Abstract
Introduction We used an experimental hip model to assess the mechanical stability of a hip prosthesis, and compared the femoral medullary canal preparation techniques of reaming and broaching.
Methods 15 pairs of cadaveric femora had a simulated replacement, the right femur with a reaming technique and the left with a broaching technique. Both femurs were radiographed to assess component positioning and cement mantle. The femurs were osteotomized 30 days after the procedure. The shear strength of the interface was studied at 4 different levels along an aluminum rod during push-out tests.
Results The overall mean value of the interface failure load was 15% lower with the reaming technique (6.5 kN for the reaming technique versus 7.7 kN for the broaching technique; p = 0.02).
Interpretation Broaching was superior to reaming for the preparation of the femoral canal, and should be used in order to increase primary stability. Further in vivo studies are required to account for factors such as intramedullary pressure, bleeding and surgical variations, which could not be accounted for in our study.
Many aspects of cemented fixation of arthroplasties have been investigated, such as variations in the cement itself, different modes of application, and implant design (Morita et al. Citation1999, Barrack Citation2000, Breusch et al. Citation2000b, Ramaniraka et al. Citation2000, Shepard et al. Citation2000, Peters et al. Citation2001, Espehaug et al. Citation2002, Glyn-Jones et al. Citation2003). One of the least researched areas is the mode of preparation of the medullary canal to receive the cement-implant composite (DiGiovanni et al. Citation1999, Breusch et al. Citation2000a, Citation2001). Most surgeons are prepared to accept the suggestions of the manufacturers, which are usually very similar to each other. Reaming to the level of templating is proposed for an uncemented implant, and then cementing of one that is usually at least 2 mm narrower all round, to allow room for an adequate cement mantle. The older technique of broaching has been accused of leaving behind a lot of weak cancellous bone that may compromise fixation (Johanson et al. Citation1987). On the other hand, the latter could also be true of mechanical reaming which leaves an almost polished endocortex surface with poor interdigitation of the cement, leading to a weak bone-cement interface. This controversy has not been resolved, and to our knowledge there has been no report published in which these two techniques are compared.
We designed an experimental model in cadaveric femora in order to compare the push-out strength of the cement-bone interface when these two different techniques are used.
Material and methods
15 pairs of cadaveric femora were used. They were radiographed (anterior-posterior and lateral projections) before any intervention, and subsequently templated using the Multilock (Zimmer,Warsaw, Indiana, USA) templates to select the appropriate size of implant.
All femurs were osteotomized at the calcar 1 cm above the lesser trochanter. On right femora, reaming to the templated size was by use of straight reamers. On the left side, size broaches were used to obtain the templated size. All instruments used belonged to the Zimmer Multilock Hip System.
CMW-1 radiopaque bone cement was applied without the use of high-pressure lavage. Second-generation cement technique was used (intramedullary plug and cement gun, with conventional open-bowl mixing technique). After introduction of the “stem” and during curing, pressure was applied to the upper surface of the cement by hand, using a femoral cement compressor (Smith and Nephew, Memphis, Tennessee, USA).
Aluminum rods of 15 cm length with a circular cross section were used to simulate the stem. According to the manufacturer's guidelines, the diameter of the rod was 2 mm less that the reamed/broached size, thus the diameter of the rods used ranged from 8 to 14 mm, with 2 mm increments.
Radiographic evaluation was repeated after implantation in order to evaluate the results of the cementing technique and to recognize any severe discrepancies that may have biased the results. We used a lower limit of at least a 2-mm thick cement mantle all around the rods (Ebramzadeh et al. Citation1994, Joshi et al. Citation1998). A large air “bubble” was found in one of the specimens, so this pair of bones was excluded from the study. Another pair was excluded due to varus malpositioning of the femoral stem that ended abutting the lateral cortex, thus leaving practically no PMMA in the area. Following preparation of the specimens, we kept them in a dark room with a steady room temperature of 21°C for 30 days, to allow complete cement polymerization.
The specimens were then sectioned into 6 pieces, using a precision water-cooled rotating diamond disk cutting device (Discotom). The first was at a level of 1.5 cm below the level of the calcar osteotomy. The other four were 3 cm thick each, and the last was the remaining bone. The upper 1.5-cm slice was excluded from testing in order to avoid any irregularities due to the cement pressurization during curing. For the same reason, the last piece was also not tested since it contained a very small part of the aluminum rod, the cement restrictor and one piece of cement that filled the entire lumen. The three regions tested corresponded to Gruen regions 1 and 7, 2 and 6, and 3 and 5, and the last corresponded to zone 4 (Gruen et al. Citation1979). Finally, we were left with 52 specimens to be tested per technique ().
