Abstract
Background The incidence of acetabular loosening with segmental and cavitatory bone loss increases as the number of total hips implanted increases. Revisionhip arthroplasty using impacted bone graft and an acetabular reinforcement device is one solution to this problem.
Patients and methodsClinically and radiographically, we assessed 35 hips in 33 patients who had undergone revision hip arthroplasty using impaction grafting and the Kerboull acetabular reinforcement device. Mean follow-up was 5 (3–7) years.
Results The mean Mayo score preoperatively was 30, which improved to a mean score of 85. Good to excellent clinical results were seen in 25 patients. The 8 individuals scoring below 80 had significantly more comorbid conditions than the others. No acetabular reconstruction required re-revision. Aseptic loosening occurred in 6 patients. Graft resorption occurred in 5 cases, resulting in inferior hook fracture of the Kerboull device. This was noted at a mean of 13 months after surgery. Further follow-up showed this to be non-progressive, with incorporation of the remaining graft to the host bone. These patients all had good to excellent Mayo hip scores.
Interpretation Early results of revision acetabular surgery using impaction grafting and the Kerboull shell in patients with severe osteolysis have shown good functional outcome. However, 6 of 35 patients had radio-graphic evidence of aseptic loosening without progression for 4 years. Long-term follow-up is required to ensure that this loosening does not result in failure.
Acetabular loosening is the principal cause of failure of total hip arthroplasty (Schulte et al. Citation1993, Wroblewski and Siney Citation1993, Berry et al. Citation2002). Revision arthroplasty has been shown to improve an individual's quality of life (Robinson et al. Citation1999), but revision hip arthroplasty is often complicated by periacetabular osteolysis. The degree of bone loss ranges from minimal to catastrophic (D’Antonio et al. Citation1989, Paproski and Magnus Citation1994). Many techniques and devices have been devised to address this problem, with varying success. It has been our practice to restore bone stock and normalize the center of rotation of the hip using impaction bone grafting and the Kerboull acetabular reinforcement device (Howmedica, Ireland).
This device has an inferior hook which, when placed under the inferior margin of the acetabulum, centers the hip and prevents superior migration. The superior plate and two transverse arms recreate the shape of a normal acetabulum, allowing the location and the extent of bone loss to be clearly identified. The gaps between the arms allow protected loading of the impact allograft (Kerboull et al. Citation2000)
Clinically and radiographically, we evaluated the intermediate term results of patients who had undergone impaction bone grafting and acetabular reinforcement using the Kerboull shell for segmental and cavitatory acetabular bone loss.
Material and methods
Patients
We treated 35 patients with impaction allografting and acetabular reinforcement with the Kerboull shell in our institution between 1995 and 1999. 1 of these patients died due to unrelated causes and 1 was lost to follow-up, leaving 33 patients (21 women) of whom 2 had undergone bilateral procedures. There were thus 35 revision hip arthroplasties available for assessment. Surgery was carried out by consultant surgeons who were principally interested in arthroplasty (authors 3, 4 and 5). 34 hips were revised for aseptic loosening following cemented hip arthroplasty. 1 patient had a two-stage procedure because of infection.
The right hip was operated on in 18 patients and the left in 17 patients. The mean age at primary hip arthroplasty was 53 (35–74) years. The mean age at revision was 68 (48–89) years. The mean time to revision was 15 (2–25) years. 18 patients had bilateral primary hip arthroplasty prior to revision hip arthroplasty, and 4 had bilateral revision hip arthroplasty (of which 2 used the Kerboull shell and impaction grafting). All primary arthroplasties were cemented with metal on polyethylene bearing couples. 5 patients underwent revision of the acetabular component only. Information about any co-morbidities was collected. Patients were followed for a mean of 59 (40–87) months.
