Abstract
Background In neuromuscular diseases, limb lengthening and foot deformity correction are associated with a high risk of complications associated with distraction callus and joint contracture. We have found no published articles of tibial lengthening and concomitant foot deformity correction using the Ilizarov method or traditional methods. To compare result of gradual distraction with triple arthrodesis for foot deformity combined with tibial lengthening, we investigated healing index and complications of two methods.
Patients and methods We reviewed 14 patients with permanent deformity after poliomyelitis who underwent tibial lengthening and concomitant foot deformity correction using the Ilizarov external fixator. Tibial lengthening over an intramedullary nail was performed in 3 patients and lengthening without a nail was performed in 11 patients.
Results The mean external fixation time was 6 (3.6- 10) months without nail and 1.6 (1.5-1.7) months with nail, whereas the mean healing index was 1.8 (0.8-3.1) months/cm without nail and 2 (1.8-2.3) months/cm with nail. Concomitant foot treatments included triple arthrodesis in 7 patients, pantalar arthrodesis in 2 patients with fiail ankle, and gradual foot frame distraction without bony foot procedures in 5 patients. Delayed consolidation and recurrent equinus contracture of the ankle requiring additional lengthening of the Achilles tendon were the most common bone and joint complications during tibial lengthening.
Interpretation The gradual foot frame distraction method was associated with major complications, such as recurrent foot deformity, joint luxation, and arthritis. We therefore recommend triple arthrodesis as a concomitant procedure during tibial lengthening
In patients with neuromuscular diseases, limb lengthening is associated with a high frequency of complications including joint contracture, delayed consolidation, and refracture because of neuromuscular imbalance, muscle atrophy, and osteoporosis (Aldegheri Citation1999). Leg shortening and complex foot deformity are common in patients with deformity after poliomyelitis. These conditions require leg lengthening and correction of the foot deformity to obtain a plantigrade foot. Some investigators have performed tibial lengthening as a separate operation, before or after correction of the foot deformity using traditional methods (Macnicol and Catto Citation1982, Huang Citation1997, Eralp et al. Citation2004). In these reports, patients experienced decreased walking speed due to weakness of the leg muscle, and equinus contracture of the ankle was the most common complication after tibial lengthening. The use of the Ilizarov method, with or without osteotomy of the tarsal bone, has been reported only for correction of foot deformity resulting from poliomyelitis (Paley Citation1993, Oganesyan et al. Citation1996, Kocaoglu et al. Citation2002, ucukkaya et al. Citation2002). Here we report the outcome of simultaneous tibial lengthening and foot deformity correction using the Ilizarov external fixator.
Patients and methods
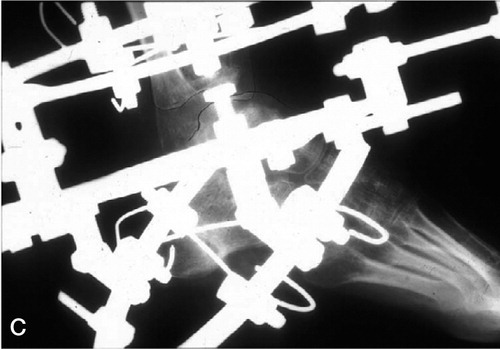
We reviewed 14 patients with permanent deformity after poliomyelitis. All patients had foot deformities and leg length discrepancy. The average patient age when the symptoms occurred and poliomyelitis was diagnosed was 9 (4-15) years, and age at operation was 33 (14-52) years The average leg length discrepancy was 3.7 (3-4.5) cm. Tibial lengthening over an intramedullary nail with Ilizarov fixator was performed in 3 patients, and without nail in 11 patients. In the proximal metaphysis, corticotomy was performed with multiple cortical drill holes and then the cortical bone was cut using an osteotome. In the no-nail group, 4 full rings were assembled with 2 proximal rings and 2 distal rings above and below the corticotomy site. Each ring was fixed by two Ilizarov wires or one wire and one half-pin. In the nail group, 3 rings were used, including 1 proximal ring and 2 distal rings (). The proximal ring and the most distal ring were fixed with two wires and one half-pin. The middle ring was not fixed to the bone by wires because it was difficult to maintain a space of more than 2 mm between the wire and the intramedullary nail due to the narrow medullary canal at the diaphysis. This space was necessary to avoid deep intramedullary infection resulting from wire/pin tract infection. We used an intramedullary nail with a diameter 2 mm less than that of the reamed medullary canal. Before surgery, we measured the diameter of the intramedullary cavity using plain radiography. Distraction was started 2 weeks after corticotomy at a rate of 0.75 mm/day (0.25 mm × 3).
