Abstract
Background A periosteal flap is frequently used in procedures involving repair of articular cartilage defects. Hypertrophy of the repair tissue, probably from a retained periosteum, is a clinical problem but not much is known about this issue. The objective of the present experimental study was to investigate the retention rate of periosteal flaps with respect to various postoperative mobilization regimes and the introduction of bone marrow elements underneath the flap.
Method We created a chondral lesion (diameter 4 mm) in both patellas of 18 New Zealand white rabbits. The subchondral bone was left intact in one knee. In the other, the bone plate was perforated, allowing bone marrow elements to enter the defect. All defects were covered with a periosteal flap, sutured and glued to the rim of the cartilage defect. Postoperatively, the rabbits were allocated to one of three groups: A. rehabilitation in cages for 4 days, then killed; B. rehabilitation in cages for 7 days, then free activity on the floor of a 10 m2 room until the end of the second week, then killed; C. rehabilitation in cages for 2 weeks, then killed.
Results 16 of 23 periosteal flaps became detached within 2 weeks (one knee was excluded because of clinical signs of infection), with no difference in the retention rate with respect to mobilization regime or established access to bone marrow elements in the defect. The periosteum still served as a cover of the defect in 10 of 12 knees at day 4. This figure decreased to 7 of 23 knees at day 14.
Conclusion Our study is the first to document the retention rate of periosteal flaps in a rabbit model. The low retention rate observed may explain why periosteal hypertrophy is not reported in experimental studies where the periosteal flap is sutured to the cartilage rim.
Of all knees subjected to arthroscopy, a focal full-thickness cartilage lesion larger than 1 cm2graded as ICRS grade 3 and 4 is detected in 5–7% (Hjelle et al. Citation2002, Aroen et al. Citation2004). Although according to current clinical practice only a few of these may need surgery, a continuous research is going on worldwide to establish the proper procedure to obtain healing of the chondral defect. Generally, most experimental models of cartilage repair include a full thickness defect (ICRS grade 4) in which the subchondral bone is completely removed when inducing the lesion (ICRS Citation1998). However, the original experimental studies on chondrocyte transplantation with a periosteal flap as cell sealing used an approach in which the subchondral bone is preserved in the lesion (Grande et al. Citation1989, Brittberg et al. Citation1996, Breinan et al. Citation1997). This was graded as ICRS grade 3. The principal methodological difference in creating the surgical defect may to some extent explain the variable outcome observed with the use of periosteum graft (Aroen et al. Citation1998). The use of periosteum as coverage of the defect in autologous chondrocyte implantation in patients is associated with need of trimming or debridement in 25% of cases at second-look arthroscopy, due to hypertrophy of the repair tissue (Knutsen et al. Citation2004). Such hypertrophy has not yet been reported in experimental studies on pure cartilage defects. Moreover, in a clinical prospective study Niekerk and coworkers (Citation2000) reported that 25% of the periosteal flaps totally detach or partially delaminate within 2 weeks of surgery. The retention rate of periosteal flaps in a rabbit model is not known, but has been assessed in the current study and related to the presence or absence of bone marrow elements underneath the periosteal sealant. The rationale for this latter aspect is that bone marrow elements at the base of the cartilage defect may increase adhesion of the periosteal flap through the effect of fibrin, thus increasing the retention rate of the flaps. Another issue that has been investigated in our study is the influence of postoperative mobilization of the experimental animals on the retention rate of the periosteal flaps. Apart from the extensive documentation on the effect of continuous passive motion (CPM), this question has not been thoroughly addressed (Salter Citation1989). Only one recent study on goat knees has focused on this issue, concluding that some degree of immobilization is needed in order to avoid immediate detachment of the flaps from cartilage defects (Driesang and Hunziker Citation2000).
Animals and methods
A defect was created in the patella of both knees in 18 22-week-old New Zealand white rabbits, at time zero. We chose the patella as the site of the lesion for two reasons; firstly, the patella has the thickest cartilage of all rabbit joints, and secondly, it has been used in the experimental work with the autologous chondrocyte implantation technique. The rabbits, weighing 3.6–4.0 kg, were allowed to acclimatize for 2 weeks before surgery. They were kept in cages with floor area 62 × 64 cm, and height 41 cm, room temperature 18.5°C, and artificial light with 12-h day and night cycles. The animals were fed 150 g of standard diet daily, with free access to water. The surgery was performed under anesthesia consisting of a mixture of Hypnorm and Dormicum with dosages adjusted according to the weight of the animals. 1.5 mL of local anesthesia (Marcain) with epinephrine was injected locally at the edges of the wound at the start of surgery. Antibiotic (Vibramycin) was given orally as prophylaxis preoperatively and postoperatively for 5 days, together with Temgesic (buprenorphinum) subcutaneously as pain relief. Medial parapatellar incisions were made in the skin and a capsular incision was performed just medial to the patella, taking care to leave a small cuff of fascia attached to the patella to permit a strong capsular closure. The patella was dislocated laterally and inverted. A 4-mm diameter biopsy punch was used to induce the cartilage lesions. Experienced surgeons specially trained in the procedure of harvesting periosteum and performing cartilage repair procedures in rabbits performed all the surgery. A pilot study showed that using this technique bilaterally does not cause any observational impairment of function compared to rabbits undergoing only a unilateral procedure.
