Abstract
Background: Computerized dynamic posturography (CDP) is the gold standard to differentiate between sensory, motor, and central adaptive impairments to postural control.
Objective: To obtain normative values in healthy adults age 20–69 for a CDP system that uses a full-field dynamic visual surround. This is in contrast to the mechanically movable visual surround used in traditional CDP systems.
Methods: Fifty healthy adults divided into five age groups were tested during the three test protocols for CDP: sensory organization test (SOT), motor control test (MCT), and adaptation test (ADT). Outcomes were compared across age groups and to published normative CDP values. Repeatability was assessed in five different subjects (23–30 years old) on 2 days, 1 week apart.
Results: Most outcomes were comparable to published norms with notable differences in SOT condition 4 and ADT. SOT composite and conditions 4–6, all MCT translations, and ADT toes up showed moderate to good repeatability (r = 0.60 to 0.99). Age group and gender differences were not substantial.
Conclusions: Some but not all CDP outcomes with a virtual visual environment were comparable to published norms. The differences are likely related to the virtual surround having a more compelling effect on balance even in conditions with a stationary surround.
Chinese abstract
背景:电脑动态姿势成像(CDP)是区分感觉、运动和中枢适应性障碍与姿势控制的黄金标准。
目标:为使用全视野动态视觉环境的CDP系统而获得20-69岁健康成年人的规范值。这与传统CDP系统中使用的可机械移动的视觉环境形成对比。
方法:50名健康成人分为5个年龄组, 在CDP的三项测试方案中进行测试:感觉组织测试(SOT)、运动控制测试(MCT)和适应测试(ADT)。比较不同年龄段的结果和公布规范性CDP值。对5位不同的受试者(23-30岁)进行重复性评估, 每次评估两天, 之间相隔1周。
结果:大部分结果与已发表的规范相当, 仅SOT条件4和ADT显示显著差异。 SOT复合性和条件4-6, 所有的MCT翻译和ADT脚趾向上显示中度到良好的重复性(r = 0 .60到0.99)。年龄组的和性别上的差异并不大。
结论:一些但不是所有的虚拟视觉环境的CDP结果与已发表的规范相当。这种差异可能与虚拟环境有关, 这种虚拟环境对平衡具有更强的作用, 即使在静止环境的条件下也是如此。
Introduction
Balance is a critical, yet underappreciated and complex part of everyday life. It is defined as the ability to control upright posture under different conditions, and the ability of an individual to sense their limitations of stability. Deficits in balance increase a person’s risk for falls and can lead to serious consequences such as hip fractures, hospitalization, and even death [Citation1]. Various methods have been introduced in order to measure balance; however, common tests used in the clinic are not always consistent due to their variable execution and subjective scoring systems [Citation2].
In the 1980s, computerized dynamic posturography (CDP) devices, such as the Equitest (NeuroCom, a Division of Natus, Clackamas, OR) were developed using sway referencing of the surface and surround as a way to manipulate the environment. By coupling the movement of the surround and/or surface with the person’s sway, proprioception and/or visual information becomes inaccurate, forcing the subject to select another sensory input to maintain postural control. CDP soon gained wide acceptance as a method of measuring postural control in patients with a variety of diagnoses affecting the vestibular system including traumatic brain injury, multiple sclerosis, peripheral vestibular disorders, post-concussion, and vestibular dysfunction in the elderly [Citation3–8]. For this reason, many clinicians still consider the Equitest as the gold-standard CDP device for identifying balance impairments in adults [Citation9–11].
More recently, with the advances in technology, the Bertec Balance Advantage (Bertec Incorporated, Columbus, OH) CDP device has become available. This system utilizes a stationary spherical dome as the visual surround. A series of concentric ovals are projected on the dome, creating the perception of a tunnel with no definable end or horizon. The computer interactive display technology of Bertec, as opposed to a mechanically moveable surround, creates a full-field dynamic visual surround (FFDVS) for the subject, therefore creating an illusion of self-motion and postural responses [Citation12]. Unlike the traditional system, the FFDVS provides full-field immersion without reference points.
