pain-free at rest, used no analgesics and could walk without crutches. The mean fiexion was 105° (70–135), abduction 30° (5–60), internal rotation 35° (0- 50), and external rotation 35° (5–50). 11 of 29 hips had positive Trendelenburg. While the mean limb length discrepancy was 1.2 (0–5.5) cm, only 2 patients had a difference of more than 2 cm in limb length (case no. 11, 4 cm, and case no. 16,5.5 cm).
Table 1. Detailed information about he patients
The skeletal maturation was determined by radiographic examination of the proximal femoral epiphysis and triradiate cartilage; 5 patients had skeletal maturation. While the preoperative mean acetabular index was 53° (35–65), in the last follow-up it was 30° (15–50). 27 hips were type 4, and 2 hips were type 3 according to Tönnis criteria. Satisfactory reduction (Severin class I) was achieved in 19 hips according to the follow-up radiography, and they developed no osteonecrosis ().
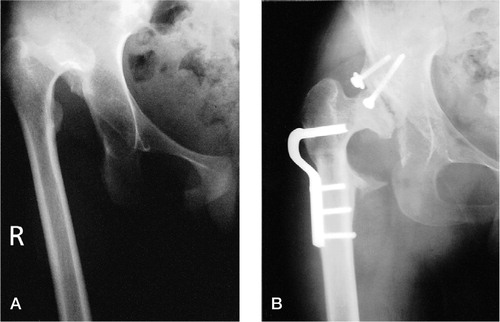
Figure 4 Case 12. A 15-year-old girl at the index operation (A) for dislocation of the right hip and after open reduction (B), capsulorrhaphy, extraarticular grafting arthroplasty and femoral shortening, showing adequate reduction at 28 months of follow-up.
The Shenton line was intact in 26 hips, and the CE angle of Wiberg was increased to 36° (20–60). In the Severin classification, 22 hips were class I, 4 hips were class II, 2 hips were class IV, and 1 hip was class VI. In the Boyer classification of degenerative changes, 18 hips were grade 0, 7 hips were grade I, and 4 hips were grade II.
Of the 10 hips that had insufficient reduction, 3 had a radiographically poor result (Severin class IV-VI), and 4 hips developed osteonecrosis. The mean Iowa score in patients below 7 years old was 95 (84–99) and in patients above 7 years old it was 89 (75–97). Iowa scores for the children who were under 7 years of age at the most recent follow-up, either with unilateral involvement or with bilateral involvement, were better () than those of patients who were over 7 years of age () (Mann-Whitney U test, p = 0.004). According to linear regression analysis presence of postoperative reduction and absence of Boyer degenerative changes were all significantly associated with a better Iowa score at the most recent follow-up examination.
Figure 5 Case 11. A 14-year-old girl at the index operation (A) for dislocation of the right hip and at follow-up (B) after 32 months: dislocation of the hip and heterotopic ossification.
1 of 3 hips with insufficient reduction was reoperated. In the hip that had previously undergone shelf arthroplasty, an open reduction was performed because of redislocation after the removal of the hip spica cast. The patient was assessed as Severin class V. In addition, 3 hips in which the desired outcomes were obtained were manipulated under general anesthesia to overcome the joint stiffness. After manipulation, the desired range of motions of hips was achieved.
Additional complications were implant failure in 1 femur with a removed hip spica cast (no. 10; right hip) and heterotopic ossification in another hip (no. 6; left hip). Case no. 10 was reoperated. In case no. 6, osseous structures prevented hip motion and were excised when the implants were removed. The patient was also given preoperative and postoperative operative radiotherapy but developed heterotopic ossification, and a new operation is planned. In addition, 3 patients had lateral rotational deformity because of excessive derotation ().
Table 2. Complications in the patients
Discussion
The treatment of congenital dislocation of the hip aims at the same outcome for both the older child and the infant, which is reduction of the femoral head into the true acetabulum. However, the age beyond which surgical treatment is contraindicated has been the subject of debate because of the risk of serious complications. The age concerned varies between 6 and 14 years.
Concentric reduction in older children may be a challenge-especially when the femoral head is fiattened or when the acetabulum is dysplastic. Reduction may also be hindered by soft tissue contracture with undue pressure on the femoral head, which increases the risk of poor development of the hip joint and avascular necrosis of the femoral head.
Most authors have evaluated the long-term functional and radiographic outcomes of one-stage open reduction of CDH. While Klisic et al. (Citation1988) obtained a rate of two- thirds good or excellent results of combined operative reduction at 7 years of follow-up, Karakas et al. (Citation1995) achieved the same results after traction and one-stage open reduction. However, Ryan et al. (Citation1998) reported good or excellent results in 16 of 18 children between 3 and 14 years of age after one-stage reduction. On the other hand, these authors obtained increasingly poor results in children above 3 years of age who had undergone pelvic osteotomies, hindered by insufficient remodeling capacity of the acetabulum.
In CDH cases in our series with an age range of 3–14 years, we performed various surgical interventions. The type of surgery was based on the preoperative evaluations of the pathologies as well on as our observations intraoperatively. We achieved good results after concentric reduction. However, for the cases in which concentric reduction was neither achieved nor could be sustained, the older age seemed to have a significant effect on the prognosis. While the patients under 7 years of age with previously insufficient reductions had good radiographic results, the patients 7 years of age and older presented poor results, and thus required reoperation. This contrasts with the report of Massie and Howarth (Citation1951) and Williamson et al. (Citation1989), who claimed that the age of the patient does not have any effect on the results.