We used dental instruments and a stereoscopic microscope to secure removal of all the cartilage in the defect down to the subchondral bone plate. Care was taken to avoid any damage of the subchondral bone plate. The wound was closed with sutures in the fascia and intracutaneous suture. 2 weeks later, the defects were repaired by rearthrotomy. Once again, the defects were debrided with dental instruments under a stereo microscope. The defect in one of the knees was randomized to undergo drilling of the subchondral bone plate. 4 drill holes (0.6 mm diameter) were made by a hand-driven burr. In the contralateral knee, the subchondral bone plate in the defect was left intact. A periosteal flap was harvested from the medial part of the proximal tibia in both knees and placed over the defect with the cambium layer facing down. Subsequently, the flaps were sutured with four or five 9.0 sutures to the rim of the defect, and glued with Tisseal glue. In addition, an extra periosteal explant of each knee was harvested in 6 rabbits to confirm the presence of a cambium layer and for evaluation of the thickness of the harvested periosteum. The periosteal explants selected for this measurement, were mounted on a cork plate and fixed in sodium phosphate-buffered 4% paraformaldehyde (pH 7.4). After embedding in paraffin wax, the specimens were sectioned perpendicular to the surface of the periosteum. Two sections of each periosteal explant were made. A semiautomatic interactive image analysis system (Analysis Soft Imaging System, Münster, Germany) was used to measure the cambium layer, the fibrous layer, and total thickness of the explants at three random sites to estimate the thickness of the sutured periosteum flaps. Postoperatively, the rabbits were allocated to one of three groups as follows: A) rehabilitation in cages for 4 days, then killed; B) rehabilitation in cages for 7 days, then free activity on the floor of a 10 m 2room until the end of the second week, then killed; C) rehabilitation in cages for 2 weeks, then killed.
The knees were evaluated macroscopically at killing and evaluated for signs of degeneration. The patellar lesion was inspected and the periosteal flaps were classified as being attached or not. A digital camera was used to document the observations concerning each patella. To assess the presence of remaining native cartilage in the patellar defects histologically, a semiquantitative grading system was used.
The experiment was performed according to the guidelines for animal research at the University of Oslo and approved by the Norwegian Government Committee for Experimental Animal Care.
Statistics
The retention rates of the periosteal flaps were evaluated according to whether or not they were attached to the defect. Comparison of the retention rate of the periosteal flap between defects with and without drill holes was done with a paired Student t-test. In comparison of the different rehabilitation groups A, B and C, one-way ANOVA was used to compare the means of retention rate among the three groups. To analyze the difference in retention of periosteal flaps between groups B and C, an unpaired t-test was used. P-values < 0.05 were considered significant.
Results
4 days postoperatively, 10 of 12 periosteal flaps were still attached to the defect (group A). This observation was different from those for groups B and C (p = 0.009). At 2 weeks, a retention rate of 7 of 23 was found (). 3 of the detached periosteal flaps were found at the patellar recess attached to the synovium. No macroscopic signs of inflammation nor any tendency to loose body formation were seen. One knee was excluded from the evaluation at 2 weeks due to infection.
Table 1. Number of retained periosteum flaps
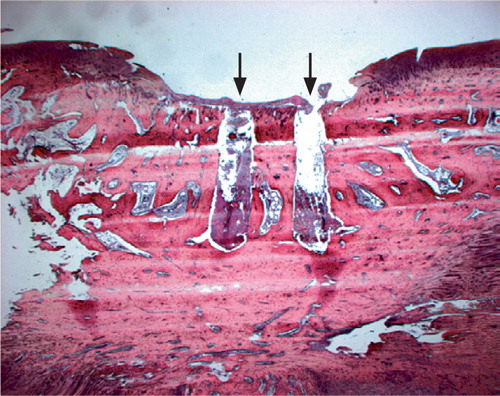
After 2 weeks, a thin film of gelatinous tissue could be seen in the defect macroscopically, though histologically these defects were empty ().
Figure 1 Histology from the cartilage defect after two weeks. The periosteal flap is detached from the cartilage defect and only a loose fibrous tissue remains in the defect. Arrows illustrate the penetration of the subchondral bone plate into the bone marrow from the hand-drive drill (HE, × 1.25).