Figure 1 A. Lengthening over intramedullary nail. B. Triple arthrodesis with 3 staples and Ilizarov foot frame extended from the lengthening frame. C. After removal of external fixator. D. After removal of external fixator.

All 14 feet had severe equinovarus deformity and 2 of the 14 feet had fiail ankle. The axial deformity of the tibia was defined by the CORA (center of rotation angulation) method with the malalignment test (Paley et al. Citation1994). Torsional deformity of the tibia was measured during physical examination in the sitting position with the knees in 90° fiexion by using a transmalleolar angle formed by the horizontal projections of the longitudinal axis of the thigh and the line perpendicular to the line connecting the medial malleolus and the lateral malleolus.
External fixation was removed when radiographs showed union (formation of 3 intact cortices at the distraction of the tibia) in the no-nail group. After removal of the external fixation, a long-leg cast or lower-leg bracing was applied for 4-6 weeks to prevent stress fracture. In the patients with nail, external fixation was removed after insertion of the interlocking screws and a long-leg cast was applied until union was achieved to avoid breakage of the interlocking screws, which would result in loss of length.
Union time at the lengthening site was evaluated using external fixation time (EFT) and healing index (HI). The HI was obtained by dividing the EFT by the amount of lengthening in the no-nail patients. In the nail patients, the HI was obtained by dividing the union time (between corticotomy and formation of 3 intact cortices) by the amount of lengthening. The results were divided into bone and function categories, according to a modification of the evaluation system previously reported by Paley (Citation1990).
Results
The average follow-up time was 5.5 (3-10) years. The mean amount of tibial lengthening was 3.7 (3.0-4.5) cm and the mean proportion of tibia lengthened was 12% (9-15%). The mean EFT was 6 (3.6-10) months in no-nail patients and 1.6 (1.5- 1.7) months in patients with nail. The mean HI was 1.8 (0.8-3.1) months/cm in no-nail patients and 2 (1.8-2.3) months/cm in nail patients.
Preoperatively, 6 of the 14 patients had an average varus deformity of 8.3° (3-12°) at the proximal tibia which was corrected with asymmetrical distraction during tibial lengthening. Axial rotational deformity of the tibia was corrected at the final stage of tibial lengthening with derotation of the Ilizarov frame distal to the corticotomy site. The amount of derotation was decided by the thigh-foot angle in prone position after correction of foot deformity. The average external torsion of the tibia was 41° (35-50°) before surgery and 21° (15-30°) after surgery. The foot deformities were simultaneously corrected with an extended foot frame connected to the leg-lengthening frame. Surgical procedures for foot deformity were triple arthrodesis in 7 patients, pantalar arthrodesis in 2, and gradual soft tissue distraction with external fixator in 5.
In the 7 patients who underwent triple arthrodesis, the varus deformity of the hindfoot was corrected with closing wedge osteotomy of the calcaneus, the talus, the cuboid, and the navicular. The severe equinus deformity was partially corrected to avoid resection of large amounts of bone. Closing wedge osteotomy was performed instead of opening wedge osteotomy with callotasis technique, because the unstable triple joints required rigid fixation to prevent resubluxation (which would result in recurrent deformity). The triple arthrodesis was performed to treat instability of the triple joints, even though the patients were young and had no osteoarthrotic change. Residual equinus deformity was gradually corrected by the extended foot frame distal to the tibial frame after tenotomy of soleus and gastrocnemius muscles at the musculotendinous junction (tendo achilles lengthening; TAL). The foot frame was composed of the calcaneal half-ring with two wires and one half-pin and the metatarsal half-ring with two wires. The triple joints were fixed with staples. At the removal of the Ilizarov fixator, the posterior tibial tendon was transferred to the dorsal aspect of the third cuneiform in 4 patients with triple arthrodesis who had absence of active foot dorsifiexion. The tendon transfer was performed during the removal of the external fixator because it was easier to perform at that time, in the absence of the wire/pins at the distal tibia, instead of at the end of distraction. Also, the general anesthesia induced for the tendon transfer permitted painless removal of the wires/pins.