Surgery
Surgery was carried out in a laminar flow theatre. In all cases, specimens were sent for culture and sensitivity. Acetabular preparation followed removal of the loose implant. The soft tissue membrane was excised, exposing the deficient cavity. The allograft used was freezedried femoral heads harvested from primary hip arthroplasty patients. Graft morsellization was with a bone mill (New Splint, UK) producing croutons of 6 mm diameter. Of the 35 hips, 33 had morsellized bone from the mill and 2 had morsellized bone from large hand rongeurs. Structural allografts were not used. The bone was not intentionally fat-reduced. Grafted bone was loosely held in position using a reversed reamer and then impacted using hemispherical impactors. The appropriate-sized Kerboull shell for the defect was chosen and implanted, ensuring that the inferior hook was under the inferior acetabular margin. The number of screws placed in the horizontal plate varied from none in 12 shells, 1 in 6 shells, 2 in 14 shells, 3 in 2 shells and 4 in 1 shell. The cup was cemented directly onto the Kerboull shell and graft.
Assessment
All patients were reviewed at 6 weeks, 6 months, 1 year, and yearly thereafter. All patients were recalled to a special review clinic where they underwent clinical and radiographical evaluation by authors 1 and 2 who were not directly involved in the care of these individuals. Patients answered questions on the Mayo hip score (Kavanagh and Fitzgerald Citation1985). This score gives a maximum of 20 points for radiographic findings and 80 points for clinical and functional parameters. A score greater than 80 is considered good to excellent (excellent < 90). The operative notes were reviewed to ascertain the size of the bony defect after removal of the acetabular component. Radiographs were assessed by two observers (authors 1 and 2). Two lines were drawn: a horizontal inter-teardrop reference line and a perpendicular reference line through the tear drop. The average of the values from the two observers was used to measure vertical and horizontal distances to the center of the head before and after revision, and the amount of graft resorption as well as the acetabular index (Peters et al. Citation1995). Acetabular defects were classified according to the system devised by Gustilo and Pasternak (Citation1988).Type 1 defects have minimal osteolysis, type 2 have osteolysis leaving the anterior and pos-terior columns intact, type 3 represent severe oste-olysis with local segmental defects, and in type 4 there is massive and global collapse involving 2 or more acetabular walls. Radiolucent lines at the graftcement interface were classified according to DeLee and Charnley (Citation1976). Graft incorporation was based on the appearance of trabecular remodeling. Initial shell placement was assessed to ascertain whether the inferior hook was correctly placed. Metal failure such as screw breakage or fracture of the inferior hook was recorded.
Femoral components used at revision types were in 25 hips Charnley (De Puy); of which 4 were long-stem, Charnley elite in 5 hips, and the original femoral components were reused in 5 hips. Of the acetabular cups used, 33 were UHMWPE (DePuy)—of which 28 were 22 mm in diameter, 2 were 28 mm in diameter and 3 were 32 mm. 2 acetabular cups were of 28-mm hylamer.
Aseptic loosening was defined as screw breakage or loosening, or when there was any change in implant position as recorded by horizontal or vertical migration, an alteration in the acetabular index or a continuous radiolucent line < 2 mm.
Statistics
The data were analyzed using Fisher's exact test, t-tests for nonparametric data, and analysis of variance. The results were considered significant at p < 0.05. We used Graphpad statistical software version 3.0 throughout (GraphPad Software Inc., CA).
Results
Clinical findings
Preoperatively, the Mayo hip score was mean 31 (9-60), and at last follow-up it was mean 86 (68-98) (). 25 patients had good to excellent results, 7 patients received a fair rating and 1 patient scored poorly. 8 patients scored less than 80. This group had more co-morbid problems than those scoring 80 or more (p = 0.04). Associated problems in these 8 patients were spinal stenosis, chronic obstructive pulmonary disease in 2 patients, contralateral hip arthrodesis and contralateral aseptic loosening awaiting revision hip arthroplasty.