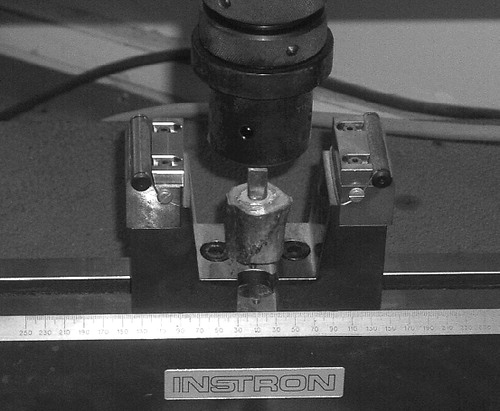
The constructs were subjected to push-out mechanical loading with an Istron 4482 testing machine, to evaluate the strength of the bone-cement interface. In order to do this, the pusher of the cervomachine was slightly larger than the cross section of the aluminum rod, so the force would be applied to the cement-rod complex (). As the failure point, we took the moment that the stresses at the surface being tested stopped rising, followed by an abrupt decrease in their value. This point was defined by observing the peak of the load in the load/displacement graph in the computer connected to the cervomachine, and this was verified by reading the value calculated by the computer.
Figure 2. The constructs were subjected to push-out mechanical loading with an Instron 4482 testing machine. Note that the pusher of the Instron machine was slightly wider than the cross section of the aluminum rod.
The value for each specimen was compared with the corresponding value for its partner specimen treated by the other technique (reaming or broaching) ().
Statistics
We used two-way ANOVA and the Bonferonni multiple comparison test, with technique (reaming and broaching) and sections (1, 2, 3 and 4) serving as discriminating variables (a = 0.05) SigmaStat software was used (Jandel Scientific, San Rafael, CA).
Results
The overall mean value of the interfaced failure load was 15% lower with the reaming technique than with broaching technique. There was also a difference in the mean values (p = 0.02) among the different techniques. There was no difference in the mean values among the different section levels (p = 0.9). There was no relation between technique and section (p = 0.9) ( and ).
Table 1. Mean failure values in push-out tests, expressed in kN, for each group of specimens according to the technique and the section
Table 2. Failure values, expressed in kN, for all 104 specimens
Discussion
There have been many studies reporting excellent clinical results using the broaching technique (McCoy et al. Citation1988, Kavanagh et al. Citation1994, Madey et al. Citation1997). Use of reaming and broaching together may also be effective (Harris Citation1997). Weber (Citation1988) reported a 92% success rate with this technique after 7–11 years of follow-up. Kavanagh et al. (Citation1994) reported very good results in a 20-year follow-up study from Mayo Clinic using a broaching-only system, as did Madey et al. (Citation1997).
Contrary to the early recommendations of Charnley (Citation1960), who suggested removal of all the cancellous bone, some authors prefer the reaming technique. In a radiographic study by Ebramzadeh et al. (Citation1994) of more than 800 hips followed for 21 years, considering multiple variables such as stem orientation, cancellous bone thickness and thickness of the cement mantle, implant survival was positively correlated to the presence of less than 2 mm of proximal-medial cancellous bone mantle.
The authors found worse results when more cancellous bone was left behind in the preparation of the femoral canal. However, there were some weaknesses in this study, since many of the hips were lost to follow-up and there were many confounders.
The view of some authors that remaining cancellous bone in the canal may jeopardize the results has been questioned. In a laboratory study, Breusch et al. (Citation1997) disproved the notion that trabeculae embedded in cement atrophy with fibrous substitution. These authors proved histologically that cement in small (< 1 mm2) cancellous honeycombs does not cause trabecular necrosis due to increased temperature. They observed that trabeculae subsequently shrink, leaving behind an area that is capable of rapid revascularization and bone remodeling. Bugbee et al. (Citation1992) reported that aggressive reaming could lead to failure of the cement fixation, and Bean et al. (Citation1987) came to the same conclusion. DiGiovanni et al. (Citation1999) stated that the excess bone resulting from broaching does not seem to compromise fixation at the bone-cement interface.
Newman et al. Citation(1993) demonstrated a 22% higher peak failure load in broached specimens, compared to ones with distal reaming followed by proximal broaching. In a similar experiment, Balu et al. (Citation1994) compared the outcome of reaming and no reaming, in fully-reversed tension and compression testing at a frequency of 0.5 Hz until failure occurred. They found 23% greater loss of rough endosteal surface on average after reaming with flexible reamers and increasing the canal diameter by only 1 mm. Another important finding was the decrease in shear strength at the bone-cement interface using flexible reamers as compared to no reaming as controls. These authors did not recommend reaming for preparation of the femoral canal for cemented fixation (Balu et al. Citation1994).
Our study shows that the use of the broaching technique was superior to the reaming technique in cadaveric femora and in a static model construction. Further studies are required to consider factors such as intramedullarly pressure and bleeding and surgical and implant variations, which were not accounted for in our study.