Normative values across age groups are available for the NeuroCom Equitest CDP protocol. It is composed of three test protocols, the sensory organization test (SOT), the motor control test (MCT), and the adaptation test (ADT). Due to the Bertec’s platform differing from NeuroCom by using a virtual environment, it is unknown if the values between the two devices are comparable. Furthermore, no normative data have been reported using the Bertec. Therefore, the purpose of this study is to report results on the CDP for healthy adults aged 20–69 using the Bertec CDP system and determine if these results are comparable to what has been established using the NeuroCom platform. A secondary purpose of this study was to ascertain repeatability in a smaller sample of five young adults (23–30 years old) on the Bertec when retested 1 week later.
Method
Subjects
We recruited 50 subjects (17 males; 33 females) who met our inclusion criteria using non-probability quota sampling. Subjects were recruited through flyers, social media, and word of mouth and stratified into five age groups, 10 subjects per group: 20–29, 30–39, 40–49, 50–59, and 60–69 years of age.
The study was approved by the California State University, Fresno, Committee on Protection of Human Subjects and informed consent was obtained from each person prior to testing. Subjects filled out a questionnaire to ensure they met the following criteria: (1) able to stand for more than 20 min, (2) independent walking, (3) no neurological or musculoskeletal impairment impacting balance, (4) no balance or vestibular disorder, (5) no history of head or cervical neck injury, (6) no visual impairment worse than 20/40 with glasses, (7) no concussion with symptoms within the past 10 years, (8) no diabetes or peripheral vascular disease, (9) no lower extremity joint disorder, (10) no current complaints of motion sickness/sensitivity, and (11) no symptoms of dizziness, impaired balance or light-headedness with prescribed medications.
Procedure
Three tests were conducted on the Bertec Dynamic CDP platform, the SOT, the MCT, and the ADT. To reduce error, the same tester was used to conduct all three examinations.
Subjects stood on the platform with bare feet while the researcher aligned their medial malleolus into the standardized position, parallel to the horizontal line on the forceplate. The lateral calcaneus of each foot was then aligned to the small, medium, or large lines, according to the manufacturer’s instructions. Subjects wore an overhead harness to prevent falls but did not limit sway. Detailed explanations of each test or trial was provided to each participant from a standardized script prior to beginning any test.
The SOT was the first test performed using the manufacturer’s standard protocol. The SOT consists of six sensory conditions, with three trials per condition, each trial lasting 20 s. An equilibrium score ranging from 0% to 100%, with 100% indicating perfect stability and 0% indicating a fall was calculated for each trial. The equilibrium score for each condition is the average of three trials. Conditions 1–3 were conducted with a fixed base of support (BoS) with eyes open, eyes closed, and eyes open with a sway-referenced virtual visual environment. Conditions 4–6 were performed with a sway-referenced mobile BoS with eyes open, eyes closed, and eyes open with a sway-referenced virtual environment.
The MCT, performed next, measures the subject’s ability to recover from unexpected external provocations. The test used sequences of small, medium, or large platform translations, scaled to the subject’s height, in either the forward or backward direction, with only the medium and large translations used for calculating test results. Three trials of each translation were performed. The time in msec (latency) between the onset of the translation and the force response in the subject’s legs was recorded for each trial.
The ADT, performed last, measures a subject’s ability to adapt and sustain proper balance with minimal sway when exposed to five equivalent surface irregularities. This is measured by the amount of anterior–posterior sway after a toes up and toes down perturbation, referred to as sway energy. For each trial, a sway energy score quantifies the force magnitude required to overcome the postural instability.
A previous study [Citation13] noted a learning effect on repeated CDP tests using the Equitest. To investigate this learning effect with the virtual reality-based CDP, we retested five subjects aged 23–30 years 7 days later on the SOT, MCT, and ADT.
Statistical analysis
Data analyses were completed using SPSS Version 25 (Chicago, IL). Equilibrium scores were the average of three trials for each of the six conditions on the SOT. The SOT composite score is a weighted average of the six conditions with greater weight given to the more difficult conditions.