We found no difference in retention rates between the two groups with different postoperative rehabilitation for two weeks (B and C) (p = 0.8, ); nor was there any difference in activity or locomotion pattern observed in comparison with animals subjected to unilateral knee surgery in ongoing experiments in our laboratory.
The number of retained flaps was similar regardless of whether there was access to bone marrow elements (9/18) or not (8/17) underneath the periosteal flaps (p = 0.3). Degenerative changes in adjacent articular cartilage were not noted in any of the knees macroscopically.
With one exception, the cambium layer () was identified in all samples and subjected to histologic analysis (n = 12).
Figure 2 Illustration of a harvested periosteal flap with the different layers of interest marked. A shows fibrous layer, B shows cambium layer and C shows the total thickness of the periosteal flap. Arrow marked D shows extra tissue neither belonging to the fibrous layer nor the cambium layer (HE, × 5).
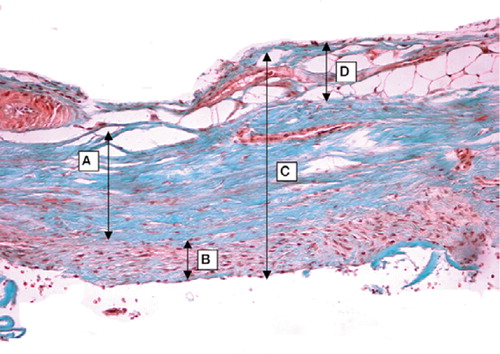
Periosteal explants showed a mean thickness of 375 μm and about 15% of this consisted of tissue not belonging to either the fibrous or the cambium layer. Articular cartilage of the patella measured at the edge of the defect showed a mean thickness of 432 μm ().
Table 2. Thickness (μm) of harvested periosteal flaps (n = 12) and the articular cartilage thickness of patella (n = 12). The cartilage thikness of patella was measured as the mean distance from the tidemark to surface at the edges of the defect
Discussion
We found that two-thirds of the sutured periosteal flaps had detached from the defect between 4 and 14 days postoperatively, irrespective of whether bone marrow elements were allowed access to the defect or not. A high rate of loosening has also been observed in a goat model (Driesang and Hunziker Citation2000). Loosening occurred irrespective of whether there was a restricted or free postoperative mobilization regime. Mechanical stimulation is considered important for the development of a functional repair tissue. Thus, a certain amount of mobilization seems to be beneficial to enhance the differentiation towards an ordinarily structured articular cartilage tissue (Alfredson and Lorentzon Citation1999, Saris et al. Citation1999, Espanha et al. Citation2001). Restricted mobilization of the joint may result in longer survival of the flaps (Driesang and Hunziker Citation2000). On the other hand, joint immobilization has harmful effects on both periarticular tissue and cartilage (Hung et al. Citation1997).
The retention rate of the periosteal flaps is an important parameter when deciding the postoperative mobilization regime. Earlier studies have indicated that the thickness of periosteal flap may be a decisive factor for the loosening rate and have pointed out the importance of specific training in the harvesting of periosteal flaps (O′Driscoll and Fitzsimmons Citation2000). Our measurements of the thickness of the periosteal flaps show that our flaps were somewhat thicker than in previously published studies (O′Driscoll et al. Citation2001). In addition to the fibrous and cambium layers, our samples included some extra tissue which amounted to approximately 15% of the total thickness of the periosteal explants. Measurements of harvested periosteal flaps have been performed both in goats and rabbits, and approximately the same thickness has been observed in both species (Driesang and Hunziker Citation2000, O′Driscoll et al. Citation2001). Although in relation to the thickness of the articular cartilage the periosteum is much thinner in goats than in rabbits, a high loosening rate was still observed. Loosening has also been reported in human series where 25% were partially or completely detached from the defect within 2–3 weeks postoperatively (Niekerk et al. Citation2000). Our study is the first to document that nearly all periosteal flaps (10/12) are attached to the defect for 4 days or more, and it is questionable whether the retention of the periosteal flap for more than 4 days is needed for retaining the cells in the defect when cells are transplanted under such a flap. In fact, a recent study stated that nine-tenths of the chondrocytes were attached to bone or cartilage surfaces already after 24 h (Wang and Kandel Citation2004).
Two clinical studies have reported the need to remove so-called overgrowth of repair tissue postoperatively following autologous chondrocyte transplantation under a periosteal flap (Peterson et al. 2002, Knutsen et al. 2004). This hypertrophy of the repair tissue is believed to be the remnants of the periosteal flap and is regularly observed at second-look arthroscopy (Peterson et al. Citation2002). This kind of overgrowth has not been seen experimentally, except in one study where a 3-mm depth osteochondral lesion of the patella was used with transosseous suturing of the periosteal flap (Car-ranza-Bencano et al. Citation1999). A possible explanation for the difference between results in experimental and clinical studies in this regard may be that the periosteal coverage detaches after a relatively short period of time in the experimental models. This may be an advantage for the cartilage repair process, in order to avoid the hypertrophic response of the periosteal flap. As far as we know, in clinical or experimental studies using this technique, there have been no reports showing that by detaching periosteum forms a loose body. However, further experimental studies comparing periosteum to alternative ways of shielding or implanting the cells in the cartilage defect seem to be warranted in order to establish an optimal procedure.
