Abstract
Background On theoretical grounds mobile bearing total knees should reduce the micromotion of the tibial component relative to the bone.
Patients and methods We used radiostereometric analysis to measure the three-dimensional micromotion in 42 tibial components during 2 years of follow-up. The patients had been randomized as to whether they would receive a mobile bearing (MB) or posterior stabilized (PS) design. We expected that the MB knee would facilitate dissipation of forces from the prosthesis-bone interface by the motion of the bearing and by load sharing with the soft tissues, leading to less micromotion. In the PS designs, limited free rotation caused by the campost articulation might cause additional stress at the bone-prosthesis interface.
Results We found no significant differences between the MB and PS group at the 2-year follow-up evaluation with respect to Knee Society scores and radiographic results. The PS group had a higher variability in subsidence and anterior-posterior tilting of the component than the MB group.
Interpretation The low variability of the data in the MB knee prosthesis group suggests that this design is more predictable and forgiving with respect to micromotion of the tibial component.
Wear is one of the critical factors limiting the long-term success of total knee prostheses (TKP). Retrieval studies of tibial inserts have shown that low conformity and the thickness of the polyethylene insert are associated with increased wear (Bartel et al. Citation1986, Collier et al. Citation1991, Wright et al. Citation1992). One design option which deals with this problem is the mobile bearing (MB) insert, which combines high conformity with maximized range of motion (Buechel and Pappas Citation1990, Jordan et al. Citation1997). In contrast to this mobile design, the fixed-bearing posterior stabilized (PS) TKP, which has a high degree of internal constraint and which has been used most frequently during some periods (Stern and Insall Citation1992, Aglietti et al. Citation1999, Li et al. Citation1999).
The better wear characteristics of the MB prostheses are based on the relatively large contact area of these designs, thus the contact stresses in the polyethylene are lower compared to the PS designs. Furthermore, if the femoral component and tibial components are malaligned and slight orientation differences are present between the components, the fixed-bearing PS insert will be forced in a certain direction during the range of motion. On the other hand, differences between component rotation and the actual knee joint will be corrected by a movable bearing. PS implants show more polyethylene wear debris (Puloski et al. Citation2001), while the MB designs result in less wear of the polyethylene (Jones et al. Citation1999).
Torque and shear forces in a MB TKP will be better dissipated from the prosthesis-bone interface by the motion of the bearing and by load sharing with the ligaments and other soft tissue structures (Buechel and Pappas Citation1990, Goodfellow and O’Connor Citation1992, Callaghan et al. Citation2001). In the PS design, the limited free rotation caused by the campost articulation may cause additional stress at the bone-prosthesis interface.
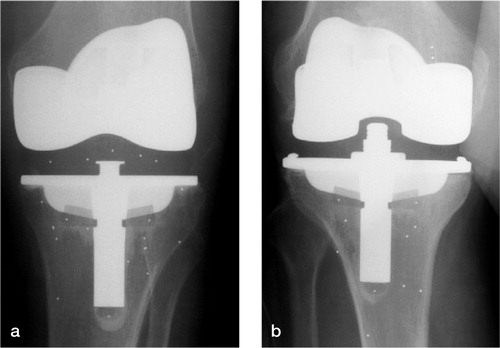
Figure. Antero-posterior radiograph of an MB (a) and a PS (b) total knee prosthesis as used in this study.
Early micromotion of implants has been shown to be related to implant survival (Grewal et al. Citation1992). This micromotion can be assessed very accurately using radiostereometric analysis (RSA). Besides the high degree of accuracy, the value of RSA is its predictive value for future prosthesis loosening (Selvik Citation1989, Kärrholm et al. Citation1994, Ryd et al. Citation1995). The purpose of our study was to examine the amount of three-dimensional micromotion of the tibial component in a randomized RSA study, comparing a fixed-bearing PS TKP with an MB design.
Patients and methods
42 consecutive primary cemented TKPs (33 patients; 21 women) were included. During surgery, a randomization scheme selected the patients for either a PS prosthesis or an MB prosthesis. If a patient was operated bilaterally, the randomization scheme was also followed starting with the right leg. In each group, 2 patients received the same implant design in both knees. Patients with a deformity of more then 20° in any plane were excluded from the study. The institution's ethics committee approved the study, and the patients were required to give informed consent.
