Abstract
Introduction Os acromiale is a rare anatomical condition; its incidence in cadaver studies has been found to be approximately 8%. In this retrospective study we investigated the incidence and types of os acromiale in patients with rotator cuff tears.
Methods We assessed operation notes and axillary radiographs for the presence and the type of os acromiale in 1 000 consecutive patients with open rotator cuff repairs.
Results 62 patients (6.2%) showed an os acromiale in the axillary radiographs. In 6 of these the os acromiale was not described in the operation notes. 57 os meso-acromiale and 5 os pre-acromiale were found. The average number of tendons involved in the cuff tear was the same (1.4) in patients with and without os acromiale. The average age of patients with os acromiale was 55 years, and 56 years in patients without os acromiale.
Interpretation Os acromiale is a co-condition in patients with rotator cuff tear. The prevalence of os acromiale in patients with rotator cuff tear is similar to that in a standard population with unknown integrity status of the rotator cuff. Thus, it seems debatable whether an os acromiale is a pathological condition leading to rotator cuff tears.
Os acromiale is the result of a failed fusion of the epiphysis of the anterior part of the acromion after the age of 22–25 years (McClure and Raney Citation1975). There are 3 types of os acromiale: the pre-acromion, the meso-acromion (commonest) and the meta-acromion (Macalister Citation1893) (). The literature mainly describes os meso-acromiale and os pre-acromiale (Burkhart 1992, Hutchinson and Veenstra Citation1993, Jerosch et al. Citation1994, Richman et al. Citation1997, Hertel et al. Citation1998, Warner et al. Citation1998, Satterlee Citation1999, Wright et al. Citation2000, Boehm et al. Citation2003) Warner et al. (Citation1998) reported the treatment of 3 symptomatic os meta-acromiale. The reported incidence of os acromiale ranges from 1% to 15% ().
Figure 1a. Axillary radiograph of a left shoulder with an os pre-acromiale. The black arrow indicates the non-ossified gap between the os pre-acromiale and the acromion.
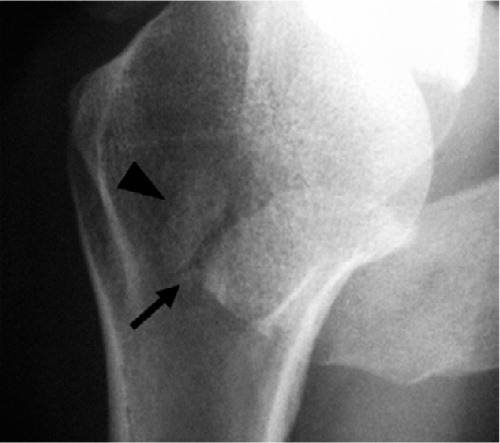
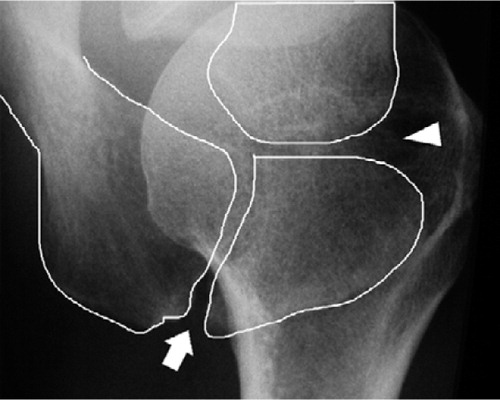
Figure 1b. Axillary radiograph of a right shoulder with an os meso-acromiale. The white arrow indicates the non-ossified gap between the os meso-acromiale and the acromion.

Figure 1c. Axillary radiograph of a right shoulder with an os meta-acromiale. The white arrow indicates the non-ossified gap between the os meta-acromiale and the acromion.

Table 1. Literature review of the incidence of os acromiale
Os acromiale is quite apparent on axial radiographs (Liberson Citation1937), in CT (Grasso Citation1992) and MRI (Park et al. Citation1994). Recently, Gumina et al. (Citation2003) reported that in most patients with os acromiale the distance of the acromioclavicular AC joint to the anterior edge of the acromion is larger than in a normal population, and described 3 types of relationship between os acromiale and the AC joint.
As a single condition, an os acromiale is rarely diagnosed. It is usually associated with subacromial impingement (Hutchinson and Veenstra Citation1993, Jerosch et al. Citation1994) or rotator cuff tears (Mudge et al. Citation1984, Park et al. Citation1994, Boehm et al. Citation2003). Mudge et al. (Citation1984) have been the only authors to report the incidence of os acromiale in patients with rotator cuff tears, and found 9 os acromiale in 145 patients (6%).