Latency scores for three trials are averaged during right and left medium and large translations during the MCT. ADT trials were averaged during toes up and toes down measures. Individual ADT trials were used when comparing to NeuroCom norms. Statistical significance of p ≤ .05 was set for all analyses.
Results for the retest study were analyzed using a Pearson’s r correlation coefficient. We defined r values of less than 0.5 having poor reliability, 0.50–0.75 as having moderate reliability, and greater than 0.75 as having good reliability.
A two-way analysis of variance (ANOVA) was used to compare the five age groups and gender for the SOT, MCT, and ADT. If significance was found, a post-hoc Tukey’s HSD was conducted to determine which groups were different.
A one-way t-test was used to compare the mean Bertec scores in our sample, to the reported NeuroCom mean values for each of the three measures. The published NeuroCom norms are grouped into 20–59 years old, 60–69 years old, and 70–79 years old. None of our subjects were in the 70- to 79-year-old age group. Thus, we separated the 60- to 69-year-old group to create a 20–59 years old (n = 40) and 60–69 years old (n = 10) age group for comparisons. Right and left sides were averaged together to be consistent with the NeuroCom normative values on the MCT. Individual ADT trials were used for analysis in order to compare to their NeuroCom normative values.
Results
Subjects
Fifty-six subjects were recruited, however 4/6 were excluded for musculoskeletal impairments and 2/6 due to residual post-concussion symptoms. Of the 50 eligible subjects, 17/50 reported visual impairments all corrected with glasses. 10/50 reported previous motion sickness sometime during their life, however, it was not considered significant to interfere with testing if they no longer experienced symptoms. 23/50 subjects reported a prior lower extremity injury and/or surgical intervention including stress fracture, knee arthroscopy, hysterectomy, caesarean section, and appendectomy; however, they were not considered significant. 18/50 subjects reported use of over the counter and/or prescription drugs. Subjects ranged from taking 0 to 4 medications. Prescription medications included bronchodilators, antacids, thyroid medications, statins, antihypertensive medications, diuretics and hormone medicines. Dosages and medication time lines were unknown, however, it was considered not significant to interfere with testing as most were over the counter type medications. There were no reports of dizziness or impaired balance symptoms prior or during testing.
Comparison between age groups and gender
When age group and gender were compared using a two-way ANOVA, there was no interaction between gender and age group. However, there was a statistically significant main effect for gender in three of the variables. Males had a greater mean equilibrium score during condition 3 compared to females (p = .042, mean diff 2.0 equilibrium score); longer MCT latency score for the backward medium translation (p = .009, mean diff 6.2 msec); and greater sway energy score on the ADT toes up test (p = .002, mean diff 13.4 sway energy score). No other gender differences were found.
Only condition 2 (p = .033) and the corresponding somatosensory ratio score (p = .013) on the SOT, large forward translation on the MCT (p = .035) and toes down on the ADT (p = .025) revealed differences between age group means. Using post-hoc tests, the equilibrium score for condition 2 on the SOT was higher in 20–29 years old as compared to 50–59 years old (p = .037, mean diff 2.5 equilibrium score), whereas the 20–29 years old had a longer latency on the large forward translation as compared to 30–39 years old (p = .037, mean diff 12.3 msec). The 20–29 years old had lower mean scores during the toes down test as compared to both 50–59 years old (p = .048, mean diff 23.08 sway energy score) and 60–69 years old (p = .029, mean diff 24.7 sway energy score). All other age group mean comparisons were not significant ().
Table 1. Mean ± SD for SOT equilibrium and ratio scores, MCT latencies (msec), and ADT averaged sway energy scores for all age groups.
Comparison to NeuroCom normative values
The assumption of normality was tested for all variables using the Shapiro–Wilk test. All variables for the 50- to 59-year-old age group had a normal distribution. All but two SOT variables (conditions 1 and 3) and ADT toes down trials in the 20- to 59-year-old age group met the criteria.