In the 5 patients who underwent gradual soft tissue correction with external fixator, the equinovarus deformity was gradually corrected using the hinge system between the tibial and foot frames after TAL. The hinge was placed at the anteroinferior area to the center of the talar dome in the sagittal plane for translational effect, to prevent the anterior subluxation of the talus and to avoid compression of the anterior part of the talar dome. The talus was not fixed with wire or pin because pain might occur at the medial aspect of the hindfoot due to stretching of the soft tissue structure that is tethered by the wire.
Complications were classified as minor or major (Table). Minor complications required nonoperative treatment or a minor operative procedure. Major complications required a more complex operative procedure. There were 5 major and 14 minor bone complications in 12 patients. Complications included 5 cases of axial deviation, 3 pin-tract infections, 8 delayed consolidations of the tibia, 1 premature consolidation of the fibula, 1 malunion of the ankle, and 1 nonunion of the talonavicular joint. 2 of the 5 cases of axial deviation were deformations of the callus at the lengthening site of the proximal tibia after removal of the external fixator, and were treated using an above-knee cast after manipulation. Additional surgeries were pin removal, intramedullary nailing, reosteotomy of the fibula, supramalleolar osteotomy of the tibia, and bone grafting. Delayed consolidation of the tibia was defined as an HI of more than 1.7 months/cm or 50 days/cm (Aldegheri Citation1999). Of 8 patients with delayed consolidation, 2 patients with HI of more than 3 months/cm required treatments. Of the 2 patients with high HI, 1 52-year-old patient was treated with acute compression and insertion of an intramedullary nail. Ilizarov ring assembly was changed to monofixator after removal of wires and insertion of half-pins. The unreamed intramedullary nail was inserted while keeping the mono- fixator to maintain the length and correction of the deformity. Acute compression of 1.5 cm after insertion of proximal interlocking screws was done to treat delayed consolidation and then distal interlocking screws were inserted. Unfortunately, the patient had procurvatum deformity of 25° at the lengthening site after removal of the monofixator. Previously, she had had severe knee flexion contracture which was treated with the tibial Ilizarov frame and extended femoral frame. The interlocking nail could not resist rebounding tightness of knee fiexor muscles and led to procurvatum deformity. The second patient, aged 47 years, was treated with the compression-distraction method using the Ilizarov fixator. He had another complication, which was nonunion at the talonavicular joint after triple arthrodesis, and required bone grafting.
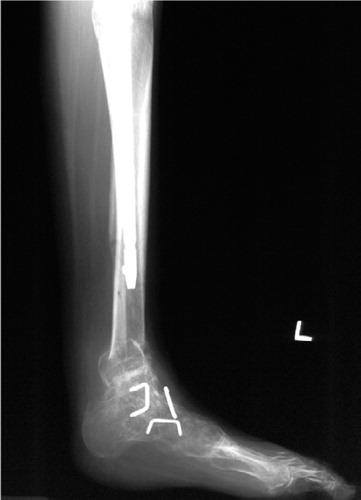
There were 7 major and 7 minor joint complications in 10 patients. Complications included 6 cases of equinus contracture of the foot, 4 knee fiexion contractures, 3 cases of anterior subluxation of the talus, 1 arthritic change of the ankle (), and 1 fiat top talus that led to stiff ankle with equinus deformity. Of the 6 cases of equinus contracture, 1 required supramalleolar osteotomy of the tibia (), and 1 required triple arthrodesis. Of the 4 cases of knee fiexion contracture, 2 were treated with gradual correction with extended Ilizarov frame above the knee with hinge system (which was located at the center of the rotation axis of the knee), and 2 required aggressive physiotherapy for knee extension, which started when the external fixation was removed. Anterior subluxation of the talus was treated with the translation system of the Ilizarov frame.