- Balu G R, Noble P C, Alexander J W, Vela V L. The effect of intramedullary reaming on the strength of the cement/bone interface. Trans Orthop Res Soc 1994; 19: 797
- Barrack R L. Early failure of modern cemented stems. J Arthroplasty 2000; 15(8)1036–50
- Bean D J, Convery F R, Woo S L Y, Lieber R L. Regional variations in shear strength of the bone -poly methyl methacrylate interface. J Arthroplasty 1987; 2: 293–8
- Breusch S J, Draenert K. Vacuum application of bone cement in total hip arthroplasty. Hip Int 1997; 7: 137–52
- Breusch S J, Lehner B, Schneider Caillouette U, Wenz W, Kreutzer J, Ewerbeck V, Lukoschek M. Effect of a rasp surface on cement penetration in paired cadaver femurs. Z Orthop Ihre Grenzgeb 2000a; 138(1)60–5
- Breusch S J, Norman T L, Schneider U, Reitzel T, Blaha J D, Lukoschec M. Lavage technique in total hip arthroplasty: jet lavage produces better cement penetration than syringe lavage in the proximal femur. J Arthroplasty 2000b; 15(7)921–7
- Breusch S J, Norman T, Revie I C, Lehner B, Caillouette J T, Schneider U, Blaha J D, Lukoschek M. Cement penetration in the proximal femur does not depend on broach surface finish. Acta Orthop Scand 2001; 72: 29–35
- Bugbee W D, Barrera D L, Lee A C, Convery F R. Variations in shear strength of the bone-cement interface in the proximal femur. Trans Orthop Res Soc 1992; 17: 22
- Charnley J. Anchorage of the femoral head prosthesis to the shaft of the femur. J Bone Joint Surg (Br) 1960; 42: 28–30
- DiGiovanni C W, Garvin K L, Pellicci P M. Femoral preparation in cemented total hip arthroplasty: reaming or broaching. J Am Acad Orthop Surg 1999; 7(6)349–57
- Ebramzadeh E, Sarmiento A, Mc-Kellop H A, Llinas A, Gogan W. The cement mantle in total hip arthroplasty: Analysis of many long term radiographic results. J Bone Joint Surg (Am) 1994; 76: 77–87
- Espehaug B, Fumes O, Havelin L I, Engesaeter L B, Vollset S E. The type of cement and failure of total hip replacements. J Bone Joint Surg (Br) 2002; 84(6)832–8
- Glyn-Jones S, Hicks J, Alfaro-Adrian J, Gill H S, McLardy-Smith P, Murray D W. The influence of cement viscosity on the early migration of a tapered polished femoral stem. Int Orthop 2003; 27(6)362–5
- Gruen T A, McNeice G M, Amstutz H C. “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop 1979, 141: 17–27
- Harris W H. Options for primary femoral fixation in total hip arthroplasty: Cemented stems for all. Clin Orthop 1997, 344: 118–23
- Johanson N A, Bullough P G, Wilson P D, Jr, Salvati E A, Ranawat C S. The microscopic anatomy of the bone-cement interface in failed total hip arthroplasties. Clin Orthop 1987, 218: 123–35
- Joshi R P, Eftekhar N S, McMahon D J, Nercessian O A. Osteolysis after Charnley primary low-friction arthroplasty. A comparison of two matched paired groups. J Bone Joint Surg (Br) 1998; 80(4)585–90
- Kavanagh BF, Wallrichs S, Dewitz M, Berry D, Currier B, Ilstrup D, Coventry MB. Charnley low friction arthroplasty of the hip: Twenty year results with cement. J Arthroplasty 1994; 9: 229–34
- Madey S M, Callaghan J J, Olejniezac J P, Goetz D D, Johnston R C. Charnley total hip arthroplasty with use of improved techniques of cementing: The results after a minimum of fifteen years follow up. J Bone Joint Surg (Am) 1997; 79: 53–64
- McCoy T H, Salvati E A, Ranawat C S, Wilson P D, Jr. A fifteen-year follow up study of one hundred Charnley low-friction arthtroplasties. Orthop Clin North Am 1988; 19: 467–76
- Morita S, Kawachi S, Yamamoto H, Shinomiya K, Nakabayashi N, Ishihara K. Total hip arthroplasty using bone cement containing tri-n-butylborane as the initiator. J Biomed Mater Res 1999; 48(5)759–63
- Newman M A, Bargar W L, Hayes D E, Jr, Taylor J K. Femoral canal preparation for cemented stems ;Reaming versus broaches. Presented at the 60th Annual Meeting of the American Academy of Orthopaedics Surgeons, San Francisco, February, 181993
- Peters C L, Bachus K N, Craig M A, Higginbotham T O. The effect of femoral prosthesis design on cement strain in cemented total hip arhroplasty. J Arthroplasty 2001; 16(2)16–24
- Ramaniraka N A, Rakotomanana L R, Leyvraz P F. The fixation of the cemented femoral component. Effects of stem stiffness, cement thickness and roughness of the cement-bone surface. J Bone Joint Surg (Br) 2000; 82(2)297–303
- Shepard M F, Kabo J M, Lieberman J R. The Frank Stinchfield Award. Influence of cement technique on the interface strength of femoral components. Clin Orthop 2000, 381: 26–35
- Weber B G. Pressurized cement fixation in total hip arthroplasty. Clin Orthop 1988, 232: 87–95