A one-way t-test revealed significant differences between the two CDPs, on condition 1 (p = .003), 4 (p = .0001), 6 (p = .0052), and SOT composite scores (p = .0001) in the 20- to 69-year-old age group (, ). Only condition 4 was significantly different in the 60- to 69-year-old age group (p = .0001) (). Large backward and medium forward translation latencies on the MCT were significantly different (p = .0038 and .0001) in the 20–59 years old (, ), whereas none of the latencies were significant in the 60–69 years old (). Trials 3–5 on the Bertec were significantly greater (p = .0004, .0001, .0001, respectively) for toes up on the ADT in 20–59 years old (, ), whereas all five trials were significantly greater (p = .0042, .0001, .0002, .0002, .0001, respectively) for 60–69 years old as compared to the NeuroCom norms (). Trials 2–5 on the Bertec were significantly greater (p = .0244 to p = .0001) for toes down on the ADT in both age groups as compared to NeuroCom norms ( and , ).
Figure 1. Comparing sensory organization test (SOT) equilibrium scores on Bertec to NeuroCom published norms for 20–59 years old. All SOT equilibrium scores on the Bertec were comparable to the reported NeuroCom norms with the exception of condition 4 (mean EQL score diff =10, p = .0001). Although other conditions had statistical significance (asterisk indicates p < .05) the mean difference was less than 8 points and therefore not considered clinically relevant. Similar results occurred for 60–69 years old (not shown).
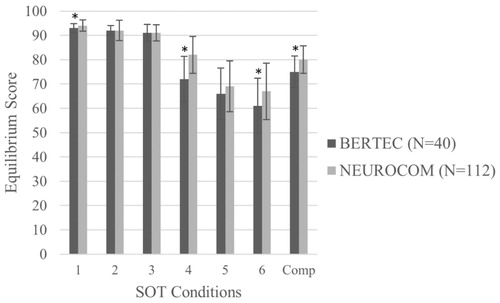
Figure 2. Comparing latencies during each of the translations during the motor control test (MCT) on Bertec to NeuroCom published norms for 20–59 years old. Although statistical significance (asterisk indicates p < .05) occurred in some translations, all differences in latency between CDP systems were within 10 msec and therefore not considered clinically relevant. There were no differences in latencies between Bertec and NeuroCom published norms for 60–69 years old (not shown).
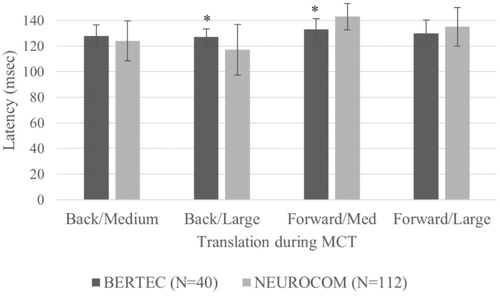
Figure 3. Comparing sway energy scores during each of the five trials during toes up and toes down adaptation test on Bertec to NeuroCom published norms for 20–59 years old. Asterisk indicates statistical significance at p < .05. Similar results occurred in the 60–69 years old (not shown).
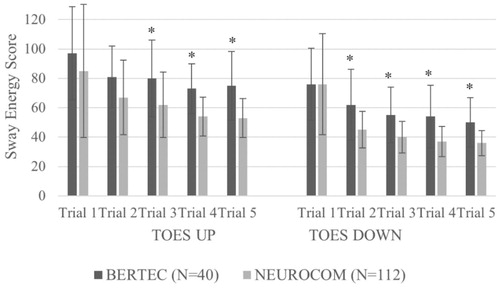
Table 2. Comparison of 20–59 years old on NeuroCom compared to Bertec for the SOT, MCT, and ADT.
Table 3. Comparison of 60–69 years old on NeuroCom compared to Bertec for the SOT, MCT, and ADT.