Figure 2 A case of severe equinocavovarus deformity and tibial shortening. A. Preoperative photograph. B. Preoperative radiograph. C. Radiograph showing anterior subluxation of the talus during correction of equinus deformity with the Ilizarov apparatus. D. Photograph after tibial lengthening and correction of the foot, showing plantigrade foot. E. Radiograph of the foot at 10-year follow-up, showing degenerative arthritis of the ankle and recurrent equinus deformity.

Discussion
The tibial lengthening has callus-related complica-tions, including axial deviation, delayed consolidation of the tibia, premature consolidation of the fibula, and refracture.
The incidence of delayed consolidation can be affected by the etiology of tibial shortening, the age of the patient, the osteotomy technique, and stability of the external fixation.
Delayed consolidation is common in poliomyelitis, infection, Turner syndrome, and metabolic bone diseases (Huang Citation1997, Aldegheri Citation1999). After poliomyelitis, the tibial lengthenings have longer healing periods compared to other diseases because of associated muscle atrophy and hypoplasia of the bone. Huang (Citation1997) reported that the mean HI was 2 (1-4.4) months/cm in 35 tibial lengthenings after poliomyelitis. Aldegheri (Citation1999) also reported a mean HI of 1.5 (1.3-1.8) months/cm after poliomyelitis and that 5 of 10 tibial lengthenings had delayed consolidations. We found that 8 of 14 tibial lengthenings with a mean HI of 1.8 (0.8- 3.1) months/cm had delayed consolidation. These results are compatible with the results of previous studies. Delayed consolidation requires a longer duration of external fixation, which is associated with a high incidence of pin-tract infection, loosening of the pin with concomitant loss of stability, and joint contracture. The bifocal lengthening osteotomy can be used to avoid delayed consolidation in poliomyelitis. Several authors have reported that this procedure reduces HI (Saleh and Jamer Citation1993, Fischgrund et al.1994, Staniski et al. Citation1996, Kristiansen and Steen Citation2002). Choi et al. Citation(1999) suggested this procedure for tibial lengthening beyond 20%, to decrease EFT and to distribute distraction force evenly throughout the entire muscle. They recommended that the distraction rate of the distal osteotomy site should be 75% of that at the proximal osteotomy site because of delayed consolidation at the distal osteotomy site. Eralp et al. (Citation2004) reported that the Gigli saw technique for tibial lengthening gave a shorter HI in 16 patients with deformity after poliomyelitis compared with percutaneous multiple drill hole osteotomy. Kristiansen and Steen (Citation2002) suggested the bifocal osteotomy for tibial lengthening of more than 6 cm to reduce HI. They found that equinus contracture of the ankle was a common complication in double-level lengthening, and recommended minimum lengthening for deformity correction at the distal tibia and prophylactic fixation of the foot with extended frame to prevent equinus contracture of the ankle. The ankle equinus occurred frequently during or after the tibial lengthening and the incidence depends on the distraction rate per day, the amount of lengthening, the age of the patient, the etiology of tibial shortening, and the technique of wire or pin insertion. Previous investigators have reported that the incidence of ankle equinus after tibial lengthening ranged from 10% to 50% according to the etiology of shortening (Yasui et al. Citation1997, Noonan et. Citation1998, Aldegheri Citation1999). Eldridge and Bell (Citation1991) and Lehman et al. (Citation1991) recommended prophylactic foot fixation with the foot frame during the lengthening phase and removal of the foot frame during the consolidation phase in patients with tibial lengthening beyond 10% of the original length or more than 6 cm, to avoid ankle equinus. Huang (Citation1997) reported that there were 11 cases of ankle equinus and 2 cases of knee fiexion contracture in 35 lengthenings of poliomyelitic tibiae. He recommended prophylactic TAL as a concomitant procedure during tibial lengthening.