21 cemented implants were included in each group. The PS group consisted of 15 knees of patients with rheumatoid arthritis and 6 knees of patients with osteoarthrosis. The MB group consisted of 14 knees of patients with rheumatoid arthritis and 7 knees of patients with osteoarthrosis. The two groups were similar with regard to age (66, SD 12 years), body mass index (27, SD 5 kg per square meter), or stage of osteoarthrosis: Ahlbäck 4, (min-max: 3–4) and Larsen 4, (min-max: 3–5) (Ahlbäck 1968, Larsen et al. 1977).
We used the Interax posterior stabilized TKP (Stryker-Howmedica, Rutherford, NJ) and the Interax integrated secure asymmetric (ISA) TKP, an MB design (). The Interax system provides a tibiofemoral articulation surface of the femoral prosthesis, which is spherically shaped in both the frontal and sagittal planes. The baseplate of the Interax system is manufactured from cast vitallium and has a highly polished surface. The articulating surface used in both designs is made of ultra-high-density-molecular-weight polyethylene (UHMWP). The PS design has a fixed articulating surface, with a central cam providing medial-lateral stability.
The knee prosthesis with the MB insert permits anterior/posterior sliding and rotation of the inlay on the tibial tray. Two metal pins guide movement of the inlay on the tibial tray, which match the profile of a corresponding groove on the underside of the inlay. Movement of the MB insert is guided by this metal pin, which matches the profile of a corresponding groove on the underside of the inlay. The maximum possible movement of the center of the inlay is 8.5 mm (anterior/posterior) with 18° of axial rotation relative to the tibial tray.
During the knee arthroplasty, 6 to 8 tantalum markers (1 mm diameter; Industrial Techtonics, Ann Arbor, MI) were inserted with a specialized instrument into the tibial metaphysis of each patient. The manufacturer inserted two 1-mm diameter tantalum markers into a polyethylene wing, which was rigidly connected between the tibial baseplate and the stem. A third implant marker was attached at the tip of the stem in a polyethylene notch.
A patellar component made of UHMWP was used in all knees. The operation was performed through a standard midline incision with a medial arthrotomy. Ligament tensioning and balancing of the MB knee group was standardized during surgery using the Monogram Knee Balancer (Stryker-Howmedica). After soft-tissue release, the prosthesis was implanted according to the manufacturer's instructions. During surgery, the stability of each PS knee was assessed in extension and 90° of flexion. Discrepancies of less than 2 mm were accepted after medial and lateral stressing of the knee.
The cut bone surfaces were mechanically pulse-lavaged with a device manufactured by Zimmer (Warsaw, IN) before Palacos bone cement (Schering, Kenilworth, NJ) was applied. The tibial base-plate and the central stem were cemented in all patients. Postoperatively, all of the knees were fitted with a Jones bandage.
The patients were evaluated preoperatively and at 1 week, 3 weeks, 6 weeks, 3 months, 6 months, 1 year, and 2 years postoperatively. At each evaluation, the clinical status was assessed and radio-graphs for RSA were exposed. Immediately after the operation, and at the 1-year and the 2-year follow-up, standard anterior/posterior exposures were taken with the patient standing (Ewald Citation1989). Lateral radiographs and also axial radiographs of the patella were made supine. The femoral tibial angle was determined based on a preoperative and 1-year hip-knee-ankle radiograph. 2 patients (1 PS and 1 MB) were lost to follow-up before the final follow-up evaluation of the study, due to severe mobility restrictions unrelated to the knee prosthesis (severe rheumatoid arthritis with multiple joint involvement).
The RSA set-up consisted of two synchronized X-ray tubes positioned approximately 1.5 m above an X-ray cassette (35 × 43 cm) at a 20° angle to the vertical. Both X-ray tubes exposed the film simultaneously. A calibration box made of Perspex was used to define the three-dimensional (laboratory) coordinate system. For this purpose, 26 1-mm tantalum markers were positioned in the lower plane of the box (fiducial markers). In order to calculate the focus position, 16 1-mm tantalum markers were positioned in the upper plane of the box (control markers).
Using a Vidar VXR-12 scanner (Vidar, Lund, Sweden), the radiographs were scanned at a resolution of 150 dots per inch and 8-bit gray-scale resolution. The measurement of marker coordinates in the digitized radiographs, the three-dimensional reconstruction of the marker positions, and the micromotion analysis were done with RSA-CMS (MEDIS, Leiden, the Netherlands). This software package performs the RSA procedure automatically using digitized or digital radiographs (Vrooman et al. Citation1998, Valstar et al. Citation2000, Valstar Citation2001).