The purpose of our retrospective study was to investigate the coincidence of os acromiale and rotator cuff tears. We examined differences in the number of tendons involved in the rotator cuff tears in patients with and without os acromiale, and performed a surgical and radiographic assessment of the position of the os acromiale relative to the AC joint.
Materials and methods
Between 1990 and 2000, 1 091 patients with 1 156 rotator cuff tears underwent open rotator cuff repair in our department. In 1 000 of these shoulders, the axillary radiographs (obtained by positioning the arm in 70° of abduction on a standardized frame with the beam directed superiorly toward the radiographic cassette and a focus-film distance of 100 cm) were suitable to allow the diagnosis of an os acromiale. These radiographs were reviewed together with the operation notes of the patients. 156 cases did not fulfill the study criteria, either because no radiographs were stored in our institution (123) or the quality of the films obtained was not good enough for proper analysis (33).
We recorded the age and sex of the patient, side, size of the rotator cuff tear, stability and type of the os acromiale, and also the location of the AC joint in relation to the os acromiale. Using the axillary radiographs, the type of os acromiale and its position relative to the AC joint were assessed according to the method of Gumina et al. (2003). This was done together by the two of the authors (TDB and WK).
Statistics
The modified chi-square test for independent samples was used to demonstrate the differences between shoulders with and without os acromiale, and between men and women. The Man-Whitney-U test was used to calculate the age differences between the group with and without os acromiale because of the very different sample sizes.
Results
An os acromiale was found on the axillary radiographs in 62 shoulders (6.2%). 5 were os preacromiale and 57 were os meso-acromiale. Os meta-acromiale was not found. The average age of patients without os acromiale was 55 years, and it was 56 years for patients with os acromiale (p = 0.9). Of the 938 shoulders with rotator cuff tear but without os acromiale, 259 (28%) were female cases and 679 (72%) were male. In the 62 shoulders with os acromiale, 17 were female cases and 45 were male. Altogether, 17 of 276 women (6%) and 45 of 724 men (6.2%) had an os acromiale. The average number of tendons involved in the cuff tear was 1.43 in patients without os acromiale and 1.45 in patients with os acromiale (p = 0.4; ).
Table 2. Numbers of tendons involved in the rotator cuff tear in patients with and without os acromiale
Our interpretation of the axillary radiographs according to Gumina et al. (Citation2003) revealed the following relationships between the AC joint and acromion tip in 62 patients with os acromiale: square type 1, intermediate type 2 and cobra-type 13. 46 of the os acromiale (5 os pre-acromiale and 41 meso-acromiale) could not be classified in this context. The typical radiographic appearance of an os meso-acromiale was when the distance of the AC joint facet was located less than 5 mm from the acromial tip (intermediate type) and when the non-ossified gap of the os acromiale ended within the AC joint (cobra type) ().
Figure 2. Axillary radiograph of a right shoulder with an os meso-acromiale. The white arrow indicates the non-ossified gap between the os meso-acromiale and the acromion; the white arrowhead indicates the AC joint. The non-ossified gap between the os meso-acromiale and the acromion ends within the AC joint and the articular facet is not 5–10 mm posterior to the anterior margin.
Discussion
Os acromiale has been reported to be the cause of shoulder pain. The reported incidences in anatomical and radiographic studies range from 1% (Liberson Citation1937) to 15% (Macalister Citation1893). We have found only two reports about the percentage of os acromiale in symptomatic patients. Mudge et al. (1984) reported a figure of 6% in patients with rotator cuff tears (the same as we found), and Jerosch et al. (1994) reported 10% in patients with subacromial impingement without rotator cuff tears. As the incidence of os acromiale in the most recent skeleton studies was 8% (Edelson et al. 1993, Nicholson et al. 1996, Sammarco Citation2000), it seems unlikely that os acromiale has a pathological effect on rotator cuff diseases. This should be considered in preoperative decision making in rotator cuff surgery, especially as the fusion of os acromiale after rotator cuff repair has not shown superior clinical results as compared to acromioplasty and unsuccessful fusion (Boehm et al. 2003).