Most poliomyelitic tibiae have foot deformities and require simultaneous correction of the tibial shortening and foot deformity. Poliomyelitic foot deformity requires bony procedures such as triple arthrodesis or V osteotomy, rather than soft tissue procedures, when the foot deformity is complex and rigid with incongruous tarsal joints due to long duration of subluxation. The incongruous tarsal joints cannot be congruous after reduction by soft tissue release or soft tissue distraction with an external fixator. Forceful reduction of the incongruous joints may produce pain and lead to recurrent foot deformity after removal of the external fixator. We found that using only the soft tissue distraction method for foot deformity was associated with more complications (including recurrent foot deformity, anterior subluxation of the talus, and arthritis of the ankle) than the triple arthrodesis during tibial lengthening. There is a tendency for anterior subluxation of the talus during correction of severe equinus deformity when the direction of the distraction force at the ankle is parallel to the long axis of the tibia in the sagittal plane. Therefore, posterior tilt of the distraction force along the posterior capsule of the ankle or tendo achilles is necessary to prevent anterior subluxation of the talus. The direction of the distraction force can be determined using the assembly of distraction rods with posterior inclination of 15° and using the universal hinge between Ilizarov frames for the tibia and foot. In our study, it was apparent in 3 patients with equinus deformity of more than 40° that the anterior part of the talar dome had been anteriorly subluxated for a long period and had resulted in a deformed talar dome with mild fiattening and joint incongruity before surgery. Even though the sub-luxated anterior part of the talar dome was reduced with the external fixator, there was resubluxation anteriorly in all 3 feet because of an abnormally remodeled joint with narrow ankle mortise during growth.
Thus, any attempt to reduce the deformed talar dome into the narrow ankle mortise to correct equinus deformity should be abandoned to avoid degenerative arthritis or resubluxation. In this situation, bony procedures, including V osteotomy, triple arthrodesis and pantalar arthrodesis, are recommended. Kucukkaya et al. (Citation2002) reported that 4 patients who had had poliomyelitis got plantigrade feet without recurrence after V osteotomy for correction of pes calcaneocavovarus and simultaneous lengthening at the distal tibia. 3 of the 4 patients had delayed consolidation at the distal tibial lengthening site after this method. In our study, 6 of 7 patients with triple arthrodesis had successful results and 1 patient required supramalleolar osteotomy for correction of recurrent foot deformity. The triple arthrodesis was performed using internal fixation with staples and the Ilizarov foot frame instead of using only the Ilizarov foot frame, because this combination method provided more stability and allowed earlier removal of the Ilizarov foot frame-with no need for additional wire insertion when there was wire-tract infection during follow-up.
During the tibial lengthening, knee fiexion contracture tended to occur instead of ankle equinus contracture because of immobilization of the ankle with the Ilizarov frame for foot deformity correction. Aggressive physiotherapy after removal of the external fixator usually solved knee fiexion contracture. However, residual tightness of the soleus-gas-trocnemius-achilles tendon complex may produce deformation of the callus during physiotherapy, and lead to procurvatum deformity. There were 4 cases of knee fiexion contracture in our study and 4 had procurvatum deformity at the proximal tibia among 14 cases. Thus, knee fiexion contracture should be managed carefully during tibial lengthening and after removal of the external fixator in order to avoid procurvatum deformity.
Previous investigators have recommended lengthening of the intramedullary nail to reduce complications associated with long EFT (Huang Citation1997, Paley et al. 1997, Simpson et al. Citation1999). The study of Huang (Citation1997) and our own study of patients after poliomyelitis have demonstrated that EFT with nail can be reduced to 28-30% of EFT without nail without affecting the healing period. The advantage of the nail method is that early removal of external fixation and cast application are possible because the foot deformity can be corrected quickly, or gradually within eight weeks. Therefore, the nail method is recommended in patients with poliomyelitis deformities to reduce EFT and associated complications such as pin-tract infection, axial deviation and refracture. However, serious complications of the nail method should be communicated to the patients, because previous studies (Paley et al. Citation1997, Kristiansen and Steen Citation1999, Simpson et al. Citation1999) have reported fatigue fractures of the intramedullary nail or interlocking screws and a deep intramedullary infection, resulting in delayed consolidation and shortening which required additional surgery.