In order to assess the micromotion of the implant with a high degree of accuracy, the bone markers must be well fixated in the bone. Bone markers were defined as being unstable when they moved more than 0.3 mm with respect to the other bone markers. Unstable markers were excluded from the analysis automatically.
The first RSA examination served as the reference baseline. All subsequent evaluations of micromotion were related to the relative position of the prosthesis with respect to the bone at the time of the evaluation. Micromotion of the components was expressed as translation of the center of gravity of the prosthesis markers and rotation of the rigid body was defined by the prosthesis markers about this center of gravity. Positive directions for translations along the orthogonal axes were: transverse (medial-lateral), longitudinal (caudal-cranial), and sagittal (posterioranterior). Positive directions for rotations about the coordinate axes were anterior tilt (transverse axis), internal rotation (longitudinal axis), and varus (sagittal axis).
The reproducibility of the RSA measurements was determined by means of double examination of a subgroup of patients (). Double examination consists of 2 RSA examinations of the same patient, exposed within a time interval of about 10 min. Because of the short time interval between these two radiographs, the assumption is made that the implant did not migrate relative to the surrounding bone between these two exposures. By measuring, analyzing, and comparing the two radiographs, the accuracy of the micromotion parameters could be assessed (Ranstam et al. Citation2000).
Table 1. Precision of the RSA measurements based on double examinations. The numbers presented are the upper limits of the 95% confidence interval (translations n = 22; rotations n = 16)
Statistics
Mean values and standard deviations were calculated for all variables. For comparison of the median values of the two groups, MannWhitney U-test was used. This test was used to compare the micromotion data between the two types of bearing designs at the 2 year follow-up. Levene's test was used to determine whether the group variances for the micromotion were equal. For all analyses, significance was assumed with a p-value ≤ 0.05.
Results
Clinical results
There were no significant differences between the two groups in the preoperative Hospital for Special Surgery score (HSS), Knee score and Functional score according to the system of the Knee Society (), or at the 2-year follow-up evaluation. The mean preoperative flexion of both groups was 111° (SD 16; range 80–135), which increased to 116° (SD 13; range 90–140) at the 2-year follow-up evaluation. The medio-lateral instability scores, based on the Knee Society system, are presented in .
Table 2. HSS, Knee Society scores and Functional scores (mean, SD) pre-operatively, and at the 6-month, 1 year and 2-year follow-up for the MB knee group (n = 21) and PS knee group (n = 21)
Table 3. Mediolateral instability according to the system of the Knee Society. Number of patients scored preoperatively and postoperatively
1 patient from the MB group (RA treated with corticosteroids and methotrexate) developed skin necrosis with secondary patella tendon necrosis and deep infection. After removal of the prosthesis, debridement and treatment with antibiotics, an arthrodesis was performed.
Radiographic results
Routine radiographs of the knee revealed no radio-lucent lines of 2 mm or more around the tibial, femoral or patellar component in either of the 2 groups at the 2-year follow-up evaluation. In 2 knees from the MB group and 3 knees from the PS group, non-progressive radiolucent lines of 1 mm were observed in the first two medial zones of the anterior-posterior radiographs. In 1 PS knee, the lateral radiograph revealed a radiolucent line of 1 mm in the posterior zone, and in another PS knee a radiolucent line of 1 mm in the anterior zone was discovered.
We found no significant differences in the radio-graphic results between the MB and PS groups. For the two groups, the mean preoperative femoral-tibial angle was 181° (SD 8.4; range 152–192). At the postoperative evaluation the mean flexion contracture for the MB group was 1.3° (SD 3.3; range 5–10) compared to 0.0° (SD 3.3; range -5–10) for the PS group. At the 2-year follow-up evaluation, the femoral-tibial angle was 178° (SD 3.2; range 176–186). 4 MB knee prostheses and 1 PS prosthesis had a varus deformity of more than 3° at the two-year follow-up evaluation ().
Table 4. Radiographic results (mean (SD)) for the MB (n = 21) and PS (n = 21) tibial components at the 2-year follow-up evaluation
RSA results
The micromotion data for the tibial components is presented in and . In some cases, problems occurred regarding the marking of the tibia. In 3 cases (2 MB, 1 PS), the bone was either marked with less than 3 markers, or the markers were positioned so that they were occluded by the component. These cases were excluded from the analysis. In 9 components (6 PS, 3 MB) one of the markers, either at the medial side or the lateral side of the tibial tray, was occluded. As a result, only the translations of these specific tibial components could be calculated ().