Retest study
When comparing the outcomes in the subset of the five different subjects who underwent a second testing 1 week later, the Pearson’s correlation coefficient for SOT conditions 1–6 and composite score were r = 0.24, 0.10, 0.33, 0.89, 0.76, 0.99, 0.98, respectively. MCT tests demonstrated correlation coefficients of r = 0.60 to r = 0.95 for individual medium, large, forward and backward latencies and r = 0.95 for the composite score. The ADT scores for the toes up condition (5 trials averaged) had a correlation coefficient of r = 0.71 and for the toes down condition (five trials averaged) r = 0.04.
Discussion
This is one of the first studies to report normative values using the Bertec CDP platform.
Age and gender differences
Many studies have reported a decline in SOT and MCT scores with aging using the NeuroCom [Citation14,Citation15], however, these studies had larger group sample sizes with a greater age span as compared to this study. A sample size of 10 per age group was not sufficient to demonstrate differences in this study. The 60–69 age group showed improved scores in stability when compared to the 50–59 age group, yet reported more visual impairments (70% vs. 20%), more surgeries (70% vs. 30%), more experiences of motion sickness (50% vs. 10%), and more joint problems (10% vs. 0%). Although we did not ask about lifestyle, it is possible subjects in the oldest group participated in more activities that address balance, as studies have demonstrated these can have positive effects on balance [Citation16–18].
We were unable to determine if gender influenced CDP in our sample of healthy adults. The uneven distribution of males and females in each age group and the overall group (33 females and 17 males) is a limitation of this study. Although three of the variables showed a statistically significant difference between males and females, the actual mean differences were small (2 points on the SOT equilibrium score in condition 3, 6.2 msec difference in MCT latency, and 13.4 points on the averaged sway energy score during the ADT toes up test) and therefore not considered substantial. Other studies have shown gender differences for some balance measures in older adults [Citation19] as opposed to young adults [Citation15].
Comparison to NeuroCom norms
The data for the SOT and MCT on the Bertec indicate comparable values to the NeuroCom system. The one exception was condition 4 on the SOT. The differences found in conditions 1, 6 and composite SOT were minor (1, 6, and 5 points, respectively, in the 20–59 years old) and not clinically relevant as the scores were less than the learning effect of 8 points reported by Wrisley et al. [Citation13] on the NeuroCom. In contrast, condition 4 on the Bertec were 10 and 15 points lower in the 20–59 years old and 60–69 years old as compared to the NeuroCom norms ( and , ). The virtual surround in the Bertec is an immersive virtual environment with no compensatory visual strategy available during condition 4. In contrast, individuals assessed in the NeuroCom can reference to the horizon and images in the scene. The Bertec, therefore, may be more sensitive in assessing visual capabilities for balance.
When comparing the Bertec’s MCT means to the NeuroCom norms, the differences are negligible, never exceeding 10 msec. Bertec samples at 1000 Hz as compared to NeuroCom at 100 Hz. The latency for the MCT on the Bertec is within 5 msec, whereas the NeuroCom system samples at a 10 msec resolution. Differences are less than 10 msec between the two systems, therefore, they should be considered comparable ( and , ).
When comparing the ADT means on the Bertec to the NeuroCom norms, the intended trend of more stability with each trial is noted for both toes up and toes down series ( and , ). However, individuals on the Bertec displayed higher average sway energy scores compared to NeuroCom norms. This could be explained by the increased difficulty in the Bertec dome. In addition, ADT is the least reliable of the three posturography tests and demonstrated the greatest variability as indicated by the large SDs ( and , ). Furthermore, the results of the ADT test can be influenced by subjects that have problems that are unrelated to balance such as fear, anxiety, and biomechanical factors. More research is needed to determine the significance of this finding. The toes up ADT test has been implicated in certain diagnoses, as well as risk for falls [Citation20]. Therefore, it would be important to conduct studies using the Bertec Balance Advantage in a patient population.
Retest study
There was moderate to good repeatability 1 week apart for all measures with the exception of SOT conditions 1 and 2 and ADT toes down test in our sample of five young adults. The most reliable conditions of the SOT were the ones that are the most difficult. This difference is most likely due to the learning effect reported by others, which is most significant between the first and second SOT tests [Citation13]. Larger studies are needed to determine the cause of these findings.