The low retention rate of periosteal flaps shown in our study should be considered when designing future investigations with cell transplantation to restore cartilage tissue.
No competing interests declared.
- Alfredson H, Lorentzon R. Superior results with continuous passive motion compared to active motion after periosteal transplantation. A retrospective study of human patella cartilage defect treatment. Knee Surg Sports Traumatol Arthrosc 1999; 7: 232–8
- Aroen A, Jones D G, Fu F H. Arthroscopic diagnosis and treatment of cartilage injuries. Sports Med Arthrosc Rev 1998; 6: 31–40
- Aroen A, Loken S, Heir S, Alvik E, Ekeland A, Granlund O G, Engebretsen L. Articular Cartilage Lesions in 993 Consecutive Knee Arthroscopies. Am J Sports Med 2004; 32: 211–5
- Breinan H A, Minas T, Hsu H P, Nehrer S, Sledge C B, Spector M. Effect of cultured autologous chondrocytes on repair of chondral defects in a canine model. J Bone Joint Surg (Am) 1997; 79: 1439–451
- Brittberg M, Nilsson A, Lindahl A, Ohlsson C, Peterson L. Rabbit articular cartilage defects treated with autologous cultured chondrocytes. Clin Orthop 1996;, 326: 270–83
- Carranza-Bencano A, Perez-Tinao M, Ballesteros-Vazquez P, Armas-Padron J R, Hevia-Alonso A, Crespo F M. Comparative study of the reconstruction of articular cartilage defects with free costal perichondrial grafts and free tibial periosteal grafts: An experimental study on rabbits. Calcif Tissue Int 1999; 65: 402–7
- Driesang I M K, Hunziker E B. Delamination rates of tissue flaps used in articular cartilage repair. J Orthop Res 2000; 18: 909–11
- Espanha M M, Lammi P E, Hyttinen M M, Lammi M J, Helminen H J. Extracellular matrix composition of full-thickness defect repair tissue is little influenced by exercise in rat articular cartilage. Connect Tissue Res 2001; 42: 97–109
- Grande D A, Pitman M I, Peterson L, Menche D, Klein M. The Repair of Experimentally Produced Defects in Rabbit Articular-Cartilage by Autologous Chondrocyte Transplantation. J Orthop Res 1989; 7: 208–18
- Hjelle K, Solheim E, Strand T, Muri R, Brittberg M. Articular cartilage defects in 1,000 knee arthroscopies. Arthroscopy 2002; 18: 730–4
- Hung S C, Nakamura K, Shiro R, Tanaka K, Kawahara H, Kurokawa T. Effects of continuous distraction on cartilage in a moving joint: An investigation on adult rabbits. J Orthop Res 1997; 15: 381–90
- Knutsen G, Engebretsen L, Ludvigsen T C, Drogset J O, Grontvedt T, Solheim E, Strand T, Roberts S, Isaksen V, Johansen C. Autologous chondrocyte implantation compared with microfracture in the knee - A randomized trial. J Bone Joint Surg (Am) 2004; 86: 455–64
- Niekerk van L J A, Richardson J B, Rees D. What happens to the periosteal patch within the first three weeks of implantation. ICRS newsletter 2000, Gothenburg issue
- O′Driscoll S W, Fitzsimmons J S. The importance of procedure specific training in harvesting periosteum for chondrogenesis. Clin Orthop 2000, 380: 269–78
- O′Driscoll S W M, Saris D B F, Ito Y, Fitzimmons J S. The chondrogenic potential of periosteum decreases with age. J Orthop Res 2001; 19: 95–103
- Peterson L, Brittberg M, Kiviranta I, Akerlund E L, Lindahl A. Autologous chondrocyte transplantation - Biomechanics and long-term durability. Am J Sports Med 2002; 30: 2–12
- Salter R B. The biologic concept of continous passive motion of synovial joints - the 1st 18 years of basic research and its clinical- application. Clin Orthop 1989;, no.??: 12–25
- Saris D B F, Sanyal A, An K N, Fitzsimmons J S, O′Driscoll S W. Periosteum responds to dynamic fluid pressure by proliferating in vitro. J Orthop Res 1999; 17: 668–77
- The cartilage standard evaluation form/knee. ICRS newsletter issue spring, 1998; 98: 5–8
- Wang H J, Kandel R A. Chondrocytes attach to hyaline or calcified cartilage and bone. Osteoarthritis Cartilage 2004; 12: 56–64