Table 1. Preoperative and postoperative Mayo hip scores correlated to Pasternak grade
Radiographic findings
Of the 35 acetabula available for follow-up, there were 4 type 2, 17 type 3 and 14 type 4 loosenings. No patient had pelvic discontinuity. All patients had correct placement of the hook under the inferior margin of the acetabulum. The mean postoperative abduction angle of the Kerboull shell was 42° (26–68).
There were 6 cases of aseptic loosening (). 5 patients had fractures of the inferior hook allowing superomedial displacement and a decrease in the abduction angle of the device. In these patients, the mean medial migration was 5 (2–13) mm and superior migration was 3 (1–6) mm. The mean abduction angle of the Kerboull shell immediately after surgery in these patients was 47° (31–68). Following graft resorption and hook fracture, this decreased to a mean of 40° (28–66). The mean time to fracture of the hook was 13 (6–18) months. The mean number of screws in the horizontal plate in these patients was 2 (1–2).
Table 2. Acetabular aseptic loosening
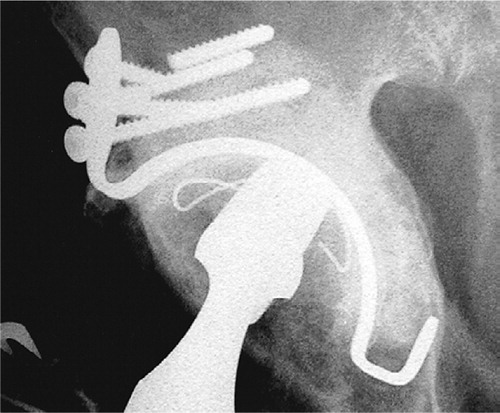
2 patients had broken screws in the horizontal plate. 1 of these had an inferior hook fracture and graft resorption. The other patient had 1 of 4 screws broken in the horizontal plate (). This occurred 12 months after surgery, and no further radiographic changes had occurred 37 months after surgery.
Figure 1. Broken screw in superior plate seen 37 months after surgery. The screw was known to be broken 12 months postoperatively.
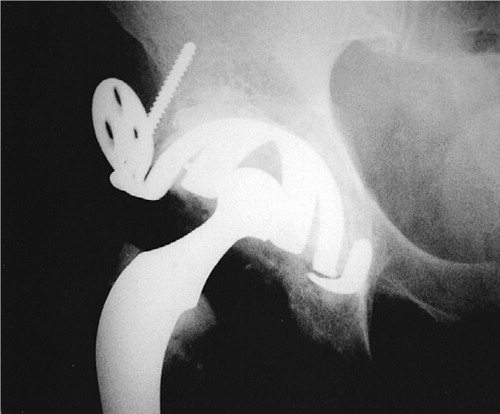
Graft resorption lateral to the vertical line occurred in 5 hips. These hips were the same as those that sustained hook fractures Graft resorption medial to this line was seen in 2 hips. However, this resorption was confined to the intrapelvic portion of the graft only, and was felt to represent graft remodeling. In the patients with hook fractures the graft resorption became apparent when the hook fractured, allowing the shell to migrate (). These patients were followed for a mean of 43 (22–59) months following hook fracture. No further migration or graft resorption was detected during this period; nor was any lucency detected at the cement bone interface. No patient had a complete radiolucent line at the bone-cement interface.
Figure 2 B. The same patient taken 4 years after revision surgery. The inferior hook fracture had been present for 3 years.
3 patients sustained dislocations. 2 patients had only one episode of dislocation and had no further recurrence, 1 of these patients did undergo graft resorption and hook fracture but this had not occurred at the time of her dislocation. 1 patient developed recurrent dislocation and required posterior augmentation of the acetabular component with a successful outcome (the acetabulum was well fixed with good incorporation of bone graft). 1 patient had a trochanteric nonunion requiring surgical reattachment, and 1 patient sustained a periprosthetic fracture of the femur and required further surgery to the femur alone.