Conclusions
When compared to NeuroCom published norms, the largest mean differences occurred on SOT condition 4. In the ADT tests, subjects showed less stability on the Bertec. SOT composite, conditions 1–3 and 5–6, and MCT tests are comparable to NeuroCom normative values. Although both devices provide different visual conflicts depending on the surround there are no significant differences between devices in assessing vestibular cues for balance. Further research with patient populations is needed to determine the significance of lower equilibrium scores during condition 4 on the Bertec as compared to NeuroCom norms.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Kannus P, Parkkari J, Koskinen S, et al. Fall-induced injuries and deaths among older adults. JAMA. 1999;281:1895–1899.
- Mancini M, Horak FB. The relevance of clinical balance assessment tools to differentiate balance deficits. Eur J Phys Rehabil Med. 2010;46:239–248.
- Shumway-Cook A, Olmscheid R. A systems analysis of postural dyscontrol in traumatically brain-injured patients. J Head Trauma Rehabil. 1990;4:1–62.
- Nelson SR, Di Fabio RP, Anderson JH. Vestibular and sensory interaction deficits assessed by dynamic platform posturography in patients with multiple sclerosis. Ann Otol Rhinol Laryngol. 1995;104:62–68.
- Oda DTM, Gananca CF. Computerized dynamic posturography in the assessment of body balance in individuals with vestibular dysfunction. Audiol Commun Res. 2015;20:89–95.
- Mirka A, Black FO. Clinical application of dynamic posturography for evaluating sensory integration and vestibular dysfunction. Neurol Clin. 1990;8:351–359.
- Guskiewicz KM. Assessment of postural stability following sport-related concussion. Curr Sports Med Rep. 2003;2:24–30.
- Norre ME, Forrez G, Beckers A. Posturography measuring instability in vestibular dysfunction in the elderly. Age Ageing. 1987;16:89–93.
- Ionescu E, Dubreuil C, Ferber-Viart CC. Physiological changes in balance control of adults aged 20 to 60 years assessed with Equitest. Ann Otolaryngol Chir Cervicofac. 2005;122:231–235.
- Dodd K, Hill K, Haas R, et al. Retest reliability of dynamic balance during standing in older people after surgical treatment of hip fracture. Physiother Res Int. 2003;8:93–100.
- Furman JM. Posturography: uses and limitations. Baillieres Clin Neurol. 1994;3:501–513.
- Thurrell AE, Bronstein AM. Vection increases the magnitude and accuracy of visually evoked postural responses. Exp Brain Res. 2002;147:558–560.
- Wrisley DM, Stephens MJ, Mosley S, et al. Learning effects of repetitive administrations of the sensory organization test in healthy young adults. Arch Phys Med Rehabil. 2007;88:1049–1054.
- Lockhart TE, Smith JL, Woldstad JC. Effects of aging on the biomechanics of slips and falls. Hum Factors. 2005;47:708–729.
- Faraldo-Garcia A, Santos-Perez S, Crujeiras-Casais R, et al. Influence of age and gender in the sensory analysis of balance control. Eur Arch Otorhinolaryngol. 2012;269:673–677.
- Douris P, Southard V, Varga C, et al. The effect of land and aquatic exercise on balance scores in older adults. J Geriatr Phys Ther. 2003;26:3–6.
- Schmid AA, Van Puymbroeck M, Koceja DM. Effect of a 12-week yoga intervention on fear of falling and balance in older adults: a pilot study. Arch Phys Med Rehabil. 2010;91:576–583.
- Jeter PE, Nkodo AF, Moonaz SH, et al. A systematic review of yoga for balance in a healthy population. J Altern Complement Med. 2014;20:221–232.
- Wolfson L, Whipple R, Derby CA, et al. Gender differences in the balance of healthy elderly as demonstrated by dynamic posturography. J Gerontol. 1994;49:M160–M167.
- Paquette C, Franzen E, Horak F. More falls in cerebellar ataxia when standing on a slow up-moving tilt of the support surface. Cerebellum. 2016;15:336–342.