We found that the presence of an os acromiale did not influence the number of tendons involved in the rotator cuff tear. Sammarco (Citation2000) has reported that os acromiale is more frequent in men than in women, but this could not be confirmed in our study. This difference may be due to the different kind of study population: we examined a regional caucasian population and Sammarco (Citation2000) studied a mixed population in the USA and found a significantly higher incidence of os acromiale in blacks (13%) than in whites (6%). Thus, possible racial and topographic effects on the incidence of os acromiale must be considered. Gruber (Citation1863) and Becker (Citation1934) reported incidences in a population with similar topography to be 3% and 7%, respectively. The relationship between the os acromiale and the AC joint position described by Gumina et al. (2003) could not be confirmed in our study, because two-thirds of the os mesoacromiale could not be classified into one of the 3 groups reported by Gumina et al. In our combined radiographic and surgical analysis of os acromiale and in all os meso-acromiale recognized during surgery, we found that the non-ossified gap of the os acromiale ended within the AC joint, but only one quarter of these could be classified radiographically as a cobra-shaped acromion (the only type in the classification of Gumina et al. (2003) where the os acromiale ends within the AC joint). Thus, a pure radiographic assessment of the relationship between the os acromiale and the AC joint position, as proposed by Gumina et al. (2003), seems to allow misinterpretations. We therefore hesitate to draw conclusions based on this classification in a clinical setting.
- Becker F. Os acromiale und seine Differentialdiagnose. Fortschr Geb Roentgen 1934; 49: 135–42
- Boehm T D, Matzer M, Brazda D, Gohlke F E. Os acromiale associated with tear of the rotator cuff treated operatively. Review of 33 patients. J Bone Joint Surg (Br) 2003; 85: 545–9
- Burkhart S S. Os acromiale in a professional tennis player. Am J Sports Med 1992; 20: 483–4
- Edelson J G, Zuckerman J, Hershkovitz I. Os acromiale: anatomy and surgical implications. J Bone Joint Surg (Br) 1993; 75: 551–5
- Grasso A. The incidence and role of the os acromiale in the acromiohumeral impingement syndrome. Radiol Med (Torino) 1992; 84: 567–70
- Gruber W. Über die Arten der Acromialknochen und accidentellen Acromialgelenke. Arch Anat Physiol und Wissensch Med 1863; 373–87
- Gumina S, De Santis P, Salvatore M, Postacchini F. Relationship between os acromiale and acromioclavicular joint anatomic position. J Shoulder Elbow Surg 2003; 12: 6–8
- Hertel R, Windisch W, Schuster A, Ballmer F T. Transacromial approach to obtain fusion of unstable os acromiale. J Shoulder Elbow Surg 1998; 7: 606–9
- Hutchinson M R, Veenstra M A. Arthroscopic decompression of shoulder impingement secondary to os acromiale. Arthroscopy 1993; 9: 28–32
- Jerosch J, Steinbeck J, Strauss J M, Schneider T. Arthroscopic subacromial decompression—indications in os acromiale?. Unfallchirurg 1994; 97: 69–73
- Liberson F. Os acromiale-a contested anomaly. J Bone Joint Surg (Am) 1937; 19: 683–9
- Macalister A. Notes on the acromion. J Anat and Physiol 1893; 27: 245–51
- McClure J G, Raney R B. Anomalies of the scapula. Clin Orthop 1975; (110): 22–31
- Mudge M K, Wood V E, Frykman G K. Rotator cuff tears associated with os acromiale. J Bone Joint Surg (Am) 1984; 66: 427–9
- Nicholson G P, Goodman D A, Flatow E L, Bigliani L U. The acromion: morphologic condition and age-related changes. A study of 420 scapulas. J Shoulder Elbow Surg 1996; 5: 1–11
- Park J G, Lee J K, Phelps C T. Os acromiale associated with rotator cuff impingement: MR imaging of the shoulder. Radiology 1994; 193: 255–7
- Richman N, Curtis A, Hayman M. Acromion-splitting approach through an os acromiale for repair of a massive rotator cuff tear. Arthroscopy 1997; 13: 652–5
- Sammarco V J. Os acromiale: frequency, anatomy, and clinical implications. J Bone Joint Surg (Am) 2000; 82: 394–400
- Satterlee C C. Successful osteosynthesis of an unstable mesoacromion in 6 shoulders: a new technique. J Shoulder Elbow Surg 1999; 8: 125–9
- Warner J J, Beim G M, Higgins L. The treatment of symptomatic os acromiale. J Bone Joint Surg (Am) 1998; 80: 1320–6
- Wright R W, Heller M A, Quick D C, Buss D D. Arthroscopic decompression for impingement syndrome secondary to an unstable os acromiale. Arthroscopy 2000; 16: 595–9