2 patients had radiolucent lines 1–2 mm in DeLee zone 1. These were non-progressive and not associated with decreased Mayo scores. No association was seen with regard to follow-up Mayo hip scores and graft resorption. Mayo scores for these patients were not different to those for the remaining cohort (mean 88 (81–96), p = 0.4). The remaining bone graft in these patients appeared to be incorporated. Nor was there any association between the follow-up Mayo scores and sex (p = 0.3), the age at primary surgery (p = 0.3), the interval to revision (p = 0.4), the age at revision (p = 0.1), Pasternak score (p = 0.3), the operating surgeon (p = 0.4), the number of screws used in the horizontal plate (p = 0.2), or whether morsellization of bone was carried out using a bone mill or a rongeur (p = 0.4).
The 2 acetabular cups that were 28-mm hylamer showed no loosening. Of the 6 hips with radio-graphic evidence of aseptic loosening, 5 were 22-mm inner diameter cups and 1 was 28 mm in diameter. No association was seen between cup size and Mayo score (p = 0.3). There were 14 acetabula with segmental medial wall defects. There was no difference in the follow-up Mayo score compared to those patients with an intact medial wall (p = 1); nor was there any difference when patients with aseptic loosening were compared to those with no component migration with regard to the presence or absence of a medial wall defect (p = 0.7).
Discussion
Revision hip arthroplasty in the presence of substantial acetabular osteolysis presents a technically challenging problem. Anti-protrusio devices are designed to bridge bone loss, protect the underlying reconstruction, restore the normal hip center and give support to the acetabular component (Oh and Harris Citation1982, Berry and Muller Citation1992, Rosson and Schatzker Citation1992, Gill et al. Citation1998, Eggli et al. Citation2002). Many such devices exist, differing in their fixation. The Muller ring (Protek, Switzerland) attaches to the ileum only, whilst the Burch-Sch-neider anti-protrusio cage (Protek, Switzerland) has both ischial and ileum fixation.
Long-term success has been obtained with morsellized allograft (Sloof et al. Citation1996, Avci et al. Citation1998, Scheurs et al. 1998, Bohm and Banzhaf Citation1999, Winter et al. Citation2001). Histological studies in animals have shown that graft incorporation is preceded by a vascularization front with subsequent graft resorption, woven bone deposition and bone remodeling (Goldberg and Stevenson Citation1987, Schimmel et al. Citation1998). These findings have been confirmed in humans by study of biopsy and retrieval specimens (Heekin et al. Citation1995, Buma et al. Citation1996). Positron emission tomography has also shown in vivo human graft viability (Piert et al. Citation1999). Success as evidenced by implant survival after using a morsellized graft has been reported to be 90% at 7 years by Garbuz et al. (Citation1996), while Schreurs et al. (Citation1998) had a 96% success rate at 12 years.
Massive structural allografts, when used in reconstruction of the acetabulum, may function initially but have been associated with cup loosening in the long term. The rate of acetabular implant loosening is related to the coverage by the allograft (Shinar and Harris Citation1997, Hooten et al. Citation1994). Early loosening with structural allograft has also been seen in uncemented cups (Hooten et al. Citation1994).
Kerboull et al. (Citation2000) published results involving 60 cases, using the shell devised by this group. The technique involved use of an allograft superiorly for load bearing, together with morsellized grafts. In 3 cases, the graft was resorbed and the acetabular component migrated. Inferior hook breakage occurred in 3 patients, of which only 1 had any graft resorption. No patient had dislocation and implant survival at 13 years was 92%.