Table 5. Mean translations (95% CI, lower bound – upper bound) of the PS and MB tibial components during the 2-year follow-up
Table 6. Mean rotations (95% CI, lower bound – upper bound) of the PS and MB tibial components during the 2-year follow-up
Table 7. Number of observations that could be used for calculation of migration for each follow-up examination
No significant differences in translations and rotations were found between the MB group and the PS group. At the 2-year follow-up evaluation, the PS components had subsided by 0.10 (SD 0.18; range -0.01–0.59) mm, and the mobile bearing components had subsided by 0.06 (SD 0.09; range -0.01–0.20) mm. The mean anterior-posterior tilting of the component at two-year follow-up was –0.09° (SD 0.27; range -0.39–0.35) for MB components, and the equivalent figure for the PS components was –0.06° (SD 0.86; range -1.42–1.75). 6 patients had a rotation of more than 0.30° about this axis. 3 of these patients also had the highest body mass index (BMI) of the PS group. The PS group showed a higher variability in subsidence (Levene's test, p = 0.04) and rotation about the transverse axis (Levene's test, p = 0.05) compared to the MB group. This indicates that some PS components showed a relatively high micromotion (e.g. maximum anterior tilt or posterior tilt) compared to the components in the MB group.
All tibial components with radiolucent lines of 1 mm rotated about the longitudinal axis by 0.4° or more. Components without radiolucent lines rotated less than this.
Discussion
Wear causes aseptic loosening of the prosthesis due to the osteolytic activity around it, induced by wear particles and fluid pressure (Schmalzried et al. Citation1992, Santavirta et al. Citation1993, Vis Citation1997). Because of the relatively small contact area of fixed bearing designs, the contact stresses in the polyethylene can be high, leading to excessive wear. The contact Wear causes aseptic loosening of the prosthesis due to the osteolytic activity around it, induced by wear particles and fluid pressure (Schmalzried et al. Citation1992, Santavirta et al. Citation1993, Vis Citation1997). Because of the relatively small contact area of fixed bearing designs, the contact stresses in the polyethylene can be high, leading to excessive wear. The contact pressure on the posterior part of the tibial tray increases rapidly during flexion, especially for patients with a high BMI. This is due to a posterior translation of the femoral-tibial contact point (Stiehl et al. Citation1999), which would explain the anterior- posterior tilting of the component observed in this study (Stukenborg et al. Citation2002). However, in MB designs wear can also be seen between the polyethylene bearing and the tibial tray. The mechanical solutions proposed to restrict bearing motion to a unidirectional motion by rotating platforms or entrapment of meniscal bearings in curved tracks (Lewandowski et al. Citation1997) may induce erratic movements, with impingement of polyethylene on metal. A prerequisite for a good load distribution in mobile bearing knees is a continuous motion of the polyethylene insert during flexion. However, the mobile bearing may be encapsulated by soft tissue after a period of time or may undergo erratic movements (Hartford et al. Citation2001). Consequently, the advantage of the mobility of the polyethylene insert—which should prevent excessive wear—is cancelled out, and could induce even more wear.
In cam-post articulation of PS implants, an additional source of polyethylene wear debris is present. The stabilizing cam acts as a contact guide in limiting tibial subluxation and in ensuring appropriate femoral rollback. Thus, the greatest amount of polyethylene wear will occur over the posterior surface of the post (Li et al. Citation1999).
Preoperative function and general condition of the patient are important factors in determining the postoperative function after TKA (Nelissen et al. 1999). The preoperative function score was only slightly higher for the MB group than for the PS group. Although the Knee Society function score was higher for the MB group at the beginning of the follow-up, no differences were observed at the two-year evaluation.
Nelissen et al. (Citation1998) showed a subsidence rate of –0.05 mm ± 0.11 mm after two-years of cemented fixed-bearing tibial components of the Interax total knee prosthesis, which is comparable to the subsidence in the results of the MB prostheses (0.08 mm ± 0.09 mm). In the former study, a low-conformity posterior cruciate retaining TKP was used, allowing more rotation than the Interax PS design. A low conformity design and also a higher conformity MB design apparently give less variability in the subsidence data than the PS design (Nelissen et al. Citation1998).