- Aldegheri R. Distraction osteogenesis for lengthening of the tibia in patients who have limb length discrepancy or short stature. J Bone Joint Surg (Am) 1999; 81: 624–33
- Choi I H, Sohn C S, Chung C Y, Cho T, Lee J W, Lee D Y. Optimum ratio of distraction in double level tibial lengthening. Clin Orthop 1999; (368): 240–6
- Eldridge J, Bell D F. Problems with substantial limb lengthening. Orthop Clin North Am 1991; 4: 625–31
- Eralp L, Kocaoglu M, Ozkan K, Turker M. A comparison of two osteotomy techniques for tibial lengthening. Arch Orthop Trauma Surg 2004; 124(5)298–300
- Fischgrund J, Paley D, Suter C. Variables affecting time to bone healing during limb lengthening. Clin Orthop 1994; (301): 31–7
- Huang S C. Leg lengthening by the Ilizarov technique for patients with sequelae of poliomyelitis. J Formos Med Assoc 1997; 96: 258–65
- Kocaoglu M, Eralp L, Atalar A C, et al. Correction of complex foot deformities using the Ilizarov external fixator. J Foot Ankle Surg 2002; 41: 30–9
- Kristiansen L P, Steen H. Lengthening of the tibia over an intramedullary nail, using the Ilizarov external fixator. Major complications and slow consolidation in 9 lengthenings. Acta Orthop Scand 1999; 70: 271–4
- Kristiansen L P, Steen H. Reduced lengthening index by use of bifocal osteotomy in the tibia. Comparison of monofocal and bifocal procedures with the Ilizarov external fixator. Acta Orthop Scand 2002; 73: 93–7
- Kucukkaya M, Kabrkcuoglu Y, Kuzgun U. Management of the neuromuscular foot deformities with the Ilizarov method. Foot Ankle Int 2002; 23: 135–41
- Lehman W B, Grant A D, Atar D. Preventing and overcoming equinus contractures during lengthening of the tibia. Orthop Clin North Am 1991; 4: 633–41
- Macnicol M F, Catto A M. Twenty-year review of tibial lengthening for poliomyelitis. J Bone Joint Surg (Br) 1982; 64: 607–11
- Noonan K J, Leyes M, Forriol F, Canadell J. Distraction osteogenesis of the lower extremity with use of monolateral external fixation. J Bone Joint Surg (Am) 1998; 80: 793–806
- Oganesyan O V, Istomina I S, Kuzmin V I. Treatment of equinocavovarus in adults with the use of a hinged distraction apparatus. J Bone Joint Surg (Am) 1996; 78: 546–56
- Paley D. Problems, obstacles and complications of limb lengthening by the Ilizarov technique. Clin Orthop 1990; (250): 81–104
- Paley D. The correction of complex foot deformities using Ilizarov distraction osteotomies. Clin Orthop 1993; (293): 97–111
- Paley D, Herzenberg J E, Tetsworth K, McKie J, Bhave A. Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin North Am 1994; 25: 425–65
- Paley D, Herzenberg J E, Paremain G, Bhave A. Femoral lengthening over an intramedullary nail. A matched-case comparison with Ilizarov femoral lengthening. J Bone Joint Surg (Am) 1997; 79: 1464–80
- Saleh M, Jamer A J. Bifocal limb lengthening: A preliminary report. J Pediatr Orthop B 1993; 2: 42–8
- Simpson A H R W, Cole A S, Kenwright J. Leg lengthening over an intramedullary nail. J Bone Joint Surg (Br) 1999; 81: 1041–5
- Song H R, Oh C W, Mattoo R, Park B C, Kim S J, Park I H, Jeon I H, Ihn J C. Femoral lengthening over an intramedullary nail using the external fixator. Risk of infection and knee problems in 22 patients with a follow-up of 2 years or more. Acta Orthop 2005; 76: 245–52
- Stanitski D F, Shahcheraghi H, Nicker D A, Armstrong P F. Results of tibial lengthening with the Ilizarov technique. J Pediatr Orthop 1996; 2: 168–72
- Yasui N, Kawabata H, Kojimoto H, Ohno H, Matsuda S, Araki N, Shimomura Y, Ochi T. Lengthening of the lower limbs in patients with achondroplasia and hypochondroplasia. Clin Orthop 1997; (344): 298–306