While osteonecrosis was more prevalent among the patients with insufficient reduction, more femoral shortening not only reduced the risk of osteonecrosis but also facilitated better reduction. Thus, increased femoral shortening proved a superior method. Furthermore, preoperative traction did not increase the risk of osteonecrosis.
In the patients with severely dysplastic acetabulum whose diagnosis had been established through preoperative radiographic studies, we performed shelf arthroplasty through extraarticular grafting to increase the degree of reduction via increased acetabular volume. However, apart from the failure in providing total concentric reduction and stability in these patients, the external rotation deformity in gait due to over-derotation was another problem.
Some authors have considered that femoral osteotomy, or any combination involving shortening, varus osteotomy, or derotation osteotomy combined with open reduction, capsuloraphy, and possibly pelvic osteotomy can be conducted safely in one stage. As shown in the study of Galpin et al. (Citation1989), despite being complicated in one-stage applications, this procedure is a safe and effective method.
- Ashley R K, Larsen L J, James P M. Reduction of dislocation of the hip in older children. A preliminary report. J Bone Joint Surg (Am) 1972; 54: 545–50
- Berkeley M E, Dickson J H, Cain T E, Donovan M M. Surgical therapy for congenital dislocation of the hip in patients who are twelve to thirty-six months old. J Bone Joint Surg (Am) 1984; 66: 412–20
- Boyer D W, Mickelson M R, Ponseti I V. Slipped capital femoral epiphysis. Long-term follow-up study of one hundred and twenty-one patients. J Bone Joint Surg (Am) 1981; 63: 85–95
- Browne R S. The management of late diagnosed congenital dislocation and subluxation of the hip. With special reference to femoral shortening. J Bone Joint Surg (Br) 1979; 61: 7–12
- Bucholz R W, Ogden J A. Patterns of ischemic necrosis of the proximal femur in nonoperatively treated congenital hip disease. The hip. Proceedings of the Sixth Open Scientific Meeting of The Hip Society. The C. V. Mosby Company, St. Louis 1978; 43–63, In
- Coleman S S. Congenital dysplasia and dislocation of the hip. The C. V. Mosby Company, St. Louis 1978; 95–154
- Gage J R, Winter R B. Avascular necrosis of the capital femoral epiphysis as a complication of closed reduction of congenital dislocation of the hip. A critical review of twenty years′ experience at Gillette Children′s Hospital. J Bone Joint Surg (Am) 1972; 54: 373–88
- Galpin R D, Roach J W, Wenger D R, Herring J A, Birch J G. One-stage treatment of congenital dislocation of the hip in older children, including femoral shortening. J Bone Joint Surg (Am). 1989; 71: 734–41
- Herold H Z, Daniel D. Reduction of neglected congenital dislocation of the hip in children over the age of six years. J Bone Joint Surg (Br) 1979; 61: 1–6
- Kalamchi A, MacEven G D. Avascular necrosis following treatment of congenital dislocation of the hip. J Bone Joint Surg (Am) 1980; 62: 876–88
- Karakas E S, Baktir A, Argun M, Turk C Y. One-stage treatment of congenital dislocation of the hip in older children. J Pediatr Orthop 1995; 15(3)330–6
- Klisic P, Jankovic L, Basara V. Long-term results of combined operative reduction of the hip in older children. J Pediatr Orthop 1988; 8(5)532–4
- Larson C B. Rating scale for hip disabilities. Clin Orthop 1963; 31: 85–96
- Massie W K, Howorth M B. Congenital dislocation of the hip. Part II. Results of open reduction as seen in early adult period. J Bone Joint Surg (Am) 1951; 33: 171–90
- Ryan M G, Johnson L O, Quanbeck D S, Minkowitz B. One-stage treatment of congenital dislocation of the hip in children three to ten years old. Functional and radiographic results. J Bone Joint Surg (Am) 1998; 80: 336–44
- Salter R B, Dubos J P. The first fifteen years′ personal experience with innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip. Clin Orthop. 1974; 98: 78–103
- Schoenecker P L, Strecker W B. Congenital dislocation of hip in the children. Comparison of the effects of femoral shortening and of skeletal traction in the treatment. J Bone Joint Surg (Am) 1984; 66: 21–7
- Severin E. Contribution of the knowledge of congenital dislocation of the hip joint. Late results of closed reduction and arthrographic studies of recent cases. Acta Chir Scand 1941, (Suppl 63)
- Thomas C L, Gage J R, Odgen J A. Treatment concepts for proximal femoral ischemic necrosis complicating congenital hip disease. J Bone Joint Surg (Am) 1982; 64: 817–28
- Tönnis D. Normal values of the hip joint for the evaluation of x-rays in children and adults. Clin Orthop. 1976; 119: 39–47
- Wedge J H, Wasylenko M J. The natural history of the congenital disease of the hip. J Bone Joint Surg (Br) 1979; 61: 334–8
- Wiberg G. Relation between congenital subluxationof the hip and arthritis deformans (roentgenological study). Acta Orthop Scand 1939; 10: 351
- Wilkinson J, Carter C. Congenital dislocation of the hip. The results of conservative treatment. J Bone Joint Surg (Br) 1960; 42: 669–88
- Williamson D M, Glover S D, Benson M K. Congenital dislocation of the hip presenting after the age of three years. A long-term review. J Joint Surg (Br) 1989; 71: 745–51