Three clinical factors might explain the variability in the micromotion between the two groups: the bone-cement interface, ligament balancing and alignment of the components. A good bone-cement interface implies a stable cemented prosthesis. Interface motion stresses the bone/cement, which will induce loosening of the prosthesis. The variability in the tilting of the components was especially large for the PS knees. In high flexion, the posterior cam of the femoral component slides against the polyethylene post and pushes the tibial component into an anterior tilt. Inducible displacements caused by this cam-post mechanism lead to increased interface motion (Uvehammer and Kärrholm Citation2001).
The second clinical factor causing variability in TKP micromotion data is improper ligament balancing. Some knees may be more lax in extension and tight in flexion, causing high contact pressures posterior to the tibial tray or at the cam-post contact point (Uvehammer and Kärrholm, Citation2001). Patients with a flexion contracture stress the posterior part of the tibial tray continuously, resulting in a rotation of the component about the transverse axis (i.e. anterior tilt of the tibial tray). However, in this study no significant difference in flexion contracture was noted between groups. Finally, post-operative collateral mediolateral stability scores were similar when comparing the MB and the PS knee prostheses. However, for MB prostheses, load inequality between the medial and lateral condyles resulting from an adduction moment during gait (Schipplein and Andriacchi Citation1991, Yu et al. Citation1997) or improper balancing of the knee (Vedi et al. Citation1999) is expected to be less at the tibial component, due to the mobility of the bearing. If alignment can be restored to normal anatomy, load sharing gives positive remodeling at the bone level (Wolff's Law) and at the soft tissue level (Roux's Law) (Malone et al. Citation2002). Appropriate tensioning of the soft tissues will not only enhance stress distribution, thus reducing bone-implant interface stresses, but will also provide appropriate knee stability and improved function. There is a low margin of error allowed during surgery. Even small errors could result in increased wear due to high contact stresses, and could undermine the theoretical benefits of prosthesis designs. The mobile bearing design is more forgiving, by correcting slight rotation differences between the actual anatomy and the TKP, but also compensating for slight rotation differences between the femoral and tibial components.
A third clinical factor affecting micromotion is alignment of the TKP. Residual varus deformity following TKP has been shown to create a substantial load imbalance, resulting in the type of stress that eventually leads to loosening of the tibial component (Schipplien and Andriacchi Citation1991, Stiehl et al. Citation1999, Perillo-Marcone et al. Citation2000). In a finite element analysis, the contact stresses in a 3° varus knee increased by 45% in comparison to a neutral alignment of the component (Liau et al. Citation2002). In the MB group, 4 prostheses had a varus deformity of more than 3°. These components may be at risk of experiencing high contact stresses in the medial compartment of the bearing, resulting in abnormal kinematics and a high degree of polyethylene wear. However, no increased micromotion (i.e. rotation of the tibial component about the sagittal axis) was found in these prostheses during the two-year follow-up. Stresses are dissipated away through the movable insert of the MB design.
We found no evidence of periprosthetic osteolysis on the plain radiographs when defining 2 mm of radiolucency as a radiographical indication of loosening (Pilliar et al. Citation1986, Søballe et al. Citation1993, Reading et al. Citation1999). When traditional radiographs are used for assessment, the rate of early loosening is underestimated. The PS components with a partial radiolucency of 1 mm also showed a substantial degree of rotation about the longitudinal axis (i.e. external rotation). Rotations about this axis are difficult to discriminate in traditional radiographs. The rotations about the longitudinal axis of the PS components can be explained by the femoral component bouncing against the cam during flexion. This cam prevents internal and external rotation of the tibia during flexion or walking (Lafortune et al. Citation1992). Puloski et al. (Citation2001) observed surface damage on the tibial posts of PS tibial components caused by cam-post articulation. Damage on the tibial posts will result in long-term failure of the PS knee prostheses through excessive wear, delamination, or may even lead to fatigue fracture of the tibial component.
The low variability of the data in the MB knee prosthesis group suggests that implantation of an MB design is more predictable and forgiving with respect to micromotion of the tibia component in the bone after two-year follow-up, compared to fixed-bearing PS designs.
Financial support for conducting this study was received from Stryker-Howmedica. The company was not otherwise involved in the study.