Previously published series using acetabular augmentation devices have suggested that incomplete spanning of defects with acetabular roof rings leads to a lower success rate in acetabula with medial segmental bone loss as compared to an anti-protrusio cage (Rosson and Schatzker Citation1992, Schatzker and Wong Citation1999). The Kerboull shell was devised to span defects taking support from both the ischium and the ileum. This may fail in cases of pelvic discontinuity, of which we had none in our series. Gill et al. (Citation1998) had 3 rerevisions after an average of 9 years, due to aseptic loosening in their cohort of 66 patients using the Burch-Schneider cage. Schatzker and Wong (Citation1999) had 2 cases of re-revision for aseptic loosening in 38 patients using the Burch-Schneider cage, with a mean follow-up of 7 years. Van der Linde and Tonino (Citation2001) had 5 cases of medial migration of 42 revised cups with grafting and an acetabular ring. This loosening did not progress after 2 years, except in 1 case which required re-revision. Their median follow-up time was 10 years. None of the 35 hips in our series required revision after a mean of 6 years. Importantly, however, 6 acetabula had signs of loosening. Component fracture and migration occurred at a mean of 13 months in x hips. After 22–59 months, no evidence of progression or lucent line formation was seen and despite initial graft resorption, good remodeling and incorporation occurred between the remaining graft and host bone ().
Figure 3. 6 years after revision surgery. Broken inferior hook, but with good residual graft incorporation.

Failure of the inferior hook and screw breakage occurred with loosening in 6 patients. Graft resorption may have been secondary to stress shielding by the Kerboull shell. This, however, is reduced by the open configuration created by the four arms allowing at least partial graft loading. Failure to impact the graft adequately may also lead to graft resorption, and we believe that optimal impaction grafting technique and the use of partially defatted graft could further reduce the frequency of graft resorption.
We continue to use allograft in association with the Kerboull shell. Our clinical outcome is good, with 100% acetabular survival at a mean of 6 years. We have seen no evidence of progressive radio-lucent lines, but long-term review is required to ensure that this loosening does not result in failure later on.
No competing interests declared.
- Avci S, Connors N, Petty W. 2- to 10-year follow-up study of acetabular revisions using allograft bone to repair bone defects. J Arthroplasty 1998; 13(1)61–9
- Berry D J, Muller M E. Revision arthroplasty using an anti-protrusio cage for massive acetabular bone deficiency. J Bone Joint Surg (Br) 1992; 74(5)711–5
- Berry D J, Harmsen W S, Cabanela M E, Morrey B F. Twenty-five-year survivorship of two thousand consecutive primary Charnley total hip replacements: factors affecting survivorship of acetabular and femoral components. J Bone Joint Surg (Am) 2002; 84(2)171–7
- Bohm P, Banzhaf S. Acetabular revision with allograft bone. 103 revisions with 3 reconstruction alternatives, followed for 0.3–13 years. Acta Orthop Scand 1999; 70(3)240–9
- Buma P, Lamerigts N, Schreurs B W, Gardeniers J, Versleyen D, Slooff T J. Impacted graft incorporation after cemented acetabular revision. Histological evaluation in 8 patients. Acta Orthop Scand 1996; 67(6)536–40
- D'Antonio J A, Capello W N, Borden L S, Bargar W L, Bierbaum B F, Boettcher W G, Steinberg M E, Stulberg S D, Wedge J H. Classification and management of acetabular abnormalities in total hip arthroplasty. Clin Orthop 1989, 243: 126–37
- DeLee J G, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop 1976, 121: 32–20
- Eggli S, Muller C, Ganz R. Revision surgery in pelvic discontinuity: an analysis of seven patients. Clin Orthop 2002, 398: 136–45