- Aglietti P, Buzzi R, De Felice R, Giron F. The Insall-Burstein total knee replacement in osteoarthritis: a 10-year minimum follow-up. J Arthroplasty 1999; 14: 560–5
- Ahlback S. Osteoarthrosis of the knee. A radiographic investigation. Acta Radiol Diagn (Stockh) 1968, (Suppl 72)
- Bartel D L, Bicknell V L. , Wright T M. The effect of Conformity, thickness, and material on stresses in ultra- high molecular weight components for total joint replacement. J Bone Joint Surg (Am) 1986; 68: 1041–51
- Buechel F F, Pappas M J. Long-term survivorship analysis of cruciate-sparing versus cruciate- sacrificing knee prostheses using meniscal bearings. Clin Orthop 1990, 260: 162–9
- Callaghan J J, Insall J N, Greenwald A S, Dennis D, Komistek R D, Murray D, Bourne R B, Rorabeck C H, Dorr L D. Mobile-bearing knee replacement: concepts and results. Instr Course Lect 2001; 50: 431–49
- Collier J P, Mayor M B, McNamara J L, Surprenant V A, Jensen R E. Analysis of the failure of 122 polyethylene inserts from uncemented tibial knee components. Clin Orthop 1991, 273: 232–42
- Ewald F C. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop 1989, 248: 9–12
- Goodfellow J, O'Connor J. The anterior cruciate ligament in knee arthroplasty. A risk-factor with unconstrained meniscal prostheses. Clin Orthop 1992, 276: 245–52
- Grewal R, Rimmer M G, Freeman M A. Early migration of prostheses related to long-term survivorship. Comparison of tibial components in knee replacement. J Bone Joint Surg (Br) 1992; 74(2)239–42
- Hartford J M, Hunt T, Kaufer H. Low contact stress mobile bearing total knee arthroplasty: results at 5 to 13 years. J Arthroplasty 2001; 16: 977–8
- Jones V C, Barton D C, Fitzpatrick D P, Auger D D, Stone M H, Fisher J. An experimental model of tibial counterface polyethylene wear in mobile bearing knees: the influence of design and kinematics. Biomed Mater Eng 1999; 9: 189–96
- Jordan L R, Olivo J L, Voorhorst P E. Survivorship analysis of cementless meniscal bearing total knee arthroplasty. Clin Orthop 1997, 338: 119–23
- Kärrholm J, Borssen B, Lowenhielm G, Snorrason F. Does early micromotion of femoral stem prostheses matter? 4–7-year stereoradiographic follow-up of 84 cemented prostheses. J Bone Joint Surg (Br) 1994; 76: 912–7
- Lafortune M A, Cavanagh P R, Sommer H J, III, Kalenak A. Three-dimensional kinematics of the human knee during walking. J Biomech 1992; 25: 347–57
- Larsen A, Dale K, Eek M. Radiographic evaluation of rheumatoid arthritis and related conditions by standard reference films. Acta Radiol Diagn (Stockh) 1977; 18: 481–91
- Lewandowski P J, Askew M J, Lin D F, Hurst F W, Melby A. Kinematics of posterior cruciate ligament-retaining and -sacrificing mobile bearing total knee arthroplasties. An in vitro comparison of the New Jersey LCS meniscal bearing and rotating platform prostheses. J Arthroplasty 1997; 12: 777–84
- Li P L, Zamora J, Bentley G. The results at ten years of the Insall-Burstein II total knee replacement. Clinical, radiological and survivorship studies. J Bone Joint Surg (Br) 1999; 81: 647–53
- Liau J J, Cheng C K, Huang C H, Lo W H. The effect of malalignment on stresses in polyethylene component of total knee prostheses. A finite element analysis. Clin Biomech. Avon, Bristol 2002; 17: 140–6
- Malone T R, Mc Poil T G, Nitz A J. Orthopaedic and sports physical therapy. Mosby, St. Louis, MO 2002
- Nelissen R G H H. Fundamental aspects of the clinical evaluation of total joint prostheses. The total condylar knee prosthesis. Leiden 1995, Thesis Groen
- Nelissen R G, Valstar E R, Rozing P M. The effect of hydroxyapatite on the micromotion of total knee prostheses. A prospective, randomized, double-blind study. J Bone Joint Surg (Am) 1998; 80: 1665–72
- Perillo-Marcone A, Barrett D S, Taylor M. The importance of tibial alignment: finite element analysis of tibial malalignment. J Arthroplasty 2000; 15: 1020–7
- Pilliar R M, Lee J M, Maniatopoulos C. Observations on the effect of movement on bone ingrowth into porous- surfaced implants. Clin Orthop 1986, 208: 108–13
- Puloski S K, McCalden R W, MacDonald S J, Rorabeck C H, Bourne R B. Tibial post wear in posterior stabilized total knee arthroplasty. An unrecognized source of polyethylene debris. J Bone Joint Surg (Am) 2001; 83: 390–7
- Ranstam J, Ryd L, Onsten I. Accurate accuracy assessment: review of basic principles. Acta Orthop Scand 2000; 71: 106–8
- Reading A D, McCaskie A W, Gregg P J. The inadequacy of standard radiographs in detecting flaws in the cement mantle. J Bone Joint Surg (Br) 1999; 81: 167–70
- Ryd L, Albrektsson B E, Carlsson L, Dansgard F, Herberts P, Lindstrand A, Regner L, Toksvig-Larsen S. Roentgen stereophotogrammetric analysis as a predictor of mechanical loosening of knee prostheses. J Bone Joint Surg (Br) 1995; 77: 377–83
- Santavirta S, Nordstrom D, Metsarinne K, Konttinen Y T. Biocompatibility of polyethylene and host response to loosening of cementless total hip replacement. Clin Orthop 1993, 297: 100–10
- Schipplein O D, Andriacchi T P. Interaction between active and passive knee stabilizers during level walking. J Orthop Res 1991; 9: 113–9
- Schmalzried T P, Jasty M, Harris W H. Periprosthetic bone loss in total hip arthroplasty. Polyethylene wear debris and the concept of the effective joint space. J Bone Joint Surg (Am) 1992; 74: 849–63
- Selvik G. Roentgen stereophotogrammetry. A method for the study of the kinematics of the skeletal system. Acta Orthop Scand, 1989: 1–51, (Suppl 232)
- Søballe K, Hansen E S, Brockstedt-Rasmussen H, Bunger C. Hydroxyapatite coating converts fibrous tissue to bone around loaded implants. J Bone Joint Surg (Br) 1993; 75: 270–8
- Stern S H, Insall J N. Posterior stabilized prosthesis. Results after follow-up of nine to twelve years. J Bone Joint Surg (Am) 1992; 74: 980–6
- Stiehl J B, Dennis D A, Komistek R D, Crane H S. In vivo determination of condylar lift-off and screw-home in a mobile-bearing total knee arthroplasty. J Arthroplasty 1999; 14: 293–9
- Stukenborg-Colsman C, Ostermeier S, Wenger K H, Wirth C J. Relative motion of a mobile bearing inlay after total knee arthroplasty. Dynamic in vitro study. Clin Biomech. Avon, Bristol 2002; 17: 49–55
- Uvehammer J, Kärrholm J. Inducible displacements of cemented tibial components during weight- bearing and knee extension observations during dynamic radiostere-ometry related to joint positions and 2 years history of migration in 16 TKR. J Orthop Res 2001; 19: 1168–77
- Valstar E R. Digital Roentgen Stereophotogrammetry. Development, validation, and clinical application. Leiden University, Den Haag 2001, Thesis
- Valstar E R, Vrooman H A, Toksvig-Larsen S, Ryd L, Nelissen R G. Digital automated RSA compared to manually operated RSA. J Biomech 2000; 33: 593–9
- Vedi V, Williams A, Tennant S J, Spouse E, Hunt D M, Gedroyc W M. Meniscal movement. An invivo study using dynamic MRI. J Bone Joint Surg (Br) 1999; 81: 37–41
- Vis H M. Wear, particles, and physical factors in loosening of hip prostheses. University of Amsterdam, the Netherlands 1997, Thesis
- Vrooman H A, Valstar E R, Brand G J, Admiraal D R, Rozing P M, Reiber J H. Fast and accurate automated measurements in digitized stereophotogrammetric radiographs. J Biomech 1998; 31: 491–8
- Wright T M, Rimnac C M, Stulberg S D, Mintz L, Tsao A K, Klein R W, McCrae C. Wear of polyethylene in total joint replacements. Observations from retrieved PCA knee implants. Clin Orthop 1992, 276: 126–34
- Yu B, Stuart M J, Kienbacher T, Growney E S, An K N. Valgus-varus motion of the knee in normal level walking and stair climbing. jClin Biomech. Avon, Bristol 1997; 12: 286–93