- Garbuz D, Morsi E, Mohamed N, Gross A E. Classification and reconstruction in revision acetabular arthroplasty with bone stock deficiency. Clin Orthop 1996, 324: 98–107
- Gill T J, Sledge J B, Muller M E. The Burch-Schneider anti-protrusio cage in revision total hip arthroplasty: indications, principles and long-term results. J Bone Joint Surg (Br) 1998; 80(6)946–53
- Goldberg V M, Stevenson S. Natural history of autografts and allografts. Clin Orthop 1987, 225: 7–16
- Gustilo R B, Pasternak H S. Revision total hip arthroplasty with titanium ingrowth prosthesis and bone grafting for failed cemented femoral component loosening. Clin Orthop 1988, 235: 111–9
- Heekin R D, Engh C A, Vinh T. Morselized allograft in ace-tabular reconstruction. A postmortem retrieval analysis. Clin Orthop 1995, 319: 184–90
- Hooten J P, Jr, Engh C A, Jr, Engh C A. Failure of structural acetabular allografts in cementless revision hip arthroplasty. J Bone Joint Surg (Br) 1994; 76(3)419–22
- Kavanagh B F, Fitzgerald R H, Jr. Clinical and roentgeno-graphic assessment of total hip arthroplasty. A new hip score. Clin Orthop 1985, 193: 133–40
- Kerboull M, Hamadouche M, Kerboull L. The Kerboull ace-tabular reinforcement device in major acetabular reconstructions. Clin Orthop 2000, 378: 155–68
- Oh I, Harris W H. Design concepts, indications, and surgical technique for use of the protrusio shell. Clin Orthop 1982, 162: 175–84
- Paprosky W G, Magnus R E. Principles of bone grafting in revision total hip arthroplasty. Acetabular technique. Clin Orthop 1994, 298: 147–55
- Peters C L, Curtain M, Samuelson K M. Acetabular revision with the Burch-Schnieder antiprotrusio cage and cancellous allograft bone. J Arthroplasty 1995; 10(3)307–12
- Piert M, Winter E, Becker G A, Bilger K, Machulla H, Muller-Schauenburg W, Bares R, Becker H D. Allogenic bone graft viability after hip revision arthroplasty assessed by dynamic 18F fluoride ion positron emission tomography. Eur J Nucl Med 1999; 26(6)615–24
- Robinson A H, Palmer C R, Villar R N. Is revision as good as primary hip replacement? A comparison of quality of life. J Bone Joint Surg (Br) 1999; 81(1)42–520
- Rosson J, Schatzker J. The use of reinforcement rings to reconstruct deficient acetabula. J Bone Joint Surg (Br) 1992; 74(5)716–20
- Schatzker J, Wong M K. Acetabular revision. The role of rings and cages. Clin Orthop 1999, 369: 187–97
- Schimmel J W, Buma P, Versleyen D, Huiskes R, Slooff T J. Acetabular reconstruction with impacted morselized cancellous allografts in cemented hip arthroplasty: a histological and biomechanical study on the goat. J Arthroplasty 1998; 13(4)438–48
- Schreurs B W, Slooff T J, Buma P, Gardeniers J W, Huis-kes R. Acetabular reconstruction with impacted morsellised cancellous bone graft and cement. A 10- to 15-year follow-up of 60 revision arthroplasties. J Bone Joint Surg (Br) 1998; 80(3)391–5
- Schulte K R, Callaghan J J, Kelley S S, Johnston R C. The outcome of Charnley total hip arthroplasty with cement after a minimum twenty-year follow-up. The results of one surgeon. J Bone Joint Surg (Am) 1993; 75(7)961–75
- Shinar A A, Harris W H. Bulk structural autogenous grafts and allografts for reconstruction of the acetabulum in total hip arthroplasty. Sixteen-year-average follow-up. J Bone Joint Surg (Am) 1997; 79(2)159–68
- Slooff T J, Buma P, Schreurs B W, Schimmel J W, Huiskes R, Gardeniers J. Acetabular and femoral reconstruction with impacted graft and cement. Clin Orthop 1996, 324: 108–15
- van der Linde M, Tonino A. Acetabular revision with impacted grafting and a reinforcement ring: 42 patients followed for a mean of 10 years. Acta Orthop Scand 2001; 72(3)221–7
- Winter E, Piert M, Volkmann R, Maurer F, Eingartner C, Weise K, Weller S. Allogeneic cancellous bone graft and a Burch-Schneider ring for acetabular reconstruction in revision hip arthroplasty. J Bone Joint Surg (Am) 2001; 83(6)862–7
- Wroblewski B M, Siney P D. Charnley low-friction arthro-plasty of the hip. Long-term results. Clin Orthop 1993, 292: 191–201
